Neuromuscular diseases (NMDs) are one of the largest groups of hereditary diseases, characterized by dysfunction of voluntary muscles, decrease or loss of control of movements. The occurrence of these diseases is caused by a defect in embryonic development or a genetically determined pathology.
A characteristic manifestation of hereditary neuromuscular diseases is ataxia - a disorder of motor coordination and impaired motor skills. With static ataxia, balance is impaired while standing, with dynamic ataxia, coordination during movement is impaired.
The following symptoms are characteristic of neuromuscular diseases: weakness, muscle atrophy, spontaneous muscle twitching, spasms, numbness, etc. If neuromuscular connections are disrupted, patients may experience drooping eyelids, double vision, and a number of other manifestations of muscle weakening, which only intensify during the day. In some cases, disturbances in swallowing function and breathing are possible.
Classification of neuromuscular diseases
Neuromuscular diseases can be classified into four main groups depending on location:
- muscles;
- neuromuscular endings;
- peripheral nerves;
- motor neuron.
Based on the type and type of violations, they are divided into the following main groups:
- primary progressive muscular dystrophies (myopathies);
- secondary progressive muscular dystrophies;
- congenital non-progressive myopathies;
- myotonia;
- hereditary paroxysmal myoplegia.
Congenital myopathies in children
Neuromuscular diseases can be hereditary, autoimmune and metochondrial.
1. Thomsen's myotonia is inherited and manifests itself in early childhood. The first sign is a swallowing disorder (slow swallowing, frequent vomiting), which occurs due to high tone of the pharyngeal muscles. Over time, the inability to unclench fingers clenched into a fist and difficulty in starting to walk occurs. Only muscle strength, due to the tone of skeletal, and not smooth muscles, does not suffer.
2. In muscular dystrophy, the muscle fibers themselves are damaged. The following symptoms are typical for muscle weakness in a child:
- muscle weakness;
- decreased muscle tone;
- children's lag in motor development;
- atrophy (“drying”) of muscles or a false increase in muscle volume due to their replacement with adipose tissue;
- skeletal deformities.
3. In case of amyotrophy, the nerve fibers of the spinal cord or the nerves themselves are affected. Already from birth you can notice in a child:
- lethargy (frog pose);
- slowdown in motor development (the child begins to hold his head up late, sit up, walk);
- "duck" gait;
- “wing-shaped” shoulder blades;
- “wasp” waist;
- increase in muscle volume (“athlete’s body”).
Myopathy
The term myopathy (myodystrophy) unites a fairly large group of diseases that are united by a common feature: primary damage to muscle tissue. The development of myopathy can be triggered by various factors: heredity, viral infection, metabolic disorders and a number of others.
Inflammatory myopathies (myositis) include diseases caused by the inflammatory process. They develop as a result of autoimmune disorders and may be accompanied by other diseases of a similar nature. These are deramtomysitis, polymyositis, myositis with various inclusions.
Mitochondrial myopathies. The cause of the disease is structural or biochemical mitochondria. This type of disease includes:
- Kearns-Sayre syndrome;
- mitochondrial encephalomyopathy;
- myoclonus epilepsy with “torn red fibers.”
In addition to these diseases, there are a number of rare types of myopathies that affect the central core, endocrine system, etc.
When active, myopathy can lead to disability and further immobilization of the patient.
Secondary progressive muscular dystrophies
The disease is associated with disruption of the functioning of peripheral nerves, disruption of the supply of organs and tissues with nerve cells. As a result, muscle dystrophy occurs.
There are three types of secondary progressive muscular dystrophy: congenital, early childhood and late. In each case, the disease proceeds with a greater or lesser degree of aggression. For people with this diagnosis, the average life expectancy is from 9 to 30 years.
Congenital muscular dystrophies and structural myopathies
Congenital (congenital) myopathies are a group of genetically determined myopathies characterized by early onset (usually from birth to 1 year), a characteristic symptom complex (floppy child syndrome) and a non-progressive or slowly progressive course. Among congenital myopathies, congenital muscular dystrophies and congenital myopathies (structural myopathies) are distinguished.
CLINICAL PICTURE
Most congenital myopathies and dystrophies are manifested by the “flaccid child” syndrome. Clinical manifestations of the “floppy child” syndrome are reduced to severe muscle hypotonia, weak muscle resistance during passive movements, head incontinence, delayed motor development, and joint hypermobility. “Floppy child” syndrome is also observed in spinal muscular atrophy and other congenital diseases of the central nervous system, metabolic diseases (glycogenosis, aminoaciduria), etc. Approximately 80% of cases of “floppy child” syndrome are caused by primary damage to the central nervous system. The main method for diagnosing congenital myopathies is a morphological study of muscles; EMG only confirms the primary muscular nature of the lesion at the initial stage of differential diagnosis. Along with the “flaccid child” syndrome, weakness of the facial muscles, trunk muscles and respiratory muscles is noted. The majority develop contractures of the hip, knee and elbow joints, neck extensor muscles, scoliosis, and later external ophthalmoplegia may develop. Despite delayed motor development, most children are able to sit independently, some can walk independently (with partial merosin deficiency). EMG reveals the primary muscle type of changes, while the spontaneous activity of muscle fibers is either absent or insignificant.
SYMPTOMS
For Fukuyama congenital muscular dystrophy, severe muscle weakness is typical (children are either not able to walk independently at all, or begin to walk only at the age of 2-8 years), symptomatic epilepsy (in 50%), mental retardation, ophthalmological pathology (microphthalmia, retinal hypoplasia, cataracts). , myopia, strabismus). Multiple and varied changes on MRI are characteristic (dysplasia, agyria, ventricular dilatation, cysts). Ullrich congenital muscular dystrophy, in addition to the “floppy child” syndrome, is characterized by kyphosis, hypermobility of the distal joints, hip dysplasia, and hyperkeratosis. The ability to walk independently depends on the severity of the disease, but by the age of 2-10 years, as a rule, it is lost due to severe contractures. Walker-Warburg syndrome is one of the most severe congenital neuromuscular diseases (average life expectancy is 9 months). Numerous congenital anomalies are observed: meningocele, agyria, agenesis of the corpus callosum, pyramidal tract hypoplasia, ventricular enlargement, microcephaly, microphthalmia, optic nerve hypoplasia, cataracts, glaucoma and other changes leading to blindness, “floppy child” syndrome and bulbar disorders.
TREATMENT
Treatment should be carried out exclusively by a neurologist. Self-medication is unacceptable. There is no specific therapy; the goal of treatment is the correction of orthopedic disorders (hip dysplasia, scoliosis), prevention of contractures, maintenance of muscle strength, treatment of cardiomyopathy and symptomatic epilepsy.
Congenital non-progressive myopathies
These include hereditary non-progressive or weakly progressive muscle diseases diagnosed in the prenatal period or immediately after the birth of the baby. The main symptom is muscle hypotonia with pronounced weakness. This disease is otherwise called “flaccid child syndrome,” which accurately characterizes its condition.
In most cases, the area of the lower extremities is affected, less often - the upper extremities; in exceptional cases, damage to the cranial muscles occurs - impaired facial expressions and eye movements.
During the development and growth of a child, problems with motor skills are noted; children often fall, begin to sit and walk late, and cannot run or jump. There are no intellectual impairments. Unfortunately, this type of myopathy is incurable.
Symptoms
For all types of myopathies, the main symptom is muscle weakness. Most often, the muscles of the shoulder girdle, hips, pelvic area, and shoulders are affected. Each type is characterized by damage to a specific muscle group, which is important to consider when diagnosing. The defeat occurs symmetrically, so he is able to carry out actions in stages, gradually including various areas in the work.
If the legs and pelvic area are affected, in order to get up from the floor, you must first lean your hands on the floor, kneel down, grab a support, and after that the patient can sit on a chair or bed. He will not be able to stand up on his own without using his hands.
With myopathy, cases of damage to the facial muscles are the least common. This is ptosis (drooping of the upper eyelid), the upper lip droops. Speech problems arise due to impaired articulation, and swallowing function may be impaired.
Most myopathies occur with almost identical symptoms. Over time, muscle tissue atrophies, against the background of which connective tissue actively grows. Visually it looks like trained muscles - the so-called. pseudohypertrophy. In the joints themselves, contractures form and the muscle-tendon fiber tightens. As a result, pain appears and joint mobility is limited.
Myoplegia
Like myopathies, these are hereditary neuromuscular diseases characterized by attacks of muscle weakness or paralysis of the limbs. The following types of myoplegia are distinguished:
- hypokalemic;
- hyperkalemic;
- normokalemic.
An attack of myoplegia is caused by a redistribution of potassium in the body - there is a sharp decrease in it in the intercellular fluid and plasma, and an increase (excess) in the cells. In muscle cells, membrane polarization is disrupted and the electrolytic properties of muscles change. During an attack, the patient experiences severe weakness of the limbs or torso, manifestations in the pharynx, larynx, and effects on the respiratory tract are possible. This can be fatal.
Myasthenia gravis
The disease most often affects women (2/3 of the total number of patients). Myasthenia has two forms - congenital and acquired. With this disease, the transmission of nerve impulses is disrupted, resulting in weakness in the striated muscles.
The disease is associated with changes in the functions of the neuromuscular system. Weakening muscles affect the normal functioning of organs: the patient may have constantly half-closed eyelids, difficulty urinating, and difficulties in chewing and walking. As a result, the disease can lead to disability and even death.
Differences between diseases
Hereditary diseases of the nervous system differ in the timing of the onset of the first symptoms, the rate of development and duration of the disease, the manifestations that arise and the degree of their severity. In addition, different diseases have varying degrees of resistance to treatment. The difference in the manifestations of these diseases is primarily due to genetic polymorphism, that is, the fact that the same disease is caused by hundreds of different mutations occurring in one part of the gene. Moreover, in some patients, two different pathological changes are combined in the hereditary material in one gene region. In addition to environmental influences, genes are modified by other genes called modifier genes.
Clinical Brain Institute Rating: 2/5 — 1 votes
Share article on social networks
Motor Neurone Diseases (MND)
Motor neuron diseases are characterized by damage to the motor neurons of the brain and spinal cord. The gradual death of cells affects muscle function: they gradually weaken, and the affected area increases.
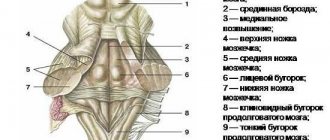
The brain neurons responsible for movement are located in the cerebral cortex. Their branches - axons - descend into the spinal cord, where contact occurs with the neurons of this department. This process is called synapse. As a result, a neuron in the brain releases a special chemical (transmitter) that transmits a signal to neurons in the spinal cord. These signals are responsible for the contraction of muscles in various parts: cervical, thoracic, bulbar, lumbar.
Depending on the severity of neuronal damage and their localization, several types of BND are distinguished. In many ways, the manifestations of the diseases are the same, but as the disease progresses, the difference becomes more and more significant.
There are several different types of BND:
Amyotrophic lateral sclerosis
It is one of the four main types of motor neuron disease. It occurs in 85% of patients diagnosed with motor neuron disease. The affected area can be both neurons of the brain and spinal cord. As a result, muscle atrophy and spasticity occur.
With ALS, there is weakness and increasing fatigue in the limbs. Some people have weakness in their legs when walking and weakness in their arms, making it difficult to hold things in their hands.
In most cases, the disease is diagnosed before the age of 40, and the disease does not affect the intellect at all. The prognosis for a patient diagnosed with ALS is not the most favorable - from 2 to 5 years. But there are exceptions: the most famous person of all, who lived with this diagnosis for more than 50 years, is Professor Stephen Hawking.
Progressive bulbar palsy
Associated with speech and swallowing disorders. The prognosis from the date of diagnosis is up to three years from the date of diagnosis;
Primary literal sclerosis
Affects only the neurons of the brain and affects the lower extremities. In rare cases, it is accompanied by impaired hand movements or speech problems. In later stages it can progress to ALS.
Progressive muscular atrophy
Occurs when the motor neurons of the spinal cord are damaged. The first manifestations are expressed in hand weakness. The prognosis for this disease is from 5 to 10 years.
Primary muscular dystrophies (myopathies)
In genetic terms, myopathies are a heterogeneous group of diseases. Myopathies with an autosomal dominant type of inheritance, with an autosomal recessive and sex-linked type of inheritance are observed.
Pseudohypertrophic form of Duchenne. This is the most common form of sex-linked myopathy. Boys are sick. The disease begins in the first five years of a child's life. Clinically manifested by atrophy of the muscles of the pelvic girdle and proximal legs. Pseudohypertrophy appears early, especially in the gastrocnemius and, less commonly, deltoid muscles, terminal muscle atrophy, retraction of the tendons, especially the Achilles, and reflexes disappear, especially in the knee. It is difficult for a child to climb stairs, he rests his hands on his hips, cannot jump, and has great difficulty getting up from the floor. After some time, weakness and atrophy of the muscles of the shoulder girdle sets in, and soon the child becomes bedridden. Subsequently, contractures develop due to sharp retraction of the tendons, and the foot assumes the position of a horse.
With this form of myopathy, changes are noted in the heart muscle, and the brain suffers to one degree or another, which is manifested by the mental retardation of the child. Due to weakness of the respiratory muscles and poor ventilation of the lungs, these children often develop pneumonia, aggravated by weakness of the heart muscle, from which patients usually die early. All this indicates the pleiotropic influence of the pathological gene. In 1955, Becker described a mild variant of sex-linked myopathy that bears his name. The disease begins after the age of 20 years. It manifests itself as pseudohypertrophy of the calf muscles and slowly developing atrophies of the muscles of the pelvic girdle and thighs. Intelligence does not suffer in this form. These two forms of the disease are determined by damage to two different genes located in two loci of the sex X chromosome, i.e. they are genocopies. Both forms of myopathy do not occur in the same family.
The Erb form is inherited in an autosomal recessive manner. It is found in three variants - early, typical and late. Of these, the most common is the typical, youthful variant. Patients, usually in the second decade of life, develop weakness of the muscles of the pelvic girdle and proximal lower extremities, and then their atrophy. Subsequently, the muscles of the shoulder girdle and proximal arms are involved in the process. Pseudohypertrophies in this form are minor and rare. The gait and static behavior of patients are changed, although less than in the Duchenne form. When rising, the patient leans on surrounding objects (74). Due to the weakness of the long back muscles, gluteal and abdominal muscles, lordosis increases and the gait resembles a duck's. Due to weakness of the serratus anterior muscles, pterygoid blades appear. Due to atrophy of the trapezius muscle, the symptom of “loose shoulders” occurs. You can take the patient by the shoulders and freely lift the shoulder girdle up. In this case, the head seems to sink between the shoulder blades. Of the abdominal muscles, the rectus and oblique muscles atrophy more and the transverse ones remain, as a result of which the waist of patients is very thin (“wasp waist”). The orbicularis oris and orbicularis oculi muscles are affected early. As a result, the patient cannot purse his lips into a tube, cannot whistle, when laughing, the corners of the mouth do not rise upward, and the oral fissure stretches to the sides (transverse smile). Due to pseudohypertrophy, the lips protrude (tapir lips). The long muscles of the limbs atrophy not only in diameter, but also at the ends (end atrophy), resulting in muscle tuberosity. As a result of muscle atrophy and shortening, active and passive movements in the joints are limited. Due to weakness of the muscles and ligaments, tendon reflexes are reduced or absent, and “looseness” of the joints is noted. Over the years, body weight increases, especially the subcutaneous fat layer develops, muscles atrophy more and more, which leads to a sharp limitation of active movements and subsequently to complete immobility of patients. Males and females are affected, but the former are more common. The earlier the disease begins, the more malignant it becomes. In the later version, the course is more favorable. Patients can walk and care for themselves for a long time. There are cases of stopping the progression of the disease for some time. Landouzy-Dejerine scapulohumeral-facial form. This is the mildest form of the disease. Inherited in an autosomal dominant manner. It begins at the age of 15-20 years, progresses very slowly and has little effect on the ability of patients to work. The disease begins with weakness and atrophy of the muscles of the shoulder blades, and later spreads to the facial muscles. The patient’s face is poor in facial expressions, without wrinkles—“myopathic” (75). They have wing-shaped shoulder blades; due to weakness of the muscles of the shoulder girdle, patients are not able to raise their arms above the horizontal level. In women, the disease is more severe than in men. The disease does not affect mental abilities. Such patients may have children, half of whom are also predisposed to developing this form of myopathy. Other forms of myopathy are much less common. Among them, ophthalmoplegic, distal, and congenital forms are distinguished.
Diagnostics
To establish an accurate diagnosis, it is important to conduct the following studies:
- biochemical. Determination of muscle enzymes, primarily creatine phosphokinase (CPK). The level of myoglobin and aldolase is determined;
- electrophysiological. Electromyography (EMG) and electroneuromyography (ENMG) help in differentiating between primary and secondary myopathy. They also help to identify whether the spinal cord or peripheral nerve is primarily affected;
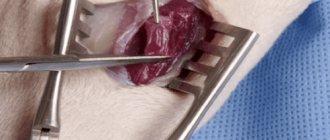
- pathomorphological. Consists of performing a muscle biopsy. Studying the material also helps to differentiate primary or secondary myopathy. Determining the level of dystrophin makes it possible to distinguish Duchenne myopathy from Becker myodystrophy, which is important for prescribing the correct treatment;
- DNA diagnostics. The study of DNA leukocytes allows us to identify hereditary diseases in 70% of patients.
Treatment of neuromuscular diseases
When one of the diagnoses related to neuromuscular diseases is made, in each specific case the treatment is selected individually, taking into account all the tests obtained. The patient and his relatives must initially understand that this is a long and very complex process that requires large financial costs.
Difficulties in prescribing treatment are also associated with the fact that it is not always possible to accurately determine the primary metabolic defect. At the same time, the disease is constantly progressing, which means that treatment should primarily be aimed at slowing the progression of the disease. This will help preserve the patient’s ability to self-care and affect his quality of life.
Treatment methods for neuromuscular diseases
- Correction of skeletal muscle metabolism. Drugs that stimulate metabolism, potassium supplements, vitamin complexes, and anabolic steroids are prescribed;
- Stimulation of the segmental apparatus. Neurostimulation, myostimulation, reflexology, balneotherapy, physical therapy (exercises and load are selected individually);
- Correction of blood flow. Various types of massage, thermal procedures on certain areas, oxygen barotherapy;
- Diet and parenteral nutrition to provide the body with all the necessary nutrients - protein, potassium salts, vitamins of the required group;
- Corrective sessions with an orthopedist. Correction of contractures, deformities of the chest and spine, etc.
Today, no medicine has been invented that can make any person absolutely healthy in an instant. Despite the complexity of the situation, it is important for a patient with a neuromuscular disease to continue to live the best possible quality of life. The example of Hawking, who was confined to a wheelchair for more than 50 years but continued to conduct research, suggests that illness is not a reason to give up.
Diagnosis and treatment of muscle diseases
Therapy for neuromuscular diseases depends on proper diagnosis. It can be medication, physiotherapy, vitamin therapy, exercise therapy, etc. With the development of joint contractures and spinal deformities, orthopedic correction is used.
An integrated approach to the treatment of children with muscle weakness slows down the progression of the disease.
To treat neuromuscular diseases, drugs that improve the metabolism of nervous muscle tissue, anabolic steroids, drugs that improve neuromuscular conduction, etc. are used. Drug therapy is prescribed by the attending physician.
Prevention of muscle disease in the unborn child is carried out during medical and genetic counseling of parents at the stages of family planning. Thus, the risks of developing hereditary diseases, including muscle pathologies, are assessed.