Destruction of central nervous system structures can be focal or disseminated, that is, having multiple zones of damage. MRI (magnetic resonance imaging) allows you to determine how the process is progressing. With its help, the diagnostician visually (using photographs) assesses the condition of the nervous tissue.
Focal brain damage - what is it and how does it manifest itself? First of all, it is a symptom of pathology, due to which in one of the areas of the organ there is a disruption in the performance of the corresponding structures, which is signaled by the appearance of neurological abnormalities.
What is demyelination
The demyelinating process that occurs in the brain is a disorder that leads to a pathological change in the structure of the nervous tissue, which often provokes the appearance of neurological symptoms and causes disability and death. The white shell is a multilayer cell membrane. Biocurrents are not able to overcome the myelin sheath.
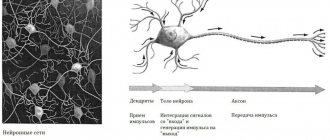
Electrical impulses are transmitted to the areas of numerous nodes of Ranvier, where myelin is absent. The interceptions are located at regular intervals of approximately 1 µm in length. In the peripheral system, the protective membrane is formed from lemmocytes (Schwann cells). Demyelination of nerve fibers is a lesion of nervous tissue that leads to a large number of central nervous system diseases.
Foci of demyelination are structural formations in the brain or spinal cord that lack myelin, which leads to disruption of the transmission of nerve impulses and disruption of the nervous system as a whole. The diameter of the lesions varies significantly; it can be several millimeters or reach several centimeters.
Classification of the disease
When describing demyelination, doctors talk about myelinoclasty - a violation of the membrane of neurons due to genetic factors.
Lesions that appear due to diseases of other organs indicate myelinopathy.
Pathological foci occur in the brain, spinal cord, and peripheral parts of the nervous system. They may be generalized in nature - in this case, the damage affects the membranes in various parts of the body. When isolated, the lesion is observed in a limited area.
The classification of this disease is based on the reasons for its development:
- if a patient has a hereditary autoimmune disorder in the body that contributes to the destruction of its own myelin proteins, then we are talking about myelinoclasty;
- in case of destruction of the myelin sheath due to any factors (illness, poisoning, etc.), the disease is classified as myelinopathy.
The consequences of such an illness are very serious. Often there is a persistent neurological deficit, and the person's condition and standard of living quickly deteriorate. Very severe complications such as respiratory arrest occur. The death of the patient is also possible.
Classification of demyelination occurs into two types:
- Damage to myelin, a consequence of a gene disorder, called myelinoclasty;
- Deformation of the integrity of the myelin sheaths under the influence of factors that are not related to myelin (myelinopathy).
Among them are:
- Deformation of the membranes in the central nervous system;
- Destruction of myelin sheaths in the peripheral structures of the nervous system.
The final division of demyelination is based on prevalence.
The following subspecies are distinguished:
- Isolated, when disruption of the myelin sheaths occurs in one place;
- Generalized, when the demyelinating disease affects many membranes in different parts of the nervous system.
Causes and mechanisms of demyelination
Types of demyelinating diseases
The classification of demyelinating diseases involves division into myelinopathy and myelinoclasty. In the first case, the destruction of myelin occurs due to a disruption in the formation of the substance, a change in its biochemical structure due to genetic mutations. This is often a congenital pathology (there is also an acquired form), the signs of which are observed in early childhood. Hereditary myelinopathies are called leukodystrophies. Acquired myelinopathies, depending on the causes of occurrence, are divided into types:
- Toxic-dysmetabolic. Associated with intoxication and metabolic disorders in the body.
- Hypoxic-ischemic. They develop against the background of impaired blood flow and oxygen starvation of brain tissue.
- Infectious and inflammatory. Triggered by infectious agents (pathogenic or opportunistic microorganisms).
- Inflammatory. Non-infectious etiology (occurs without the participation of an infectious agent).
- Traumatic. They arise due to mechanical damage to brain structures.
With myelinoclasty, myelin synthesis proceeds normally, the membrane cells are destroyed under the influence of external and internal pathogenic factors. The division is arbitrary because myelinopathy often progresses under the influence of negative external factors, while myelinoclasty usually occurs in patients with a predisposition to myelin damage.
Demyelinating diseases are divided according to the location of the lesions into types that affect the central nervous system or the peripheral nervous system (PNS). Diseases that develop in the structures of the central nervous system include multiple sclerosis, leukoencephalopathies, leukodystrophies, Balot (concentric) and Schilder (diffuse) sclerosis.
Damage to the fiber sheaths of the PNS provokes the development of diseases: Charcot-Marie-Tooth amyotrophy, Guillain-Barré syndrome. Examples of acquired myelinopathies: Susak and CLIPPERS syndromes. A common inflammatory myelinopathy of non-infectious etiology is multiple sclerosis.
This group includes quite rare types of sclerosis: multiple encephalomyelitis, pseudotumorous demyelination, hemorrhagic leukoencephalitis, Balo and Schilder’s sclerosis. Infectious-inflammatory forms include HIV encephalitis, sclerosing panencephalitis, cytomegalovirus encephalitis. An example of a toxic-metabolic form is demyelinating syndrome of the osmotic type, an example of a hypoxic-ischemic form is Susak syndrome.
Features of MRI diagnostics of focal changes in the brain substance
As a rule, the presence of focal changes in the brain substance becomes known after the patient has undergone an MRI. To clarify the nature of the lesion and differential diagnosis, the study can be performed with contrast.
Multiple focal changes are more typical for infections, congenital pathology, vascular disorders and dysmetabolic processes, multiple sclerosis, while single focal changes occur after strokes, perinatal lesions, certain types of injuries, and tumor metastasis.
Main symptoms
Demyelination is a pathology that always manifests itself as a neurological deficit, which makes it possible to suspect the beginning of the process of myelin destruction if neurological symptoms appear without obvious reasons. The demyelinating process always occurs with the participation of the immune system, leading to atrophy of brain tissue - brain and spinal cord, and dilation of the ventricles.
Symptoms of demyelination depend on the type of disease, the causes and localization of the lesion in the brain, spinal cord or in the structures of the PNS. With minor damage to the brain substance (up to 20%), symptoms may be absent, which is associated with complete compensation of functions. The tasks assigned to damaged nerve fibers are performed by healthy tissues. Neurological symptoms usually appear in cases where the amount of nerve tissue damaged exceeds 50%. General signs:
- Ataxia (disorder of coordination when working a muscle group).
- Paresis, paralysis.
- Muscular hypotonia (muscle weakness).
- Pseudobulbar syndrome (dysarthria - impaired pronunciation due to a disorder of the innervation of the elements of the speech apparatus, dysphagia - difficulty swallowing, dysphonia - changes in pitch, timbre, strength of the voice).
- Visual dysfunction (nystagmus - involuntary oscillations of the eyeballs, deterioration of visual acuity, loss of visual fields, blurred, unclear images, color distortion).
- Changes in skin sensitivity, paresthesia (numbness, tingling, itching, burning).
- Tonic spasms, mainly in the extremities.
- Bladder and bowel dysfunction.
Neuropsychological disorders are associated with deterioration of memory and mental activity, changes in personality and behavior. Patients often develop neuroses, dementia of organic origin, asthenic syndrome, depression, and less often euphoria. Patients are subject to sudden changes in mood, they lack a critical analysis of their own behavior, which, against the background of dementia, leads to numerous problems in everyday life.
Demyelinating process of the brain: what is it, signs, treatment
The most common disease is MS. It is characterized by the following first signs:
- Nystagmus (eye fluctuations);
- Slow speech (chanted);
- Trembling that occurs when moving (intention tremor);
- A split picture before your eyes;
- A sudden urge to go to the toilet (urgency);
- Problems with urination (retention due to spasm);
- Weakening or complete absence of abdominal reflexes;
- Pallor of the temporal part of the optic nerve.
As the pathology develops, the patient experiences the following symptoms:
- Deterioration of sensitivity of the facial nerve;
- Impaired coordination of movements;
- Dizziness;
- Babinsky asynergia (impaired functioning of the limbs);
- Adiadochokinesis (inability to perform rapid movements);
- Increased intention tremor;
- Failures that are diagnosed in the Romberg position;
- Decreased perception of pain, temperature and touch;
- Weakening and paralysis of individual muscle groups;
- Excessive increase in tone in muscle tissue;
- Hearing impairment;
- General muscle weakness.
Causes
Demyelinating diseases affecting the central and peripheral nervous systems often develop against the background of a genetic predisposition. Patients often have a combination of certain genes that causes malfunctions of the immune system. Other reasons:
- Autoimmune and genetic pathologies.
- Taking antipsychotic drugs (neuroleptics).
- Chronic and acute intoxications.
- Ionizing radiation, solar radiation.
- Past viral and bacterial infections.
- Nutritional features.
It is believed that representatives of the Caucasian race living in northern latitudes are most susceptible to the development of pathology. Provoking factors are injuries to the head and spine, frequent stressful situations, and bad habits. The risk of getting sick increases due to vaccination against smallpox, influenza, measles, whooping cough, diphtheria, hepatitis type B and other infectious diseases.
Amyotrophic lateral sclerosis (LAS)
LAS begins unnoticed. The patient has difficulty with normal activities (writing, fastening buttons). Later, problems with walking, muscle cramps, and difficulty swallowing develop. At the end, the patient is completely paralyzed and depends on artificial respiration and nutrition. In fatal LAS, the patient gradually loses nerve cells. In 5-10% of cases the disease has a hereditary form.
Demyelinating disease is characterized by selective damage to central and peripheral motor neurons (a motor neuron is a nerve cell that directly innervates skeletal muscles). We are talking about the gradual disappearance of motor neurons of the spinal cord, in the area of the brain stem, degeneration of the corticospinal tract.
Common diseases
Multiple sclerosis is a demyelinating, autoimmune disease with a chronic course that affects the main elements of the nervous system (brain and spinal cord). As the pathology progresses, normal brain structures are replaced by connective tissue. The lesions appear diffusely. The average age of patients is 15-40 years. Prevalence – 30-70 cases per 100 thousand population.
Hemorrhagic leukoencephalitis, which occurs in an acute form, develops due to damage to small elements of the vascular system. Often defined as a post-infectious complication with a pronounced autoimmune reaction. It is characterized by rapid progression of the inflammatory process and numerous focal lesions of brain tissue, accompanied by cerebral edema, the appearance of foci of hemorrhage, and necrosis.
The precursor to the pathology is usually diseases of the upper respiratory tract of infectious etiology. The disease can also be triggered by influenza and Epstein-Barr viruses or sepsis. Usually leads to death. Death occurs due to cerebral edema within 3-4 days from the onset of the first symptoms.
Necrotizing encephalopathy, which occurs in an acute form, is characterized by multifocal, symmetrical damage to brain structures of a demyelinating nature. Accompanied by tissue swelling, necrosis and the appearance of foci of hemorrhage. Unlike hemorrhagic leukoencephalitis, cells indicating an inflammatory process - neutrophils - are not detected.
Often develops against the background of a viral infection, manifested by epileptic seizures and confusion. There is no pleocytosis (abnormally increased concentration of lymphocytes) in the cerebrospinal fluid; the concentration of protein compounds is increased. An increased concentration of aminotransferase is detected in the blood serum. It develops sporadically (in single cases) or due to a hereditary gene mutation.
Pseudotumorous demyelination is manifested by general cerebral and focal cerebral symptoms. In 70% of cases it is accompanied by edema of the brain matter with an increase in intracranial pressure. Foci of demyelination are detected in the white matter during an MRI study of the brain using a contrast agent.
Balo's sclerosis (concentric) is manifested by pain in the head, pathological changes in behavior, cognitive disorders, epileptic seizures, hemisyndromes (neurological disorders in one half of the body). The course of the pathology clinically resembles the development of an intracerebral tumor. Foci of tissue damage are most often observed in the white matter.
Lymphocytic pleocytosis and an increased concentration of protein compounds are detected in the cerebrospinal fluid. The presence of oligoclonal antibodies is often observed in smaller quantities than in normal multiple sclerosis. An MRI scan shows signs of brain tissue damage typical of multiple sclerosis.
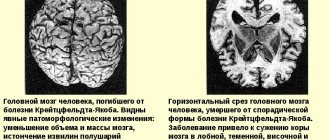
The images clearly show multiple ring-shaped foci of demyelination in the white matter, often in the frontal lobes of the brain, surrounded by characteristic areas of remyelination (restoration of normal myelin). In most cases, death occurs within several weeks or months of the acute course of the pathology. With early diagnosis, the prognosis is more favorable.
On the way to diagnosis
When the patient feels that something wrong is happening, but it is no longer possible to justify the changes with fatigue or stress, he goes to the doctor. It is extremely problematic to suspect a specific type of demyelinating process only based on the clinic, and the presence of demyelination itself is not always clear to a specialist, so additional research is indispensable.
example of demyelination foci in multiple sclerosis
MRI is traditionally considered the main and very informative way to diagnose the demyelinating process. This method is harmless, can be used for patients of different ages, pregnant women, and contraindications include excessive weight, fear of closed spaces, the presence of metal structures that react to a strong magnetic field, and mental illness.
Round or oval hyperintense foci of demyelination on MRI are found predominantly in the white matter under the cortex, around the ventricles of the brain (periventricular), diffusely scattered, and have different sizes - from a few millimeters to 2-3 cm. To clarify the time of formation of foci, contrast enhancement is used, with In this case, “younger” fields of demyelination accumulate contrast agent better than those that have existed for a long time.
The main task of a neurologist when detecting demyelination is to determine the specific form of pathology and choose the appropriate treatment. The prognosis is ambiguous. For example, with multiple sclerosis, you can live a dozen or more years, while with other types, life expectancy can be a year or less.
Diagnostics
In the absence of characteristic symptoms in the early stages of the course, white matter lesions often become an incidental finding during a diagnostic examination for another reason. During a personal examination by a neurologist, the degree of impairment of the conductive functions of the brain is determined using the FSS scale (state of functional systems).
The main method of instrumental diagnostics is neuroimaging. Foci of demyelination located in the brain are mainly detected using MRI studies; the images clearly show areas of affected tissue with a diameter of at least 3 mm. Foci of demyelination in the structures of the PNS are detected during electromyography. Angiography shows the extent of vascular damage.
Treatment methods
The disease is incurable. The efforts of doctors are aimed at eliminating symptoms and improving the patient’s quality of life. Treatment of demyelinating diseases that affect the brain is prescribed depending on the type and nature of the course. Pharmaceutical agents that neutralize the manifestations of neurological syndromes are usually indicated. Symptomatic therapy includes drugs:
- Painkillers.
- Sedatives, sedatives.
- Neuroprotective, nootropic.
To treat rapidly progressing forms of multiple sclerosis, pulse corticosteroid therapy is used. Intravenous administration of large doses of the drug often does not give the desired result. In case of a positive reaction after a course of intravenous administration, corticosteroids are prescribed orally to prevent relapse. Corticosteroids can be combined with other immunosuppressive (immune-suppressing) drugs and cytostatics.
In 40% of cases, patients resistant to corticosteroid therapy respond positively to plasmapheresis (collection, purification and reintroduction of blood into the bloodstream). Cases of effective treatment of Balo's sclerosis with human immunoglobulins have been described. Therapy with folk remedies is ineffective. In parallel with drug treatment, patients are prescribed diet, physiotherapy, massage, and therapeutic exercises.
Forecast
The survival prognosis depends on the type of pathology, the nature of the course and the extent of brain damage. Partial or complete restoration of brain function is possible.
Demyelinating diseases, affecting the structures of the central nervous system and PNS, are associated with the destruction of the sheath surrounding the nerve fibers. In the initial stages of the disease, they may be asymptomatic. The prognosis with early diagnosis is more favorable. The disease cannot be completely cured and often leads to disability and death of the patient.
900