Post-traumatic encephalopathy (ICD-10 - T90.5 and G93.8) is a specific brain disease that develops within a year after a traumatic brain injury.
A disease such as post-traumatic encephalopathy is not classified as chronic, but it can cause serious disruption of brain function and the appearance of symptoms that can not only significantly worsen a person’s quality of life, but also significantly shorten it.
Post-traumatic encephalopathy (ICD-10 - T90.5 and G93.8) is a specific brain disease that develops within a year after a traumatic brain injury.
A disease such as post-traumatic encephalopathy is not classified as chronic, but it can cause serious disruption of brain function and the appearance of symptoms that can not only significantly worsen a person’s quality of life, but also significantly shorten it.
Severity
There are 3 degrees of severity of encephalopathy resulting from injury, namely:
- First. It is detected mainly by chance, since the disease of this degree does not manifest itself in any way. Changes in brain tissue can be seen using hardware research methods;
- Second. In the case of this degree of severity, the manifestations of encephalopathy are extremely mild and occur in paroxysms. The most characteristic symptom is a neuropsychiatric disorder. It includes poor concentration, depression, memory impairment, outbursts of emotions, etc.;
- Third. It is characterized by pronounced neurological symptoms. Among the signs of grade 3 encephalopathy are dementia (dementia), ataxia, parkinsonism and other disturbances in the nervous system.
Causes and mechanism of development
There is only one cause for post-traumatic encephalopathy - trauma. The severity of the pathology depends on the location of the injuries and their severity. However, its development mechanism is not so simple and it includes the following stages:
- When injured, nerve fibers are damaged, often in the temple or forehead area;
- Due to serious damage, swelling of the brain is possible and, as a result, disruptions in its blood circulation;
- Swollen tissues compress the ventricular space (cerebral ventricles) and disruptions in the circulation of cerebrospinal fluid (CSF) occur;
- Dead nerve cells are replaced by connective tissue, as a result of which scars appear and adhesions form;
- Due to disruptions in the immune system caused by injury, the patient's body begins to perceive nerve cells as foreign objects and attacks them.
Classification of dementia according to ICD 10
Specialists diagnosing dementia select the main ones for a particular case from a variety of causes of impairment. Vascular dementia with ICD code 10 can be diagnosed to a patient in old age with certain manifestations or at a young age with injuries and pathology of the brain. Key numbers marked in the classification with the sign “*” cannot be used as independent numbers. Codification of dementia according to ICD 10:
- Alzheimer's disease has dementia code according to ICD 10: F00*. Alzheimer's disease is a brain disease of unknown origin, which manifests itself at the level of chemical regulatory mechanisms of the nervous system. The development of the disease occurs slowly and unnoticed by the patient and others, but progresses over several years;
- Vascular dementia ICD 10 code: F01 is interpreted as a result of cerebral infarction due to cerebral vascular disease. The development of the disease occurs at a late age;
- Dementia due to other diseases associated with causes not related to Alzheimer's disease or pathological conditions of the brain is coded: F02*. The development of the disease can begin at any age, but in old age the likelihood of its development is lower;
- dementia, unspecified. This category includes senile or senile dementia ICD: F03. Senile dementia is quite common: by the age of 80, the disease affects 25% of people.
Neurologists at the Yusupov Hospital use this classification when making a diagnosis, therefore, if a patient is diagnosed with ICD vascular dementia, then this fact is confirmed by certain clinical manifestations.
Symptoms
In most cases, post-traumatic encephalopathy of the brain is expressed depending on the severity of the injuries received and their location. However, you can find out about its presence by the following set of symptoms:
- Decreased mental activity;
- Memory impairment;
- Epileptic seizures;
- Outbursts of emotions, which are expressed mainly in the form of aggression;
- Depressive state;
- Trouble concentrating;
- Sleep rhythm disturbance;
- Nystagmus (involuntary fluctuations of the pupils);
- Severe headaches caused by disruptions in the circulation of cerebrospinal fluid;
- Manifestation of dizziness after physical overload;
- Development of astheno-neurotic syndrome.
Etiology and pathogenesis of disease development
It is believed that a condition such as post-traumatic encephalopathy develops due to severe damage to brain cells, impaired cerebral circulation and oxygen starvation. Post-traumatic encephalopathy is an extremely severe and serious consequence of head trauma. As a rule, such a complication begins to appear within 1 year after the injury. Thus, the main reason for the appearance of such a defect is severe trauma accompanying obvious defects of the cranial bones, against the background of which cerebrospinal fluid fistulas and other gross organic structural disorders of tissue are formed.
In many ways, the severity of the manifestation of post-traumatic encephalopathy depends on the location of the source of damage, the age of the victim and the presence of a person’s history of vascular diseases. In addition, post-traumatic encephalopathy more often develops in people who abuse alcohol. Post-traumatic encephalopathy often develops in people who have been in a car accident, as well as in those who have experienced a fall from a great height.
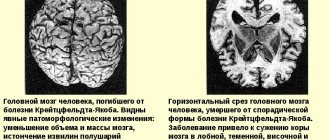
As a result of traumatic injury, atrophic processes are triggered in the brain tissue, which is why the brain gradually decreases in size. The death of brain tissue and its reduction in size leads to the fact that the vacated space is replaced by cerebrospinal fluid, that is, cerebrospinal fluid; among other things, as a result of these processes, compression of healthy cells is observed, which subsequently leads to unfavorable processes. As a person’s condition worsens and encephalopathy develops, localized foci of softening and breakdown of brain tissue appear. Where hematomas appear due to traumatic injury, large hollow areas filled with fluid may appear.
Diagnostics
If 2-3 symptoms from the list of main manifestations of encephalopathy are detected, then you should consult a neurologist. The diagnosis will be based on the collection of data on the trauma experienced and the appointment of the following instrumental research methods:
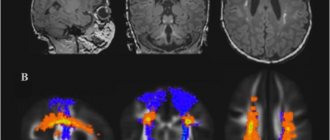
- Tomography (computer and magnetic resonance imaging). It is used to detect atrophic changes in brain tissue;
- Electroencephalography. It makes it possible to study the electrical activity of the brain and identify the presence of epileptic activity.
Dementia: ICD 10 code
The International Classification of Diseases is generally accepted throughout the world and is used to make a diagnosis. ICD-10 includes 21 sections, each of which contains headings with specific codes. Vascular dementia code according to ICD 10 and other forms of this disease are designated F00 – F09. This category includes mental disorders that are caused by injuries, brain diseases and strokes that lead to brain dysfunction.
When patients contact us, neurologists at the Yusupov Hospital carefully study the symptoms and conduct a full diagnosis to establish the origin of the disease, its stage, after which, together with other specialists, they determine possible treatment options.
Expert opinion
Author:
Vladimir Vladimirovich Zakharov
Neurologist, Doctor of Medical Sciences, Professor, Head of the Center for Diagnostics and Treatment of Memory Disorders
Dementia is the most diagnosed disease in old age. According to statistics, pathology occurs in 10% of cases in people over 65 years of age. After 80 years, the disease is detected in 25% of cases. Vascular dementia accounts for 10–15% of all cases of the disease in the elderly. The pathological condition is believed to be the cause of Alzheimer's disease. According to numerous clinical studies, the ability to detect vascular dementia decreases with age. But the chances of detecting Alzheimer's disease increase.
At the Yusupov Hospital, the diagnosis of vascular dementia is carried out using CT, MRI, ECG, EchoCG, and ultrasound scanning of the vessels of the brain and neck. Based on the data obtained, a therapeutic plan is developed.
Disruption of cerebral vessels requires immediate treatment. At the Yusupov Hospital, therapy is selected according to the type of disease. Among the main tasks of doctors is not only stabilization of the condition against the background of exacerbation of the disease, but also the selection of treatment that will reduce the risk of relapse. For this, neurologists use drugs that are part of the European recommendations for the treatment of vascular dementia.
A course of treatment
The treatment is carried out comprehensively and is aimed at protecting nerve cells and relieving emerging symptoms to improve the general condition. If the patient has developed cerebral edema, then medications are used to eliminate it - Diacarb.
In the presence of epileptic activity, antiepileptic medications are prescribed. After achieving the result, the course of therapy is repeated 1-2 times a year for preventive purposes.
To protect nerve cells, experts recommend the following groups of drugs with neuroprotective effects:
- Nootropics (Ceraxon, Piracetam);
- Antioxidants (Actovegin, Glycine, Neuronorm);
- Medicines that improve cerebral blood flow (Phenilin, Trental);
- Medicines with combined effects (Phesam, Thiocetam);
- Adaptogens (Eleutherococcus tincture).
Medications can also be added to the course of symptomatic therapy to reduce pressure inside the skull. Such drugs are prescribed mainly to hypertensive patients.
In addition to drug therapy, it is necessary to use the following methods in treatment:
- Meditation;
- Massotherapy;
- Sports activities;
- Acupuncture;
- Breathing exercises.
It is recommended to start visiting a psychologist and devote time to special exercises to normalize the psycho-emotional background. Start following a healthy lifestyle, and for this you should remember the following rules:
- Make a proper diet;
- Exercise;
- Take a walk in the fresh air;
- Get enough sleep (at least 6-8 hours a day);
- To refuse from bad habits.
In extreme cases, surgery will be required. It is necessary in the absence of treatment results. The purpose of the operation is to restore cerebral circulation.
Treatment methods
Adequate therapy is aimed at protecting neurons from damaging factors. It normalizes blood circulation in brain tissue, restores metabolism and cognitive functions. It involves an individual selection of medications including vitamins, diuretics, analgesics, antioxidants (including tranquilizers, nootropic, antipsychotic compounds), supplemented by physiotherapy. Consultations with a psychotherapist provide correction of impairments in the cognitive sphere, which is important for a favorable outcome in the treatment of post-traumatic encephalopathy.
To optimize metabolic processes in brain neurons, the doctor prescribes Piracetam. Cerebrolysin, obtained from pig brain, is characterized by a high content of biologically active amino acids and polypeptides. It is intended for the formation of new synapses and the proliferation of short processes. Helps nerve cells survive in conditions of ischemia and oxygen deficiency, exhibits antioxidant properties. Efficacy depends on dosage. With Cerebrolysin they are quite high, since the drug does not have a psychostimulating effect.
ethnoscience
The use of traditional medicine methods is permitted after the approval of the attending physician. They cannot completely cure a person from post-traumatic encephalopathy, but they can reduce its severity and complement the main course of therapy. The following recipes have worked well:
- Hawthorn fruits. They serve to improve cerebral blood flow and strengthen the walls of blood vessels. To prepare the decoction, take 2 tbsp. l. crushed hawthorn fruits and pour them into a container with 500 ml of boiling water. Then the resulting mixture must be left to settle for 12 hours. After preparation, you can use the decoction 3 times a day before meals;
- Rosehip berries. They have a good effect on cerebral vessels and improve general condition. To prepare, you need to take 4 tbsp. l. dried and crushed berries and pour them into a liter container with boiling water. After 3-4 hours, the decoction will be ready and experts recommend replacing tea with it, since the drink is non-toxic and very healthy.
G00—G09 Inflammatory diseases of the central nervous system
G00 Bacterial meningitis, not elsewhere classified
On: bacterial:
- arachnoiditis
- meningitis
- meningitis
- pachymeningitis
Excl.: bacterial:
- meningoencephalitis (G04.2)
- meningomyelitis (G04.2)
G00.0 Influenza meningitis
Meningitis caused by Haemophilus influenzae
G00.1 Pneumococcal meningitis
G00.2 Streptococcal meningitis
G00.3 Staphylococcal meningitis
G00.8 Meningitis caused by other bacteria
- Friedlander wand
- Escherichia coli
- Klebsiella
G00.9 Bacterial meningitis, unspecified
- purulent NOS
- pyogenic NOS
- pyogenic NOS
G01 * Meningitis in bacterial diseases classified elsewhere
Incl.: Meningitis (with):
- anthrax (A22.8)
- gonococcal (A54.8)
- leptospirosis (A27.-)
- listeriosis (A32.1)
- Lyme disease (A69.2)
- meningococcal (A39.0)
- neurosyphilis (A52.1)
- salmonellosis (A02.2)
- syphilis: secondary (A51.4)
- congenital (A50.4)
Excl.: meningoencephalitis and meningomyelitis in bacterial diseases classified elsewhere (G05.0*)
G02 * Meningitis in other infectious and parasitic diseases classified elsewhere
Excl.: meningoencephalitis and meningomyelitis in infectious and parasitic diseases classified elsewhere (G05.1-G05.2*)
G02.0 * Meningitis in viral diseases classified elsewhere
Meningitis (caused by a virus):
- adenoviral (A87.1)
- enterovirus (A87.0)
- herpes simplex (B00.3)
- infectious mononucleosis (B27.-)
- measles (B05.1)
- mumps (B26.1)
- rubella (B06.0)
- chickenpox (B01.0)
- herpes zoster (B02.1)
G02.1 Meningitis in mycoses
Meningitis:
- candidiasis (B37.5)
- coccidioidomycosis (B38.4)
- cryptococcal (B45.1)
G02.8 * Meningitis in other specified infectious and parasitic diseases classified elsewhere
Meningitis caused by:
- African trypanosomiasis (B56.-)
- Chagas disease (B57.4)
G03 Meningitis due to other and unspecified causes
On:
- arachnoiditis
- meningitis
- meningitis
- pachymeningitis
Excl.:
- meningoencephalitis (G04.-)
- meningomyelitis (G04.-)
G03.0 Non-pyogenic meningitis
Nonbacterial meningitis
G03.1 Chronic meningitis
G03.2 Benign recurrent meningitis (Mollaret)
G03.8 Meningitis caused by other specified pathogens
G03.9 Meningitis, unspecified
Arachnoiditis (spinal) NOS
G04 Encephalitis, myelitis and encephalomyelitis
On:
- acute ascending myelitis
- meningoencephalitis
- meningomyelitis
Excl.:
- benign myalgic encephalitis (G93.3)
- encephalopathy: NOS (G93.4)
- alcoholic origin (G31.2)
- toxic (G92)
- sharp transverse (G37.3)
G04.0 Acute disseminated encephalitis
Post-immunization:
- Encephalitis
- Encephalomyelitis
G04.1 Tropical spastic paraplegia
G04.2 Bacterial meningoencephalitis and meningomyelitis, not elsewhere classified
G04.8 Other encephalitis, myelitis and encephalomyelitis
Postinfectious encephalitis and encephalomyelitis NOS
G04.9 Encephalitis, myelitis or encephalomyelitis, unspecified
Ventriculitis (cerebral) NOS
G05 * Encephalitis, myelitis and encephalomyelitis in diseases classified elsewhere
G05.0 * Encephalitis, myelitis and encephalomyelitis in bacterial diseases classified elsewhere
Encephalitis, myelitis or encephalomyelitis (with):
- listeriosis (A32.1)
- meningococcal (A39.8)
- syphilis: congenital (A50.4),
- late (A52.1)
G05.1 * Encephalitis, myelitis and encephalomyelitis in viral diseases classified elsewhere
Encephalitis, myelitis and encephalomyelitis with:
- adenoviral (A85.1)
- cytomegaloviral (B25.8)
- enteroviral (A85.0)
- herpesviral (B00.4)
- influenza (J09, J10.8, J11.8)
- meats (B05.0)
- mumps (B26.2)
- postchickenpox (B01.1)
- rubella (B06.0)
- zoster (B02.0)
G05.2 * Encephalitis, myelitis and encephalomyelitis in other infectious and parasitic diseases classified elsewhere
Encephalitis, myelitis and encephalomyelitis with:
- African trypanosomiasis (B56.-)
- Chagas disease (chronic) (B57.4)
- naegleriasis (B60.2)
- toxoplasmosis (B58.2)
Eosinophilic meningoencephalitis (B83.2)
G05.8 * Encephalitis, myelitis and encephalomyelitis in other diseases classified elsewhere
Encephalitis in systemic lupus erythematosus (M32.1)
G06 Intracranial and intravertebral abscess and granuloma
G06.0 Intracranial abscess and granuloma
Abscess (embolic):
- brain (any part)
- cerebellar
- cerebral
- otogenic
Intracranial abscess or granuloma:
- epidural
- extradural
- subdural
G06.1 Intravertebral abscess and granuloma
Abscess (embolic) of the spinal cord (any part)
Intravertebral abscess or granuloma:
- epidural
- extradural
- subdural
G06.2 Extradural and subdural abscess, unspecified
G07 * Intracranial and intravertebral abscess and granuloma in diseases classified elsewhere
Include: Brain abscess:
- amoebic (A06.6)
- gonococcal (A54.8)
- tuberculous (A17.8)
Granuloma of the brain in schistosomiasis (B65.-)
Tuberculoma:
- brain (AI7.8)
- meninges (A17.1)
G08 Intracranial and intravertebral phlebitis and thrombophlebitis, septic, intracranial or intravertebral venous sinuses and veins
Excl.:
intracranial phlebitis and thrombophlebitis: complicating:
- abortion
- ectopic or molar pregnancy (O00 - O07, O08.7)
- pregnancy
- childbirth or puerperium (O22.5, O87.3)
- non-purulent origin (I67.6)
- non-purulent intravertebral phlebitis and thrombophlebitis (G95.1)
G09 Consequences of inflammatory diseases of the central nervous system
Note: This category should be used to identify conditions primarily classified in categories G00 to G08 (excluding those marked with *) as the cause of consequences that are themselves classified in other categories.
The concept of “consequences” includes conditions specified as such or as late manifestations or consequences that exist for a year or more after the onset of the condition that caused them.
Forecast
Predictions can only begin to be made 6-12 months after injury. All this time, the patient must follow the doctor’s recommendations and undergo the necessary rehabilitation procedures. After all, eliminating the consequences of injuries is often extremely difficult. However, it is necessary to continue to do this, since in some cases the defects were completely or partially eliminated 5-7 years after the injury.
Regardless of the presence or absence of possible consequences, the experience of post-traumatic encephalopathy is an exemption from military service. If the patient's mental activity is greatly reduced, then he is given a disability.
This encephalopathy is a severe complication of a traumatic brain injury. It manifests itself depending on the location of the injury and the severity. The pathology can be eliminated with the help of symptomatic therapy and drugs with a neuroprotective effect.