A stroke is an acute disorder of cerebral circulation. There are 2 main types of stroke - hemorrhagic and ischemic.
For ischemic stroke, the use of thrombolytic therapy is practiced.
Thrombolytic therapy involves dissolving the blood clot. The sooner administration of the drug for thrombolysis is started after the onset of ischemia, the more effective its result will be.
At the same time, the procedure has strict indications, and its use is limited by the possibility of developing complications from the use of thrombolytic agents.
The sequence of actions in case of stroke is described in Order of the Ministry of Health of the Russian Federation No. 928n “On approval of the procedure for providing medical care to patients with acute cerebrovascular accidents.” Thrombolytic therapy is carried out in the intensive care unit of the vascular center.
Types of drug thrombolysis:
- Selective - administration of the drug intra-arterially, immediately before the thrombus. Requires control by angiography.
- Non-selective - intravenous administration of the drug, its distribution throughout the body. Used more often.
Drugs can be administered either as a stream or intravenously.
Indications for the use of thrombolysis in ischemic stroke
Thrombolysis is the introduction of special thrombolytic drugs into the lumen of the artery, which are designed to dissolve the formed blood clot and thereby restore blood supply to the brain.
This procedure is based on the enhanced activation of plasminogen in the patient’s blood and its subsequent active transfer to the plasmin state. It is this substance that actively neutralizes the cross-links of all existing fibrin molecules, which ensures the integrity of the formed blood clot.
Indications for the thrombolysis procedure for stroke are:
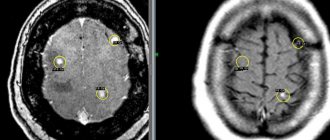
- Ischemic stroke confirmed by CT or MRI of the brain.
- The time interval between the onset of apoplexy and the patient’s admission to the hospital is no more than 4 hours.
- Carrying out a thorough diagnosis of the patient's body.
- The patient has no absolute contraindications to therapy.
Important: if thrombolysis is carried out incorrectly during a hemorrhagic stroke, it will lead to death due to increased bleeding due to the administration of drugs.
What is thrombolysis treatment
Everyone knows that a stroke is a very dangerous disease and is fraught with irreversible consequences for health. However, not everyone understands that even with an ischemic stroke of the brain, the outcome of the disease will largely depend on several basic nuances. Namely, from correctly selected treatment and, most importantly, surgical medical intervention.
The affected brain cells, even during a stroke, do not die immediately - in the area of the ischemic core they remain viable for at least another 6-8 minutes, while in the adjacent brain tissue the cells function for three to six hours, and in exceptional cases - up to several days inclusive. If blood circulation in the brain is restored during these periods of time, then the neurons will be able to return to normal. For this purpose, it is common practice in medicine to use thrombolysis.
Thrombolysis therapy is a procedure, the purpose of which is to introduce special medications into the damaged arteries of the brain that can quickly resolve the resulting blood clot and restore blood supply. Thanks to this technique, patients have a real chance of recovery. The main condition for thrombolysis is its use in the first hours after a stroke attack.
Thrombolysis Basics
Thrombolytic therapy for ischemic stroke is carried out subject to compliance with all of the principles and fundamentals listed below:
- Admission to the hospital of a patient with a suspected ischemic stroke no later than 2–3 hours from the onset of the stroke. Another hour is allocated for accurate diagnosis.
- The clinic has a special intensive care ward with all the necessary equipment.
- Carrying out all necessary diagnostic measures to make an accurate diagnosis.
- Examination of the patient by a neurologist and assessment of all body functions.
- Patient assessment using the NIH Stroke Scale. With a total score of 25 points on a given scale, thrombolysis is strictly contraindicated for the patient.
- Conducting general and biochemical blood tests for coagulability, glucose and other parameters.
- Slow introduction of thrombolytic drugs into the pool of a vessel blocked by a thrombus.
Important: with rapid administration of the drug, the patient experiences regression of one or more neurological factors. That is, cerebrovascular disorders appear. The patient may suffer from speech, vision, muscle tone, sensitivity, etc.
Depending on the possibility of localizing a blood clot in the vascular bed of the brain, doctors can use one of the types of thrombolysis:
- Selective (also local, catheter, intra-arterial). With this method of performing the procedure, the drug is injected using a catheter into the immediate area where the blood clot is located. The procedure lasts about two hours. All this time, the thrombolytic drug is slowly injected into the vessel under the control of cerebral angiography. That is, the doctor monitors the condition of the blood clot and blood vessels using x-rays. The selective method has a number of advantages: no need for tissue dissection, high accuracy and local impact on the thrombus. Due to the local administration of the drug, its dose is significantly reduced. This reduces the risk of additional bleeding.
- Systemic. It is used if the location of the blood clot cannot be determined. The medicine is administered into the vascular bed using a dropper. The drug acts throughout the bloodstream, dissolving all blood clots along the way. The duration of the procedure is about an hour. However, the risk of additional bleeding is too high due to the fact that the medicine works on a large scale, circulating through the bloodstream throughout the body.
Conditions for thrombolytic treatment
Treatment is always carried out in a hospital setting under the close supervision of a doctor. For this, the patient is placed in the vascular department, where there should be an intensive care unit or a neuro-resuscitation unit with all the necessary equipment.
The procedure is always carried out after a thorough diagnosis of the admitted patient. The main diagnostic measures are an MRI or CT scan of the brain, a blood test, transcranial Doppler sonography and a TCD examination.
A test for blood clotting and glucose levels is required, and if necessary, other important blood parameters are studied. In addition, the patient is examined using a stroke scale. If the sum of the points obtained on this scale is 25 or higher, then the procedure will be completely contraindicated for the patient.
After carrying out all the necessary diagnostic measures and laboratory tests, the doctor will be able to make a final diagnosis and choose the method of thrombolytic therapy.
The technique of the procedure boils down to slowly introducing the selected drug into the affected artery to resolve the blood clot. The thrombolytic agent can be administered intravenously or through a catheter. However, no matter what treatment technology the doctor chooses, the effectiveness will directly depend on his professionalism.
Thrombolytic drugs
When performing thrombolysis, the following thrombolytic drugs are most often used:
- "Anistreplase", "Tenecteplase" or "Metalise". Third generation drugs that can be injected into the vascular bed using the jet method.
- "Streptokinase" and "Urokinase". Old drugs that are used extremely rarely today. The consequences of taking such medications include severe allergic reactions in the body of a stroke victim.
- "Prourokinase." An effective and at the same time fast-acting drug. But in some cases it can provoke cerebral hemorrhage.
- Alteplase and Actilyse. Allows you to achieve a quick positive effect.
Contraindications to thrombolysis
It is worth knowing that thrombolysis has indications and contraindications for stroke. In this case, all contraindications are divided into absolute and relative. The absolute ones include:
- Hemorrhagic stroke (including subarachnoid).
- Minor symptoms of neurological disorders and rapid improvement in the patient’s condition.
- Repeated ischemic stroke.
- Coma.
- Detection of neoplasms, cysts, abscesses in the patient’s body.
- A history of cardiac arrest that occurred at least 10 days before the attack of apoplexy.
- Patient's history of epilepsy.
- Pathology of the cerebral veins, in which their connection is determined.
Relative contraindications for thrombolysis include the following conditions and pathologies:
- Varicose veins of the esophagus.
- History of surgical interventions performed within the last 14 days (including biopsy, puncture and other minimally invasive operations).
- The patient is on hemodialysis.
- Traumatic brain injuries suffered by the patient 3 months before apoplexy.
- Pregnancy, lactation period and two weeks after birth.
- Liver failure in the stages of compensation and decompensation.
- Renal failure is acute and chronic.
- Diathesis is hemorrhagic.
- Reduced blood clotting (hypocoagulation).
- An increase or decrease in blood glucose levels beyond the normal range.
- History of acute internal bleeding that occurred in the last 20 days.
In all these cases, the doctor assesses the patient’s condition and makes a decision to carry out manipulation or to prohibit it. The patient's relatives should be informed about the possible outcomes of thrombolysis performed against the background of relative contraindications.
If all the basics and principles of manipulation are observed, a favorable prognosis for the patient is guaranteed. It is only important to deliver the patient to the hospital on time and insist on an urgent examination.
Ischemic stroke belongs to the category of the most common vascular diseases of the brain and is a cerebral infarction. It has been clinically proven that in the first minutes after a cerebral stroke, only a small part of the brain, called the ischemic core, is subject to irreversible damage.
The remaining parts of the brain retain their viability and minimal functioning for some time.
- All information on the site is for informational purposes only and is NOT a guide to action!
- can give you an ACCURATE DIAGNOSIS !
- We kindly ask you NOT to self-medicate, but to make an appointment with a specialist !
- Health to you and your loved ones!
That is why it is very important to make all possible attempts to restore normal blood circulation in the damaged brain tissue as soon as possible.
One of the most effective and efficient methods is considered to be thrombolytic therapy, the main idea of which is to restore normal blood circulation and dissolve the blood clot or atherosclerotic plaque that caused the blockage of the vessel.
The use of thrombolysis for ischemic stroke requires strict implementation of a number of organizational measures:
- Hospitalization of post-stroke patients as quickly as possible.
- In the first 2-3 hours after the development of an ischemic stroke, it is necessary to carry out all the necessary diagnostic studies, since thrombolysis is carried out only after a complete diagnosis of the patient’s condition. As a rule, the VMP protocol is most often used for this purpose - this is a kind of referral to highly qualified medical care.
- For post-stroke patients, special intensive care wards with all the necessary equipment are required.
The essence of this type of therapy is that a special drug is delivered into the vessel through a dropper, which promotes the effective dissolution of a blood clot or atherosclerotic plaque.
Timely thrombolytic therapy is an opportunity not only to save the life of a person in a post-stroke state, but also to restore hope for complete rehabilitation and a return to normal life.
Complications
Thanks to the use of third-generation thrombolytics, the incidence of complications from thrombolytic therapy has decreased. But they are possible, about which the patient and his relatives should be notified in advance:
- hemorrhagic penetration into the focus of ischemic stroke, or the formation of hemorrhage;
- bleeding in another organ: from the veins of the esophagus, hemorrhoids;
- allergic reaction - up to anaphylaxis.
Due to the risk of developing dangerous complications, the percentage of thrombolysis remains small. An alternative to such therapy may be instrumental removal of the clot using a retriever, or exposure of the clot to ultrasound. In the latter case, 2 MHz waves are applied to the area of the affected vessel for several hours after the development of an ischemic stroke.
Mortality from cardiovascular diseases is in first place worldwide. In addition, the percentage of social and everyday maladaptation among stroke survivors is high. Therefore, it is extremely important to immediately seek medical help at the first signs of acute cerebrovascular accident.
Basics of therapy
As mentioned above, thrombolytic therapy should be carried out no less than 3 and no more than 6 hours after the onset of an ischemic stroke. Timely thrombolysis helps to quickly dissolve the blood clot in the affected vascular area and return blood flow to normal.
How does thrombolysis work?
Rapid injection of a special thrombolytic into the pool of a blocked vessel leads to regression of neurological factors, which may include speech disorders, as well as numbness of certain parts of the body.
The essence of this procedure is that the thrombolytic activates the finrinolytic abilities of the blood, which becomes possible due to the degeneration of ordinary plasminogen into its active form, which is called plasmin.
For quite a long period of time in medicine, there was one possible type of thrombolytic therapy, the essence of which was the intravenous administration of a special drug to a patient in a post-stroke state. The administration of the thrombolytic drug was carried out through a dropper.
Today, several modern types of thrombolysis can be distinguished:
In addition to the fact that in medicine, thrombolysis is classified into types, it is also possible to differentiate the procedure depending on the method of its implementation.
Today, thrombolytic therapy is performed by two main methods:
- The essence of this method is the local administration of the drug directly into the area where the blood clot is located, clogging the blood vessel.
- This method is also called the catheter method, as it is performed by administering a thrombolytic medication through a catheter.
- This method is used in cases where it was not possible to reliably determine in which blood vessel the thrombus is located.
- The drug is injected into a vein and spreads throughout the circulatory system, removing and dissolving all blood clots and atherosclerotic plaques in the vessels.
- The dosage of the drug used during the systemic method of thrommolysis increases markedly, which can lead to the most unpleasant consequences for the general condition of the patient in the post-stroke state.
The symptoms of an incoming stroke can be confused with a hypertensive crisis, so it is important to know the small nuances, which you can read about in the link.
To dissolve blood clots and atherosclerotic plaques that block blood vessels, certain medications called thrombolytics are used.
The main and most commonly used drugs for thrombolysis in stroke can be identified:
What is thrombolytic therapy?
Ischemic stroke usually occurs due to an intravascular thrombus obstructing cerebral blood flow.
After the onset of stroke, neurons surrounding the ischemic core may remain viable for a certain period of time.
The destruction of brain cells after ischemia occurs gradually, and restoration of blood flow through early correction can save damaged neurons.
Blood clots blocking cerebral blood flow can be lysed (dissolved). Thrombolysis (thrombolytic therapy) is carried out by dissolving blood clots (thrombi) blocking a blood vessel using thrombolytic drugs.
Thrombolysis is a type of pharmacological therapy aimed at restoring blood flow in a vessel by dissolving a blood clot under the influence of various agents inside the vascular bed.
Thrombolysis for acute ischemic stroke is a key intervention that can reduce disability.
Thrombolytic therapy is carried out by injecting alteplase (g-TPA), a substance belonging to the group of thrombolytic agents, into the patient’s veins.
Alteplase works by converting inactive plasminogen to the active form plasmin, which promotes thrombolysis of fibrin by breaking it down.
The lysis procedure is performed by injecting 0.9 mg of alteplase (g-TP) into the patient’s bloodstream per 1 kilogram of the patient’s weight over 60 minutes (but not more than 90 mg), with 10% given as a bolus.
There are two types of thrombolysis aimed at freeing a blocked vessel from a blood clot.
Thrombolysis using thrombolytic agents
- Eminase (Anistreplase);
- Retavaz (Reteplase);
- Streptase (Streptokinase, Cabikinase);
- tPA (a class of drugs that includes Activase);
- Tenecteplase;
- Abbokinase, Kinlitik (Urokinase).
Depending on the pattern of stroke development, the doctor may choose one of the listed drug treatment options.
The drug is usually given through a long catheter that is threaded into the blood vessel directly to the site of the clot to deliver the drugs directly to the site of the blockage.
During thrombolysis, the doctor uses X-ray tomography to see the result of the dissolution of the blood clot. If the clot is relatively small, the lysis process may take several hours. A severe blockage may take several days to heal.
WHO has announced an increase in the number of people suffering from epilepsy after a stroke. Why do seizures develop after an attack? Let's try to figure it out.
Everyone should know how to prevent a stroke. This information is important for everyone.
What is a migraine stroke and how dangerous is it? If you often suffer from migraines, then this article is for you.
Mechanical thromboembolism
Doctors may also choose another type of thrombolysis called mechanical thromboembolism.
During this procedure, a long catheter that has a tip with a small cuff and a rotating device is inserted into the blood vessel.
A high-speed jet of liquid or ultrasonic radiation is used to physically destroy a blood clot.
Indications for thrombolysis in stroke
As with each treatment method, thrombolytic therapy has its own indications.
Such indications include:
- The main indication for thrombolysis is a confirmed diagnosis of ischemic cerebral stroke.
- This type of therapy is prescribed to patients aged at least 18 and not older than 80 years.
- An extremely important indication is the fact that no more than 3-6 hours have passed since the onset of the ischemic stroke. It is in such cases that thrombolysis may be the most effective treatment for this disease.
- Before prescribing thrombolytic therapy, a computed tomography scan of the head is required. The procedure is prescribed exclusively in cases where there is no hemorrhage in the brain area.
You can learn about the treatment and prevention of chronic cerebral ischemia here.
A list of vitamins after a stroke and reviews about them are listed here.
Contraindications
Just like the indications, thrombolysis for ischemic stroke also has a number of significant contraindications that must be taken into account:
- One of the most important contraindications when performing thrombolysis for the treatment of stroke is the presence of cerebral hemorrhage, which can be determined by the results of a computed tomography scan of the head.
- Rapidly regressing neurological deficit.
- Clinical improvement of the patient’s condition immediately within 3-6 hours after an ischemic stroke.
- Behavior of severe surgical treatment during 3-4 months before stroke.
- Pregnancy, lactation period.
- Chronic liver diseases, a history of arterial aneurysm.
- Risk of aortic dissection as a result of thrombolysis.
Ischemic stroke is a serious pathology that threatens many complications. This disorder occurs quite often, and in most cases it is caused by vascular occlusion, that is, blockage by a blood clot. Thrombolysis can solve this problem. This technique is also called thrombolytic therapy.
What is thrombolysis? Thrombolysis methods
Thrombolytic therapy involves the administration of special drugs that dissolve blood clots. This procedure is recommended to be carried out in a specialized vascular department equipped with an intensive care unit or a neuro intensive care unit.
Thrombolysis can be carried out selectively or systemically. The first option is also called local. Selective therapy is a complex technique. They resort to it only if it is impossible to perform systemic thrombolysis. The drug must be injected directly into the area where the blood clot is located.
The systemic method means intravenous administration of the drug. The bloodstream carries it throughout the vascular system, dissolving existing clots. This option is effective when specialists were unable to determine the exact location of the blood clot.
During thrombolysis, the patient receives a loading dose of the drug, which quickly destroys the blood clot that has blocked the lumen of the vessel in the brain. The drug continues to flow through the drip, completing the process of destroying the blood clot and maximally restoring the patency of the artery.
Thrombolytic therapy is a highly effective technique, but it is permissible for use only with a clearly established diagnosis. Specialists must determine with 100% accuracy that the patient has an ischemic stroke. In this case, the picture must meet the following conditions:
- diagnosed ischemic stroke causing a clear neurological deficit;
- no more than 3-6 hours have passed since the initial signs of stroke appeared;
- The patient's blood pressure does not exceed 180/110 mm Hg. Art.;
- the patient has not undergone thrombolysis during the last six months;
- there are no erosive and ulcerative lesions of the gastrointestinal tract (can be a source of bleeding);
- There are no pathological conditions characterized by increased bleeding (hemorrhagic rash, coagulopathy).
To make an accurate diagnosis and confirm the absence of contraindications, the patient must undergo diagnostics. It includes computed tomography or magnetic resonance imaging. Thrombolysis can be performed on patients aged 18-80 years.
Non-drug treatment
For ischemic stroke, non-drug treatment is also carried out, which consists of the following:
- The patient must be taken to the hospital as soon as possible, preferably within the first three hours from the moment of the attack. This must be a stroke center or a neuralgia department.
- The patient is placed in an intensive care unit or undergoes intensive care unit as indicated.
- Monitoring of all vital functions.
- The patient is provided with bed rest for a couple of days with gradual verticalization.
- If necessary, restore patency of the airways.
- Ventilation as needed and indicated.
- Dietary regimen:
- the first couple of days, all food should be boiled and pureed, so that it is easier for the body to digest and assimilate;
- the amount of fat consumed is reduced to a minimum, this applies not only to animal fats, but also to vegetable fats;
- minimize the amount of salt to 3 grams per day;
- the amount of complex carbohydrates and fiber should prevail in the diet;
- vegetables and fruits are 1/3 of the diet;
- fried, smoked, salty foods are prohibited;
- bread made only from wholemeal flour and bran.
Doctors strongly recommend that all patients who are prone to any type of stroke lead a healthy lifestyle. This includes proper nutrition, regular exercise, spending more time outdoors, and giving up bad habits. It is important to have regular medical examinations.
It will help to identify at an early stage any pathology or disease that can trigger the occurrence of ischemic stroke. In addition, the doctor will prescribe medications that will have a preventive effect on blood vessels and prevent the formation of blood clots.
Ischemic stroke is a serious pathology that occurs as a result of weakening or complete cessation of blood circulation in one of the areas of the brain. The most common cause of this condition is blockage (occlusion) of blood vessels by a blood clot.
To eliminate it, thrombolysis is used - the introduction of special drugs that dissolve blood clots. We will talk about the essence of thrombolytic therapy, its types, features, indications and contraindications below.
Drugs prescribed for thrombolysis
For thrombolytic therapy, thrombolytic drugs are used. They are also called plasminogen activators or thrombolytic agents. There are several groups of such drugs:
- I generation. This group includes Streptokinase and Urokinase.
- II generation, including Actilyse (Alteplase), Prourokinase.
- III generation, including Metalyse (Tenecteplase), Reteplase, Anistreplase.
Sterptokinase is rarely used in modern medicine due to its significant drawback - incompatibility with the human body. This factor means a high risk of allergic reactions. Urokinase rarely causes allergic reactions. Sterptokinase must be administered over an hour, and the use of Urokinase involves intravenous heparin.
Actilyse must be used within the first 4-5 hours. The effectiveness of therapy directly depends on the time of its initiation. The dosage of the drug is calculated based on the patient’s weight - 0.9 mg per 1 kg, but not more than 90 mg. First, 10% of the required dose is injected by stream, the rest is infused over an hour. If the indications do not require it, then heparin is not administered to the patient. Compared to Streptokinase, Actilyse provides higher patient survival rates.
Prourokinase is optimally used within 6 hours after the first manifestations of a stroke, but therapy is also allowed within the first 12 hours. The dosage is calculated similarly to Actylase, bolus administration. The drug is based on DNA-recombined kidney cells from human embryos. Prourokinase can be glycosylated or non-glycosylated. The first option is attractive due to its faster onset of action.
III generation thrombolytics are attractive due to the possibility of jet administration. Methylase is administered once for no more than 10 seconds. The dosage of the drug is calculated based on the patient’s body weight, and the volume of the prepared solution depends on it. If you weigh up to 60 kg, you must administer 30 mg of the drug, that is, 6 ml of solution. If the weight is 80-90 kg, then you need 45 mg of the drug, which is 9 ml of solution. The effectiveness of therapy is increased by the administration of heparin and acetylsalicylic acid.
Reteplase is used in 2 doses. The injection is given within 2 minutes, repeated after half an hour.
Anistreplase is represented by a tandem of Streptokinase and plasminogen. This complex provides a quick effect on the blood clot. The drug is administered once at a dose of 30 units over 2 minutes.
Thrombolysis for ischemic stroke has many side effects. The most common complication is bleeding. The risk of such consequences is reduced with the use of fibrin-specific agents.
Contraindications
Thrombolytic therapy is not allowed for all patients. The list of contraindications for this treatment is quite wide.
It is not performed if the patient:
- recurrent stroke;
- blood pressure exceeds 185 mm Hg. Art. in systole and 110 mm Hg. Art. by diastole;
- there is an abscess or tumor in the brain;
- cardiac arrest was observed before illness (a 10-day period is taken into account);
- blood glucose level does not fall within the range of 2.8-22.2 mmol/l;
- hemorrhagic rash;
- vascular malformations;
- reduced coagulation properties of blood;
- there was an epileptic seizure before the stroke;
- serious problems with the liver or kidneys;
- within the last 3 months there has been a severe head injury or cranial vault injury;
- Surgery was performed within 2 weeks;
- I have had internal bleeding for the past 20 days.
Thrombolysis is contraindicated in pregnant women and breastfeeding women. For the first 2 weeks after birth, such treatment is prohibited.
If cerebral circulation is slightly impaired or the patient’s condition has improved, then thrombolytic therapy is not required.
There are also a number of relative contraindications. If they exist, the decision on the possibility of therapy is made by a specialist. This is necessary in the case of large-scale burns, bone fractures, acute pericarditis, infective endocarditis and a number of other pathologies.
Thrombolytic therapy after ischemic stroke is effective, but should be carried out only in the first hours after the initial signs of pathology appear. This treatment has quite a few contraindications, so before starting it it is necessary to conduct a number of studies.
Thrombolysis for ischemic stroke is carried out to restore blood flow through the vessels of the brain. The action of the drugs administered during the procedure is aimed at destroying the blood clots that caused the development of the pathology.
Diagnostics
Thanks to the fact that medicine does not stand still, all diagnostic measures do not take much time. This allows thrombolysis to begin in the first hours after an ischemic stroke. Diagnostic measures are usually divided into basic and additional. Usually the first results are sufficient, but there is no need to exclude cases when additional procedures are indispensable.
Standard or basic diagnostic measures include:
- general blood analysis;
- checking blood glucose levels;
- checking cholesterol using both general and structured analysis;
- blood test for electrolyte levels;
- checking liver transaminases and total and direct bilirubin;
- analysis of urea, creatinine, total protein;
- coagulogram;
- OAM, ECG;
- 24-hour CT, MRI, ultrasound.
Additionally, they may assign:
- checking antinuclear factors of antibodies to lupus anticoagulant, cardiolipins, etc.;
- analysis of proteins and protein fractions;
- CPT and troponin test;
- blood testing for sexually transmitted diseases and HIV;
- arterial MSCT or MRA;
- EEG;
- X-ray;
- Ultrasound or Doppler Doppler of the peritoneum, kidneys;
- lumbar puncture.
Indications for use
Thrombolysis for stroke is advisable only for the following indications:
- The first signs of pathology were detected no earlier than 3 hours ago.
- There is a history of operations performed within the last 3 months.
- Thrombosis formed in the cerebral artery. Cerebral infarction caused by cerebral artery embolism.
Contraindications
The procedure cannot be performed if the patient has the following contraindications to thrombolysis:
- bleeding of any nature, including in the gastrointestinal tract;
- pressure above 185/110;
- tumors in the brain, foci of inflammation and purulent abscesses;
- aortic dissection;
- according to indicators, the possible development of recurrent strokes;
- interruptions in the functioning of the heart muscle;
- epilepsy attacks;
- any operations, regardless of their complexity, performed within 2 weeks before the development of pathology;
- fresh head injuries, bruises that damaged the brain;
- any trimester of pregnancy and the entire period of breastfeeding;
- 2 weeks after birth;
- impaired functioning of the kidneys and liver;
- glucose levels are higher or lower than normal;
- platelets less than 100,000.
Ignoring any contraindication may negatively affect the treatment process, causing complications.
How does the procedure work?
The clinic must have conditions for conducting computed tomography or magnetic resonance imaging, as well as a clinical laboratory for prompt testing, because in the event of a stroke, every minute can be decisive.
To accurately determine the location of the thrombus, transcranial Doppler sonography is recommended. After the procedure, re-occlusion of the blood vessels may occur, so it is necessary to monitor the patient’s condition and take the necessary measures in a timely manner aimed at eliminating the consequences of the stroke.
During the procedure, the patient's blood pressure is measured every 15 minutes, which should not be higher than 180/110. In the next 6 hours, blood pressure is monitored once every 30 minutes, and until the end of 1 day - every hour. This indicator is the main one in the treatment of stroke. Important indicators are monitored within 24-36 hours so that complications do not develop and recovery is more efficient.
There are 2 ways to administer drugs for thrombolysis:
- Systemic. Thrombolytics are infused intravenously and circulate through the vessels along with the bloodstream, destroying the structure of blood clots. It is used if there is no accurate information about the location of the blockage, and no more than 4 hours have passed since the onset of the stroke. It is carried out only after a complete examination, but this wastes time and reduces the number of living cells capable of recovery.
- Selective. This method has been little studied. The drug is injected close to the blood clot. It is carried out if it is not possible to perform systemic thrombolysis. It is used for severe circulatory disorders in the vessels of the brain that occur within 6 hours from the onset of a stroke. Leads to serious consequences if contraindications are not taken into account. The outcome can be fatal.
Therapy is not carried out in an emergency setting, because it is necessary to determine the type of pathology (ischemic or hemorrhagic), the place where the blood clot has blocked the vessel, and this is only possible in the clinic. For hemorrhagic stroke, treatment is different, and thrombolysis is contraindicated in this case.
Thrombolysis for ischemic stroke (thrombolytic therapy, TLT) allows you to restore blood flow in the affected vessels of the brain and reduce the area of damage, and subsequently minimize the consequences of a stroke and prevent disability in patients. Thrombolytic therapy is a high-tech type of medical care (HTMC) and is carried out according to the HTMC protocol.
The symptoms of a stroke vary. The patient may be bothered by a headache, then, depending on the place where cerebral ischemia occurred (oxygen starvation of brain tissue due to obstruction of the lumen of a cerebral vessel by a thrombus), speech impairment, memory loss, dizziness and unsteadiness of gait, weakness in the limbs on the left or on right.
Previous uncontrolled hypertension and heart rhythm disturbances play a major role in the development of ischemic stroke. uncontrolled diabetes mellitus (with blood glucose levels elevated above normal).
Thrombolysis for stroke is carried out according to strict indications. The diagnosis of ischemic stroke must be made using a neurological examination and computed tomography and differentiated from other diseases that have similar symptoms.
The victim must be between 18 and 80 years old. From the onset of the disease until the patient arrives at the hospital where such treatment is carried out, no more than 3 hours should pass.
Contraindications
Thrombolytic therapy has contraindications:
- more than 3 hours have passed from the onset of the first symptoms to the patient’s arrival at the hospital;
- the patient is taking anticoagulants (warfarin) or thrombin inhibitors (Xarelto, Pradaxa);
- the patient suffers from diabetes mellitus type 1 or 2;
- cirrhosis of the liver;
- history of bacterial endocarditis;
- there is an indication in the anamnesis of the presence of hemorrhagic diathesis;
- CT or MRI results revealed intracranial hematomas, arteriovenous malformations, intracranial tumor formations;
- myocardial infarction in the last 3 months;
- pregnancy or the first 10 days after birth.
The essence of therapy
Thrombolytic therapy allows you to quickly destroy and remove the blood clot from the brain vessels that led to the development of a stroke. Thrombolysis can be systemic or local.
The method of thrombolysis and the dosage of the thrombolytic drug depend on various factors. With systemic thrombolytic therapy, the thrombolytic is administered intravenously; it is carried throughout the body through the bloodstream, dissolving blood clots. The disadvantage of this method is the high risk of bleeding.
Local thrombolytic therapy for ischemic stroke is carried out in the operating room by an x-ray surgeon under the supervision of ultrasound and angiography. Using a catheter, the thrombolytic drug is injected directly into the vessel with the thrombus located in it. This requires a small amount of the drug and reduces the risk of bleeding.
Thrombolytic drugs
There are 2 groups of thrombolytic drugs for TLT. The drugs of the first group include streptokinase, its disadvantage is a large number of hemorrhagic complications in patients. The drug of the second group (more modern, created using genetic engineering) is alteplase, the risk of bleeding and allergies when using it is low.
The thrombolysis method helps to avoid the tragic consequences of cerebral ischemia. The main thing is not to miss
Our expert is the head of the department of diagnosis and therapy of stroke, assistant of the department of fundamental and clinical neurology of the Russian State Medical University and the Research Institute of Stroke of the Russian State Medical University, candidate of medical sciences Nikolai Shamalov .
In Russia today, the mortality rate from stroke is almost twice as high as in the West, where only 10–20% of diseases are fatal. The technique of thrombolysis (intravenous administration of drugs that dissolve blood clots) has long been used abroad. This is an effective method of treating stroke, which provides the fastest and most complete restoration of impaired neurological functions. Today, thrombolytic therapy is also available to Russians. One thing is that the therapeutic “window” during which thrombolysis can be resorted to is only three hours, counting from the onset of the disease. That is why it is extremely important not to miss the first symptoms of the disease.
Video on the topic
The most common disease associated with cerebral vessels is ischemic stroke. This cerebral infarction affects only a part of the cells irreversibly and only in the first minutes.
The remaining cells can function minimally and be active for a certain time, insignificant, but sometimes sufficient to save a person without losing his ability to work.
Thrombolytic
therapy for ischemic stroke, according to doctors,
is
the only opportunity for such patients to minimize the consequences of a stroke and prevent it from developing further. Is it so?
There are restrictions
You can suspect something is wrong based on the following sudden signs:
- weakness or numbness in the extremities on one side (for example, in the left arm and leg);
— distorted face (numbness of half the face);
- speech disorder (unintelligible speech, feeling of “porridge in the mouth”, complete loss of the ability to speak).
Despite the fact that the method itself is technically simple - the patient is given an IV with special medications for an hour - it can only be carried out after careful research. The fact is that in addition to time restrictions, there are other contraindications. For example, thrombolysis cannot be used if the patient underwent any surgical operations shortly before the stroke. In addition, this method can only be used for ischemic stroke, whereas in the hemorrhagic form of the disease it only worsens the situation. Therefore, thrombolytic therapy is carried out only after a computed tomography scan has been performed to exclude the presence of hemorrhage.
The method gives good results, but sometimes, unfortunately, leads to complications. One of them (occurs in 6–8% of cases) is the transition of an ischemic stroke to a hemorrhagic form (vessel hemorrhage). The risk of such complications is higher the more time has passed since the onset of the disease.
However, today an alternative method has emerged - selective thrombolysis, which allows you to help the patient within six hours after the onset of a stroke.
In this case, the medicine is administered to the patient not intravenously, but through a puncture of the femoral artery, from where a microcatheter delivers the medicine to the cerebral artery.
History and more
The procedure and selection of the necessary thrombolytics begin with diagnostics, which are prescribed after studying the patient’s complaints and medical history. These include:
- Transient and monocular blindness.
- Any heart pathologies.
- Diagnoses of “angina pectoris” or “ischemia of the lower extremities”.
- Severe fatigue after waking up, taking a bath with hot water, or minor physical activity.
- Signs of development of neurological symptoms.
- Age from 50 years.
In cases where neuralgic symptoms become focal and begin to predominate over the brain, thrombolysis will be prescribed. Most often this is:
- headaches accompanied by dizziness;
- unsteady gait and staggering;
- critical violation of facial symmetry;
- slurred speech;
- clouding of consciousness;
- tremor, weakness and numbness of the arms and legs;
- convulsive type seizure;
- disturbance of visual, auditory, respiratory function;
- vomiting and nausea;
- rapid heartbeat and heart pain;
- temperature.