A transient ischemic attack (or simply a microstroke) is a disorder in the cerebral circulation. A micro-stroke occurs when oxygen stops flowing through the blood to the brain. This condition differs from a massive ischemic stroke only in that the body is able to independently again ensure sufficient blood flow to the brain. Despite the fact that the recovery process occurs quite quickly and without the help of doctors, a small stroke is still very dangerous and such a condition cannot be ignored.
This article will discuss methods for diagnosing a microstroke, its consequences, treatment and recovery of the body after the disease.
What is a microstroke
It should be immediately clarified that such a diagnosis and disease as microstroke does not exist in the International Classification of Diseases, but despite the fact that the term is colloquial, it is used by both patients and doctors. What we call a microstroke is interpreted in medicine as a transient disturbance of cerebral blood flow. This is the most common type of vascular dysfunction, which is a “warning” of the body about an impending much more terrible problem - a stroke.
In simple terms, a transient ischemic attack is a sudden blockage of the arterial lumen by a blood clot, the body copes with the dissolution of which on its own, and the flow of blood to the brain is resumed. Cerebral blood flow is restored within a few minutes and the signs of an ischemic attack that have already appeared disappear without a trace. Then what is the difference between a microstroke of the brain and a major stroke?
Differences from stroke
Firstly, during a massive hemorrhage in the brain, a large blood clot forms and the body is not able to cope with it quickly. The blood clot disappears only after a few hours or days. During this period, brain cells and tissues rapidly die due to nutritional deficiency and oxygen starvation. They will never be able to recover, so the patient’s severe consequences remain for life.
Secondly, the symptoms of a microstroke are less pronounced, and doctors mistakenly diagnose many patients with “vegetative-vascular dystonia,” attributing the ailment to a violation of cerebral vascular tone. A minor stroke is a serious signal that the blood supply to the brain has failed and the risk of a severe stroke is high. It should be remembered that a repeated micro-stroke can cause the same tragic consequences as a massive cerebral hemorrhage.
Ischemic microstroke: who is at risk
An attack, as a rule, appears against the background of certain predisposing external or internal factors. Most often, many chronic diseases lead to illness:
- Atherosclerosis (systemic vascular damage). If a person suffers from cardiac ischemia, then atherosclerotic plaques will also be in the vessels of his brain.;
- Hypertension;
- Diseases of the cardiovascular system;
- Diabetes;
- Severe obesity
- High cholesterol levels in the blood;
- Major blood loss suffered in the past;
- Heart disease (tachycardia, myocardial infarction);
- High concentration of red blood cells in the blood.
A large number of people facing ischemia lead a sedentary lifestyle, abuse alcohol and smoke for quite a long time.
Regular headaches and taking oral contraceptives also increase the risk of developing an attack.
Knowing the causes of a micro-stroke and being able to recognize it in time, one should begin to prevent more severe disorders in the body, with the ensuing consequence of a stroke.
Causes
The main causes of transient cerebral circulatory disorders are identified:
- Hyperlipidemia and atherosclerosis . Atherosclerotic damage to the carotid and brachiocephalic arteries is the basis for atherothromboembolism , which causes micro-stroke in 50% of cases.
- Arterial hypertension . Damage to cerebral vessels in hypertension is associated with changes in small arteries, arterioles and capillaries, which acquire pathological tortuosity, lose elasticity and the ability to quickly expand when necessary. In addition, arterial hypertension accelerates the development of atherosclerosis , which is an independent risk factor for micro-stroke.
- Anomalies of the development of the vertebral and carotid arteries.
- Angiopathy due to diabetes mellitus .
- Vascular damage in systemic diseases, vasculitis .
- Hematological diseases ( sickle cell anemia , erythremia , leukemia ).
- Carotid stenosis , which causes microstroke in 50% of cases.
- Heart diseases with rhythm disturbances (for example, atrial fibrillation ), in which there is a tendency to form blood clots in the cavities of the heart and there is a risk of cardiogenic thromboembolism .
- Obstructive sleep apnea .
- Coagulopathies ( protein C , antithrombin III protein S deficiency ).
Predisposing factors:
- Smoking.
- Physical inactivity.
- Alcohol abuse.
- Overweight.
- Hyperhomocysteinemia.
If we consider the causes of disturbances in the vertebrobasilar system, these will be a variety of conditions and diseases leading to obliteration of the vertebral arteries:
- Tortuosity of the arteries (characteristic of arterial hypertension), which can lead to kinking of the vertebral artery - stenosis will form and blood flow will be disrupted.
- Congenital anomalies of the vertebral arteries. Insufficiency of blood flow in one vertebral artery can be compensated for a long time by another vertebral artery. With age and the development of atherosclerosis and arterial hypertension, decompensation occurs.
- Changes in the rheological properties of blood. This refers to an increase in platelet and blood viscosity, an increase in hematocrit - all these conditions in the body worsen microcirculation.
- Compression of the vertebral artery by an osteophyte , an articular process (for example, with instability of the cervical spine), a spasmodic neck muscle, or an accessory cervical rib.
Insufficiency of blood flow in the vessels of the vertebrobasilar system is manifested by attacks of falling, but without loss of consciousness (drop attacks), which occur with sudden turns of the head or throwing back the head. The risk group for the development of micro-strokes includes people who have:
- severe osteochondrosis of the cervical spine;
- previous skull injuries and concussions;
- constant nervous professional stress;
- congenital vascular pathology.
The first signs of a microstroke
Above, we tried to figure out who can be “overtaken” by a microstroke and what it is. Now let's talk about how to identify a microstroke by its primary symptoms. It is not difficult to suspect a minor ischemic stroke in yourself or someone nearby, knowing what symptoms are characteristic of it:
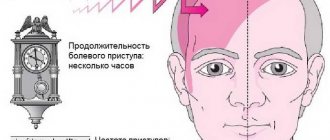
- The patient complains of dizziness and increasing severe headache;
- Vision deterioration often occurs: flashes and “spots” appear before the eyes;
- Coordination of movements is impaired: a person may stagger and even fall;
- Part of the face or limb goes numb;
- Blood pressure changes, vomiting is possible;
- Bright light and noise cause irritability and worsen headaches;
- The ability to speak deteriorates: it is difficult for a person to answer basic questions, speech becomes inarticulate.
Be sure to call an ambulance!
It is important to note here that even if the signs of the disease completely subsided after a few minutes, the state of health became normal, an ambulance should still be called. Timely detection of an attack significantly increases the chances of complete recovery.
An ischemic attack of the brain may recur soon and possibly in a more serious form. Statistics say that a third of people experience the symptoms of a mini-stroke again. Every tenth person after a “minor hemorrhage” experiences a major stroke within three months. Moreover, 50% of attacks occur within the first 48 hours.
A microstroke and its symptoms are the first signs of an approaching major stroke.
Specificity of signs: why is a microstroke dangerous?
Many patients attribute the first symptoms of a micro-stroke (dizziness, headache of any intensity, general weakness) to constant fatigue and stress, weather changes and magnetic storms. Often, some symptoms of an attack are absent or mild, however, 4-5 signs are enough to make a diagnosis.
Classic neurological signs of the disease develop to a greater extent in men. At the same time, the risk of cerebrovascular accidents in women from 20 to 40 years of age is higher compared to men of the same age.
Often, a person’s attack can be noticed quickly by those around him: the patient’s speech suddenly becomes incoherent, he becomes silent or stops responding to calls. The man looks like he's drunk.
Main symptoms
Signs of a microstroke in women resemble the picture of a regular stroke:
- Violation of facial symmetry: sliding of the lips, cheeks or eyelids on one side.
- Inability to raise both arms in front of you and hold them in the air without weakness or numbness.
- Slurred speech, poor pronunciation of words.
- Visual impairment: blurred vision, double vision, appearance of black dots.
Other symptoms of TIA include:
- partial loss of vision in one eye;
- dizziness;
- communication problems: the person speaks indistinctly and does not understand what is said to him;
- impaired balance and coordination;
- problems with swallowing;
- numbness or weakness, which can lead to paralysis on one side of the body;
- loss of consciousness (in severe cases).
Most often, patients note a sharp headache (in 90% of cases), then dizziness (in 13%), numbness of the face and lips (almost 40%) and extremities (54% of cases). The one-time or episodic nature of the listed signs of a microstroke is assessed as a manifestation of neurocirculatory dystonia.
First aid
What to do before the doctors arrive if a micro-stroke begins in a loved one?
First of all, you should put the patient to bed and ensure maximum peace in the room where he is located. To make breathing easier, you need to remove tight clothes (at least unfasten the collar, loosen the belt). Place a pillow (folded clothes, blanket, etc.) under the patient’s head so that the shoulders are also raised: this is necessary so that the blood flow in the vertebral arteries does not deteriorate. If blood pressure readings are above 140/90, then the patient can be given medications that lower blood pressure.
It is important to know: the neurological symptoms characteristic of cerebral hemorrhages are similar to the clinical manifestations of myocardial infarction. Sometimes diagnosis is difficult even for experienced specialists, so you should not take or give the patient numerous medications on your own: taking the wrong pills can only aggravate the condition.
How to recognize a micro-stroke
Diagnosis of this disease is based on a complete examination of the state of the cardiovascular system. Usually, for the accuracy of the diagnosis, consultation with an ophthalmologist, cardiologist, or therapist is required.
Studies that help make an accurate diagnosis include:
- Electrocardiogram (ECG),
- Echocardiogram,
- Complete blood test
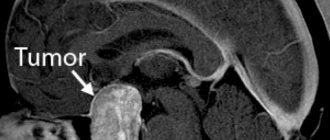
- Computed tomography (CT),
- Magnetic resonance diagnostics,
- Blood clotting test (coagulogram),
- MRI (magnetic resonance imaging).
A doctor can decide how to treat a microstroke only after studying the results of the examination. Thus, the result of an electrocardiogram may indicate that the formation of a blood clot, which prevented the flow of blood to the brain, occurred in the heart. In such cases, the doctor may decide to prescribe anticoagulants. The result of an ultrasound examination of the carotid arteries can show whether there are atherosclerotic lesions of the vessels (their lumen is too narrow due to atherosclerosis). As a measure to prevent ischemia and stroke, surgery may be recommended in such situations.
Consequences
The consequences of a micro-stroke may not be noticeable if it was experienced only once. Otherwise, brain cells begin to experience “oxygen starvation.” It leads to:
- Memory impairment;
- The appearance of dementia;
- Change of character for the worse.
Every micro-stroke a person experiences is a blow to the health of the brain, leading to premature aging.
Treatment involves restoring cerebral blood flow to the affected area. Rehabilitation after a mini-stroke begins, first of all, with studying the medical history: this allows you to identify the true cause of the disease and select appropriate medications for the recovery period.
Diet for microstroke in men
After an attack, sweet and salty foods, street food, fatty meats, and smoked foods are prohibited. What should be included in a patient’s daily menu after a mini-stroke?
- Protein. This component is necessary for any organism. After illness and stress, protein amino acids allow the restoration of damaged tissue. Important sources of protein: lean meat (turkey, chicken, rabbit, veal), fish (cod, pink salmon, chum salmon), cottage cheese, unsweetened yogurt;
- Carbohydrates. Cereals (buckwheat, millet, rice, oats), rarely pasta, potatoes (rarely);
- Fats. Vegetable oils (linseed, olive, sesame, sunflower);
- Products containing fiber. These are vegetables and fruits. In case of diabetes mellitus, it is recommended to limit their quantity. But if there is no insulin resistance, then the amount of vegetables and fruits in the diet should be at least 500 grams. Recommended are fresh greens (spinach, arugula, lettuce), root vegetables (carrots, turnips, beets), fruits (apples, pears, plums), berries (blueberries, currants, cranberries).
Beverages. You should limit your diet to strong coffee, tea and alcohol. Sugary carbonated drinks should be avoided. The volume of fluid should be at least 1.5-2 liters of clean water, if there are no restrictions on arterial hypertension. For drinks, you can use fruit drink, weak tea, or rosehip decoction.
Micro-stroke in men occurs quite often and leads to dire consequences if the disease has not been given enough attention. A transient attack should be considered a wake-up call. The body signals that lifestyle changes are needed. And if he is not heard, then you should not expect a good outcome.
Treatment
The drugs most often used in the complex treatment of disorders of this disease are aimed at:
- Restoration of blood microcirculation in blood vessels;
- Improving blood flow, dilating blood vessels;
- Preventing the accumulation of platelets on the walls of blood vessels;
- Improved brain activity;
- Normalization of blood pressure;
- Improving metabolic processes (blood oxygen saturation).
Recovery after a mini-stroke is aimed at preventing recurrent attacks. Treatment at the rehabilitation stage may also include physiotherapeutic procedures: massage, therapeutic exercises, circular shower, electrophoresis. In specialized centers, hirudotherapy (treatment with leeches) is often used, which helps normalize blood flow and cleanse blood vessels of blood clots.
To exclude a relapse, the patient must be observed by a doctor for some period.
What is the treatment for microstroke at home?
If the attack was caused by any chronic disease, then most of the medical therapy is aimed specifically at eliminating it. When the cause of an attack is an incorrect lifestyle, it is strongly recommended:
- Minimize stressful situations;
- Stop drinking alcohol and cigarettes;
- Normalize weight (this is also important for stabilizing blood pressure);
- Reduce the amount of salty, fatty or smoked foods you consume - nutrition after a mini-stroke should be healthy and balanced;
- Eat more fish, legumes, fresh herbs, fruits and vegetables;
- Normalize the work and rest schedule.
What to do with the consequences?
Memory impairment, general malaise, weakness in the arms and legs, difficulty swallowing, and sensory disturbances in the limbs are extremely rare consequences of several experienced transient ischemic attacks. It is also possible to develop depression and stuttering. Such conditions may require the intervention of not only doctors, but even psychologists and speech therapists.
Prevention
After a TIA, the risk of a stroke remains at 20%. Lifestyle correction protects against dangerous vascular problems in the brain. After a mini-stroke, you need to monitor your health more carefully:
- Engage in timely treatment of any diseases, including infectious ones.
- Monitor blood pressure and cholesterol levels and see a therapist and cardiologist.
- Monitor your blood sugar, take medications to regulate it as needed, and eat in accordance with your doctor’s recommendations.
- Take anticoagulants as prescribed by your doctor to reduce your risk of stroke. Discuss any problems you have with taking your medications with your doctor.
- Walk 10 thousand steps a day, lead a healthy lifestyle. Give up bad habits, reduce alcohol consumption to a minimum.
- Maintain a healthy weight. Excess body weight increases the risk of hypertension and is an independent risk factor for micro-strokes.
It is recommended to perform physical activities that raise the heart rate. You can calculate your heart rate for aerobic exercise using the formula: (210-age)x 0.6. Walking at a speed of 5-6 km/h is one of the methods of prevention if there are contraindications for running in the form of chronic heart disease. You can use an exercise bike, play table tennis, or simple exercises with a rubber expander.
Meals need to be balanced in favor of healthy fats, reduced sugar, increased fruits and fiber. Additionally, take omega-3 fatty acids in capsules, vitamin D3, vitamin E.
Stress factor is one of the most important factors identified in the pathogenesis of micro-strokes and heart diseases. The release of adrenaline causes the same spasm of blood vessels, disrupting breathing and blood supply to the brain. The only way to protect yourself from stress in a world filled with negative information is through affirmations and meditation. It is useful to “let off steam” after a stressful situation - use synthesized adrenaline for action, for example, going for a walk. To reduce spasm, breathing exercises help - correct diaphragmatic breathing. It involves expanding the lower ribs as you inhale and contracting the abdominal muscles as you exhale.
Why is it dangerous to have a mini-stroke on your feet?
Many people suffer a mini-stroke (and sometimes more than one) without seeking help from doctors. The consequences of such an attitude towards one’s own health are often tragic: a critical condition increases and turns into a massive stroke, after which only a few fully recover. Even short-term and mild signs (their totality) of an attack should be a reason for immediately contacting a doctor (calling an ambulance).
It is not at all necessary that after a mini-stroke a major stroke will occur: some people suffer several successive transient ischemic attacks without encountering a severe attack in the future. When performing a CT scan in such people, small numerous changes in the brain are detected, although nothing indicates a stroke. It is worth remembering that there is a direct connection between senile dementia and the number of transient ischemic attacks experienced.
Bibliography
- Astrakov S.V. Cortexin in neuroremediation practice / S.V. Astrakov. // Cortexin five years of experience in domestic neurology: collection. scientific Art. / under. ed. A.A.Skoromets. - St. Petersburg. : Science, 2005.-P. 83-92.
- Vilensky B.S. Stroke: prevention, diagnosis and treatment / B.S. Vilensky. St. Petersburg : Foliot, 2002. - 397 p.
- Medical informatics: textbook / V.I. Chernov et al. - Voronezh, 2004. 282 p.
- Neuroprotection in acute and chronic cerebrovascular insufficiency: collection. scientific Art. / ed. A.A. Skoromets, M.M. Dyakonova, St. Petersburg: Nauka, 2007. - 200 p.
- Ryzhak G.A. Cortexin and regulation of brain functions / G.A. Ryzhak, V.V. Malinin, T.N. Platonova. - St. Petersburg. : Foliot, 2003.
- S.K.Ternova, S.L.Arkhipov. // Current issues in neurology. -M., 1987.
Transient ischemic attack: symptoms and classification
Depending on the location of the cerebral vessel blocked by the thrombus, attacks can be divided into:
- transient ischemic attack in the vertebrobasilar region: diagnosed in 70% of cases;
- acute cerebral ischemia;
- transient attack in the carotid region
Symptoms and treatment for each type of attack may vary. The following distinctive features are characteristic of a vertebrobasilar attack:
- pain in the head is acute and localized in the back of the head;
- characterized by paralysis;
- the patient makes frequent movements of the eyeballs;
- Various visual impairments are characteristic: short-term blindness, simple visual hallucinations;
- Possible short-term memory loss.
Transient cerebral ischemic attack is usually detected in infants. Transistor microstroke has the most pronounced symptoms: the child sleeps poorly, he has tremors and nervous tics, natural reflexes are reduced, and dysfunction of muscle tone is often present.
Transient microstroke occurs in newborns due to oxygen starvation during pregnancy or childbirth. Treatment in infants depends on the severity of the disease, the specificity and severity of symptoms.
Consequences and treatment: prognosis
A favorable outcome of minor cerebral hemorrhage directly depends on the speed of timely detection of symptoms. Treatment must take place in a hospital under the constant supervision of doctors. In no case should you self-medicate or completely ignore the signs of an attack (their course can become chronic).
There is such a thing as a “silent stroke”; this is a major stroke that occurs in people who have previously suffered a transient ischemic attack. It is scary because no signs of an attack are observed, but disturbances in blood flow occur during this period, and irreversible negative processes occur in the brain cells.
Kinds
All types have one thing in common: blockage of blood flow to the brain. This causes big problems. Brain cells need oxygen, which enters the blood. So when a stroke cuts off its supply, cells begin to die. There are two types of microstroke:
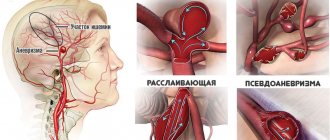
- Ischemic microstroke . Occurs as a result of an obstruction in the blood vessels supplying blood to the brain. The main condition for this type of obstruction is the development of fatty deposits lining the walls of the vessel. This is called atherosclerosis.
- Hemorrhagic microstroke . Hemorrhagic microstroke is also called intracerebral hemorrhage. Occurs when a blood vessel ruptures and blood accumulates in the tissue around the rupture. This puts pressure on the brain and causes blood loss in surrounding areas.
Immediate medical treatment is important to increase the chances of recovery. Prevention is also important. If you control your risk factors, you can significantly reduce the likelihood of any type of mini-stroke.