Pinchuk Elena Anatolyevna
Deputy chief physician for medical work, kmn, neurologist, doctor of physical and rehabilitation medicine
Kritskaya Olga Pavlovna
Neurologist, highest category
Maltseva Marina Arnoldovna
Neurologist, specialist in the field of extrapyramidal pathologies, doctor of the highest category
Shabunina Ekaterina Mikhailovna
Neurologist, category 2
Stroke is an acute disorder of cerebral circulation resulting from damage to the vascular wall. A stroke can be ischemic - as a result of occlusion of a cerebral artery, or hemorrhagic - due to a rupture of the vessel wall or an aneurysm.
Most often, hemorrhagic stroke occurs with damage to the middle cerebral artery and has a characteristic clinical picture with a number of typical symptoms.
Symptoms and signs
When an acute cerebrovascular accident occurs, various symptoms appear, which are divided into general and pathognomonic. Common stroke symptoms include:
- Severe headache;
- Nausea and vomiting that does not bring relief;
- Noise in ears;
- Sweating and dry mouth;
- Cardiopalmus.
All of the above symptoms can occur with a variety of diseases, but when there are 2 or more common symptoms, you should consult a neurologist.
For a stroke involving the middle cerebral artery, there are a number of pathognomonic symptoms, i.e. those that are diagnostically significant for stroke.
Topical diagnostics allows you to accurately determine the location of thrombosis or rupture of the middle cerebral artery and determine the extent of brain damage. Characteristic symptoms:
- Paresis and paralysis on the opposite side of the body from the affected hemisphere;
- Impaired coordination and orientation in space;
- Cognitive impairments including the perception of speech and visual information, loss of various types of memory.
Cerebral infarction in the left cma
Introduction
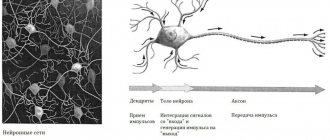
The clinical picture of left hemisphere strokes is characterized by speech disorders, among which the most significant is aphasia. Aphasia, which manifests itself acutely, indicates a circulatory disorder in the middle cerebral artery (MCA) [1]. Speech processes, as a rule, exhibit a significant degree of lateralization and in most people depend on the leading (dominant) hemisphere [2]. It must be taken into account that in determining the dominant hemisphere responsible for speech, the approach that associates dominance only with right-handedness or left-handedness is simplified. The profile of the distribution of functions between the hemispheres is usually diverse [2, 3], which is reflected in the degree of speech disorders and the possibilities of speech restoration [4]. Many people exhibit only partial and unequal hemispheric dominance for different functions [2]. While speech function in right-handers (≥90%) and most left-handers (>50%) is predominantly associated with the left hemisphere [1,4], there are three exceptions to this rule: 1. Less than 50% of left-handers have speech function associated with the right hemisphere. 2. Anomic (amnestic) aphasia can occur with metabolic disorders and volumetric processes in the brain. 3. Aphasia may be associated with damage to the left thalamus [1]. The so-called crossed aphasia (aphasia caused by a cerebral lesion ipsilateral to the dominant hand) is currently attributed only to right-handers [4]. The area of the cortex responsible for speech function is located around the Sylvian and Rollandian fissures (SMA basin). Speech production is determined by four zones of this area, closely interconnected and located sequentially along the posteroanterior axis: Wernicke's area (posterior part of the superior temporal gyrus), angular gyrus, arcuate fasciculus (AF) and Broca's area (posterior part of the inferior frontal gyrus) (Fig. 1, 2) [1].
The DP is a subcortical white matter fiber that connects Broca's area and Wernicke's area. There is evidence that in the left hemisphere DP occurs in 100% of cases, while in the right hemisphere – only in 55% [5]. A number of researchers believe that there are several pathways involved in ensuring speech function [6, 7]. Other authors have received reliable confirmation only of the role of DP [8]. The pathogenesis of dysarthric speech disorders is determined by focal brain lesions of different locations. Complex forms of dysarthria are often observed [9]. Purpose of the study:
to study the relationship between the volume of brain damage in stroke in the left MCA and the degree of speech impairment.
Material and methods
Over a 4-month period, 356 people were admitted to the emergency room of the City Hospital No. 5 with suspected stroke. All patients were examined by a neurologist in the hospital emergency room, the neurological deficit was assessed, and the presence/absence of speech disorders was reflected. Subsequently, if the patients’ condition allowed, they underwent speech therapy examination, in most cases, the day after admission to the hospital. In 124 cases (every third patient) a preliminary diagnosis was made: stroke in the territory of the left middle cerebral artery (MCCA). This localization is most relevant when studying aphasia in patients with stroke. All patients upon admission and most patients over time underwent a CT scan of the brain (Bright Speed 16 tomograph) to confirm/exclude focal brain lesions and clarify the extent of the lesion and the location of the pathological area. According to the results of CT scan of the brain, 32 (25.8%) people out of 124 revealed typical ischemic changes in the LMCA basin, of which 7 were examined dynamically, i.e., upon admission, the changes were not yet obvious (initial stage of stroke). In 5 (4.0%) cases, hemorrhages were detected: left-sided medial hematomas and 1 case of subarachnoid hemorrhage (SAH). In 5 (4.0%) cases out of 124, infarctions of other localization (not in the LSMA basin) were detected (Table 1).
In 22 (17.7%) cases, according to CT scans of the brain, no infarction was detected in the area of interest, but the patients were hospitalized in the primary neurological department for patients with stroke, because they had significant neurological symptoms: atrophy of the brain substance , vascular focal changes, vascular leukoaraiosis, post-infarction cysts. This group also includes patients whose symptoms were caused by a transient ischemic attack. In 60 (48.4%) cases, patients were not hospitalized. In most cases, stroke was not confirmed (there were no corresponding changes in CT data or in the neurological status). The number of patients not hospitalized in the acute stroke department also included patients with various types of atrophy of the brain substance in combination with significant neurological symptoms who refused the proposed hospitalization. A few patients were transferred to other hospitals because they were diagnosed with traumatic changes in the skull, brain, and tumors. Some patients were transferred to the on-duty neurology department of another hospital, for example, with a diagnosis of osteochondrosis. 64 patients hospitalized in the acute stroke department with stroke had speech impairments (Table 2). The detailed nature of speech disorders was determined by a speech therapist. In 20 (31.2%) cases, patients were diagnosed with dysarthria and absence of aphasia. In 2 cases, dysarthria was accompanied by dysphonia and dysphagia. Aphasia was detected in 44 (68.8%) people, of which in 7 cases it regressed by the time of consultation with a speech therapist the next day (in 2 cases, ischemic infarctions were detected with regression of aphasia). 3 people from the group with sensorimotor aphasia had severe dysarthria, 9 people had dysphagia. In 4 people from the group with motor aphasia, symptoms of dysarthria were also noted, in 1 case - severe dysarthria.
Two left-handed patients, who were initially suspected of having a stroke in the left MCA, were diagnosed with a stroke in the right MCA based on the results of a CT scan of the brain. In one case there was aphasia, which regressed within 24 hours, in another case dysarthria was noted. In patients with dysarthria without aphasia, 4 types of dysarthria were identified: extrapyramidal (3 cases), afferent cortical (1 case), bulbar (1 case), pseudobulbar (8 cases), in other cases it was difficult to clearly determine the type of dysarthria, the manifestations were mild ( Table 3). In groups of patients with dysarthria and regression of aphasia within 24 hours, there is a slight predominance of men.
Aphasia is observed with lesions of the cerebral cortex. In one case, the cause of aphasia was damage to the subcortical structures of the left hemisphere (medial intracerebral hematoma in the thalamus (Fig. 3). Speech disorders in such cases do not correspond to any of the main types of aphasia. Damage to the subcortical structures can be suspected in cases where amnestic aphasia is combined with dysarthria or aphasia - with hemiparesis. This patient had a right-sided hemiparesis of 4 points.
Middle cerebral artery lesion
A stroke can have varying degrees of severity and it depends on the following factors. At what level did thrombosis or rupture of the vessel occur? If the lesion is at the level of the trunk of the middle cerebral artery, then the infarction will be extensive and will affect the entire hemisphere, including the structures of the cerebellum. The most common ischemic stroke of the middle cerebral artery occurs. When any of the branches of the middle cerebral artery is damaged, a milder course is observed, while fewer body functions are disrupted. Thrombosis or rupture of small arterioles is called a microstroke, and the patient may not even suspect any symptoms.
External manifestations
The cerebral hemispheres are supplied with blood by three large vessels. The anterior and middle cerebral arteries arise from the internal carotid. The posterior cerebral artery is a branch of the basilar artery, which is formed after the fusion of the vertebral vessels. Thus, the brain receives blood from two large arteries - the internal carotid and vertebral.
Clinical signs of ischemic stroke directly depend on which vessel the blood flow has stopped. The larger the area of the brain that is left without nutrition, the more pronounced the symptoms will be. Accordingly, the prognosis for the life and health of such a patient will be worse. When small branches are affected, the patient’s chances of surviving and fully recovering increase significantly. In such patients, the disease often resolves without consequences.
Treatment of arterial stroke
If the symptoms described above appear, you must immediately call an ambulance. The time from the onset of acute cerebrovascular accident to the development of irreversible processes of necrotization of the nervous tissue of the brain is 2-2.5 hours. The treatment approach varies for different types of stroke. In hemorrhagic stroke, it is important to promptly begin brain decompression therapy to avoid herniation of the brain stem into the foramen magnum, which is fatal. For this use:
- Antihypertensive drugs that lower blood pressure;
- Diuretics that cause diuresis and reduce the volume of circulating blood. If there is a large amount of bleeding and the hematoma grows, surgical intervention with craniotomy is required.
For ischemic stroke, the tactics are completely different. The patient is prescribed thrombolytic therapy aimed at eliminating thrombosis. In some cases, it is possible to use surgical intervention under X-ray control. Embolectomy and stenting of the affected arteries are performed, and blood flow is restored. The Ural Center for Resuscitation Neurorehabilitation offers high-quality services for the treatment and rehabilitation of even the most severe forms of stroke. Only correct diagnosis, comprehensive treatment and full rehabilitation can avoid serious consequences and complications after a stroke.
Diagnosis of acute cerebrovascular accident
To identify the etiology of stroke of ischemic type, the following diagnostic methods are necessary:
- Blood tests (electrolytes, hemostasis indicators, glucose, lipid spectrum, antiphospholipid antibodies).
- Electrocardiography, blood pressure measurement.
- Auscultation of vessels on the extremities, duplex scanning, transcranial Dopplerography of precerebral arteries.
| Hypoechoic atherosclerotic plaque in the distal part of the right common carotid artery in patient A., 48 years old. |
- Computed tomography (CT) of the brain shows a hypodense zone 12–24 hours after the development of an ischemic stroke. SPECT (at earlier stages of cerebral ischemia).
| CT scan of the brain of patient V., 75 years old, with a diagnosis of stroke of ischemic type in the MCA basin on the right: A) CT scan upon admission; B) CT scan on the third day. |
- Cerebral angiography (stenosis, occlusion, ulceration, aneurysm).
Differential diagnosis:
- Hemorrhagic stroke.
- Acute hypertensive encephalopathy.
- Dysmetabolic or toxic encephalopathy.
- Migraine stroke.
- Traumatic brain injury.
- The debut of multiple sclerosis.
Consequences of a stroke
The consequences largely depend on the degree and area of brain damage, the compensatory forces of the victim’s body and the quickly and correctly initiated treatment.
Most often, the patient becomes disabled as a result of developed paralysis of skeletal muscles and multiple contractures in the joints of the limbs. Persistent impairments in a person’s cognitive abilities can be corrected, but residual effects always remain in the form of memory loss, difficulties in perceiving information, and others. The degree of loss of function largely depends on the patient himself, his relatives and their correct attitude towards treatment and long, labor-intensive recovery after a stroke.
Clinical Brain Institute Rating: 2/5 — 4 votes
Share article on social networks
Recovery
The effect of the recovery process depends on the extent of the stroke, the age of the patient, and the start of rehabilitation.
Nutrition
You should give preference to healthy foods. The Mediterranean diet is a priority: limiting meat, increasing fish consumption, vegetables and a small amount of carbohydrates. Alcoholic products should be avoided in the first year after the attack.
Important! For diabetes mellitus, a low-carbohydrate diet is recommended to carefully control this pathology. It is patients with decompensated diabetes who are most often at risk of recurrent stroke.
Depending on the degree of damage
| Stroke severity | Duration and completeness of recovery |
| Stroke with minimal neurological deficit (mild paralysis of the limbs and face, dizziness, problems with coordination and vision) | After 1-2 months, full rehabilitation gives partial recovery; Completeness occurs closer to the 3rd month. |
| Stroke with persistent paralysis of the limbs and loss of coordination | Partial functions are restored after 6 months, full recovery lasts for years. There is still the possibility of lifelong loss of some skills. |
| Severe form of stroke (paralysis of one side and other neurological defects) | The ability to move independently in bed and sit appears after 1-2 years. Complete recovery is extremely rarely achieved. |
Physiotherapy
This rehabilitation method allows you to restore muscle activity, restore blood circulation, relieve spasm and painful tension in the affected limbs. Physiotherapy procedures are prescribed together with the attending physician and physiotherapist. They are selected taking into account possible contraindications. This can be magnetic therapy, laser, EMS, acupuncture.
Exercise therapy
Exercise therapy for stroke is developed by a specialist. The muscle tone on the affected limb is taken into account. It is necessary to dose the force with which the exercise is performed. Charging should be done daily. The work should affect all muscle groups (face, neck, shoulders, torso, lower limbs). An example complex can be found by following the link.
Work with the paralyzed side is carried out first in passive mode. A physical therapy specialist develops a paretic limb, repeating all normal movements. After independent tone and strength appear, it is necessary to load the arm and leg, allowing them to work.
Breathing exercises
This type of exercise is important for the prevention of congestive pneumonia. It must be performed while the patient is in bed. After this, breathing exercises are effective in restoring the reserves of the cardiovascular system.
A left-sided stroke is difficult for the patient and his family. Quick delivery of the patient to a medical facility and timely initiation of therapy can save a person’s life and improve the prognosis of rehabilitation.
Programs:
Assessment of rehabilitation potential
Movement restoration
Rehabilitation after stroke
Restoration of cognitive functions
Early (resuscitation) rehabilitation
General cerebral symptoms
Common symptoms of brain damage include:
- headache;
- nausea;
- vomit;
- dizziness;
- disturbance of consciousness.
In ischemic strokes, it is expressed rather weakly, often completely absent. The patient remains conscious, sometimes a disturbance such as stunning is possible. When large vessels are blocked - the middle cerebral or intracranial part of the internal carotid, when the process affects large areas and is accompanied by intense cerebral edema, a coma may develop. Due to secondary displacement and compression of the brain stem, the prognosis for the patient worsens significantly.
It is in the trunk that vital centers are located - respiratory and cardiovascular.
Squeezing them significantly reduces the chances of success, even with timely and properly organized treatment.
In addition, the patient may lose consciousness if blood circulation in the vertebrobasilar system is impaired. In this case, nausea, vomiting, intense dizziness, and hiccups may occur.
With the development of cerebral edema, the following disorders occur:
- disruption of the cardiovascular system;
- sharp fluctuations in blood pressure;
- arrhythmias;
- hyperthermia;
- convulsions;
- dysfunction of the respiratory system.
What factors determine the prognosis of the disease?
With correct treatment tactics, the main factor determining the prognosis for a patient with a stroke is the timeliness of treatment.
It depends on him what consequences await the patient in the future. Early seeking help allows blood flow to be restored in the affected vessels, due to which the activity of neurons is completely restored.
The prognosis of stroke largely depends on the adequacy of treatment
In the worst case, it is possible to restore nerve cells located in the ischemic penumbra zone, thus reducing the size of the lesion. Delaying the start of therapy has an extremely negative impact on the patient’s health.
Therapeutic measures
Therapy begins in the first hours after the onset of an attack. It is important to remember that the prognosis and severity of consequences depend on the timeliness of assistance provided.
- thrombolytics (Urokinase, Fibrinolysin) for resorption of formed blood clots;
- anticoagulants (Warfarin, Heparin), which reduce blood density and prevent recurrent thrombus formation;
- neuroprotectors (Nootropil) and antioxidants (Glycine, Mexidol) to reduce possible damage to brain cells;
- vasoactive agents (Actovegin, Cinnarizine) to improve cellular metabolism.
Regardless of which areas of the brain are affected, clinical stroke is almost always accompanied by arterial hypertension. To reduce and stabilize blood pressure, fast-acting drugs (Captopril, Clonidine) and long-term medications are used to prevent the development of crises (Lisinopril, Prestarium).
In the first days after an ischemic stroke in the left MCA or in other areas, the patient is provided with rest to prevent cerebral edema and prevent a recurrent ischemic attack.
After the person’s condition becomes stable, he is transferred to the general ward and, while continuing drug therapy, rehabilitation measures to restore impaired functions begin.
Features of ischemic stroke in stenosis of the internal carotid artery
In case of cerebral infarction, which is caused by severe stenosis in the extracranial part of the internal carotid artery on the left, the symptoms are: numbness or transient weakness of the limbs, decreased vision on the right and motor aphasia.
Read also: Ocular stroke
The causes of hemodynamically significant stenosis of the internal carotid artery are in most cases severe atherosclerosis of the main vessels of the head, therefore, in the clinic, as a rule, previous transient ischemic attacks are present and a systolic murmur is detected over the affected artery (on the left) and asymmetry of the pulsation of the carotid arteries.
According to the clinical course of this type of stroke, there is an apoplectic form, which is characterized by a sudden onset and resembles a hemorrhagic stroke, subacute and chronic forms (with a slow increase in symptoms).