Symptoms of inflammation of the maxillofacial nerve and treatment methods
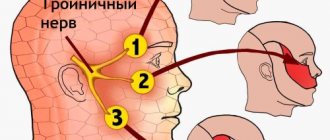
The trigeminal nerve is divided into 3 branches: orbital, maxillary and mandibular. The first runs along the organs of vision. The maxillary nerve innervates areas in the upper jaw. It is also responsible for sensitivity on the outer and inner sides of the nasal sinuses.
The mandibular nerve carries signals from the brain to the chin and lower jaw. This branch, unlike the first, has motor fibers. Neuritis of both sections, which causes acute pain, due to the peculiarities of its location, quite often develops due to inflammation of the tissues of the oral cavity.
Anatomy
The trigeminal nerve, which includes the maxillary and mandibular branches, contains motor and sensory nuclei. The maxillary nerve is divided into three branches:
- infraorbital;
- nodal;
- zygomatic
The infraorbital branch is considered the most powerful branch of the maxillary nerve. It is its direct continuation and, passing under the eye along the groove, reaches the canal in the canine fossa. Here it is divided into branches that innervate:
- lower eyelids and skin around the corner of the eyes;
- the inner and outer parts of the nasal passages;
- skin and mucous membrane of the upper lip, wings of the nose;
- the area near the upper teeth, including the large molars.
Four branches of the maxillary nerve are responsible for the innervation of the teeth of the upper jaw, each of which ensures the transmission of impulses to a strictly defined zone (incisors, canines, small and large molars). These parts in the area of the nasolabial triangle form a rather large knot. Fibers extend from it, providing innervation to the gum tissue.
The nodal branches are represented by several short processes that run along:
- upper sky;
- pharynx (behind the trunk of lingual nerve fibers);
- bottom of both eyes;
- medial and lateral sides of the nasal sinuses.
The nodal branch, connecting its ends with the facial nerve, runs along the bottom of the eye and stops in the cheek, temple and forehead. This section provides exceptionally sensitive perception.
The anatomy of the mandibular nerve is more complex. The mandibular nerve exits the cranial cavity through the foramen ovale and stretches towards the temporal plexus. Here it is divided into sensory and motor fibers.
The sensitive part of its branches is divided into:
- auriculotemporal;
- buccal;
- lingual;
- lower lunulae.
The auriculotemporal region innervates:
- parotid salivary gland;
- temporomandibular joint;
- part of the temple, ear canal and eardrum.
The buccal branch transmits impulses to the mucous membrane on the inside of the cheek and the corner of the mouth, and the lingual branch - to:
- anterior two-thirds of the tongue;
- sublingual and submandibular salivary glands;
- mucous membrane at the bottom of the mouth;
- pharynx;
- palatine tonsils.
Alveolar nerve fibers running in the mandibular canal innervate the gums and teeth. Also, this branch extends beyond the oral cavity and transmits impulses to the lower lip and chin.
The motor portion of the mandibular nerve is represented by fibers that provide innervation to the muscles responsible for chewing, tension of the tympanic membrane and palatine curtain, and jaw movement.
Reasons for violation
Damage to nerve fibers in this area is caused by:
- diseases of the oral cavity (gingivitis, periodontitis and others);
- unsuccessful oral surgery, including tooth extraction;
- severe hypothermia of the front part of the head;
- stress.
Pinching of the jaw nerve is caused by tumors that grow both in the oral cavity and in other parts of the skull in the areas where this branch runs.
Less commonly, neuralgia of this form occurs against the background of:
- acute infectious processes in the body;
- multiple sclerosis, the course of which is accompanied by destruction of the myelin sheath of nerve fibers;
- inflammation of the salivary gland;
- tuberculosis.
Quite often, after nerve removal, the jaw hurts. This phenomenon in most cases is temporary and is caused by damage to local tissues.
Symptoms
With inflammation of the submandibular nerve, symptoms are usually determined depending on the location of the pathological process. In most cases, acute pain occurs, which radiates along the affected fibers. But when the maxillary nerve is pinched, the symptoms may differ from the manifestations of mandibular neuralgia.
Traditionally, in addition to pain, the patient with neuritis decreases or increases the sensitivity of a particular part of the face.
Uneven contraction or tonic tension (spasm) of local muscle fibers is possible.
Signs of inflammation of the upper jaw
When the nerves of the upper jaw are damaged, sensitivity in the area decreases:
- maxillary sinus;
- upper cheek;
- lower eyelid;
- outer corner of the eye;
- side of the face;
- oral mucosa on the upper jaw;
- upper jaw.
The intensity of pain when nerves and jaw are damaged depends on the characteristics of the disorder. This symptom is acute and aching in nature. The pain may spread towards the eye, indicating damage to the entire trigeminal nerve. Also, with this localization of the pathological process, tic of the lower eyelid is often observed.
Signs of inflammation of the lower jaw
With inflammation of the mandibular nerve, symptoms appear as:
- decreased sensitivity in the area of the lower jaw and chin;
- paresis or paralysis of the muscles that provide chewing function;
- facial asymmetry.
If the nerves of the lower jaw are affected, the patient experiences increased sensitivity of the hard tissue and mucous membrane to food or palpation.
Such susceptibility is observed both along the entire length of the affected fibers and in the following areas:
- gums;
- teeth;
- mandibular bone;
- language;
- sublingual area.
If paresis or paralysis develops, then a weak bite and the inability to pull the lower jaw upward are of concern. Due to the latter disorder, the patient's mouth remains constantly open.
Diagnostics
If damage to the mandibular nerve is suspected, an external examination of the patient and palpation of the problem area are first performed. This form of neuritis is indicated by the inability to close the jaws, muscle spasms, and painful sensations that occur when touched.
Additionally, CT, MRI and electromyography are performed. The first two methods help determine the causes of neuritis and identify the localization of the pathological process, the latter assesses the degree of conductivity of nerve fibers and allows you to differentiate neuralgia from other pathologies that have similar symptoms.
Treatment methods
Treatment tactics are selected based on the characteristics of the causative factor. Drug therapy is mainly used, the effect of which is aimed at relieving the symptoms of the disease and eliminating inflammation, including pain relief.
Traditional therapy
If the maxillofacial nerve is damaged, painkillers are used at the beginning of treatment:
- "Clonazepam";
- "Nimesil";
- "Ibuprofen";
- "Gabapentin";
- "Carbamazepine" and others.
If treatment of neuritis with analgesics does not produce a positive result, then narcotic medications are prescribed. In severe cases, trunk anesthesia is performed, in which anesthetic medication is injected directly into the affected area.
Treatment for neuritis of the submandibular nerve is determined taking into account the symptoms and characteristics of the provoking factor. Broad-spectrum antibacterial drugs are used in therapy. Additionally, antiherpetic medications are prescribed, and B vitamins are prescribed to restore nerve conduction.
Traditional medicine treatment
Neuralgia of the submandibular nerve fibers cannot be treated using traditional medicine. Such treatment is used only in consultation with a doctor to relieve concomitant symptoms. Helps reduce the intensity of pain:
- chamomile or hibiscus tea;
- bay oil;
- beet juice;
- aloe juice (taken orally);
- compresses from decoctions of fresh wormwood or marshmallow root.
Neuritis is also treated using physiotherapy methods: electro- and phonophoresis, UHF and others. Massaging the affected area during an exacerbation is prohibited.
Forecast
The prognosis for inflammation of the mandibular or maxillary nerves directly depends on the characteristics of the causative factor.
Neuralgia caused by injury usually responds well to treatment.
But if the disease is caused by metabolic disorders in older people, chronic diseases or severe infectious pathologies, then it is not possible to completely get rid of pain in the facial area. Neuralgia in such cases periodically recurs.
Source: https://bereginerv.ru/patologii-nervov/zashhemlenie-chelyustnogo.html
Neuralgia of the submandibular and sublingual nodes
Neuralgia of the submandibular and sublingual nodes is a pain syndrome that is accompanied by attacks of acute burning pain in the tongue, mucous membranes of the oral cavity, sublingual and submandibular zones. Pathology refers to organic diseases of the vegetative nodes of the face. Diagnosis is carried out by a neurologist using topical methods and diagnostic blockades.
The content of the article:
The disease can be unilateral or bilateral.
Often the pathology has a chronic form, which is accompanied by paroxysmal pain attacks lasting up to 1 hour, impaired salivation, soft tissue swelling and reflex pain in nearby nodes on the face, neck, occipital and temporal region, in the upper chest and arm on the side of the pathology. In 96% of cases, neuralgia of the sublingual and submandibular ganglia is observed on one side and only in 4% - bilateral.
Treatment of affected sublingual and submandibular nodes includes a whole range of measures from sanitation and elimination of foci of infection with the help of drug therapy, therapeutic blockades, physiotherapeutic methods to surgical interventions if necessary.
Therapy should correspond to the degree of spread of the disease, the nature and frequency of pain attacks, the condition of the surrounding tissues, tongue, sublingual and submandibular zones.
The means and methods that will be used for therapy are determined by a neurologist in consultation with other specialists.
Causes of neuralgia of the submandibular and sublingual nodes
The following factors can provoke the development of neuralgia of the submandibular and sublingual nodes:
- physical impact - prolonged or regular hypothermia of the ganglia;
- chronic inflammatory processes in the oral cavity - stomatitis, multiple caries, gingivitis, periodontitis;
- infectious pathologies - viral diseases, sepsis, syphilis, tuberculosis;
- chronic diseases of the digestive system and pelvic organs;
- negative consequences of surgical interventions - removal or prosthetics of teeth;
- foci of infection in nearby organs - sore throat, otitis media, sinusitis.
Often neuralgia can appear due to intoxication of the body with poisons, salts of heavy metals, and low-quality alcohol. It can also develop against the background of allergic and endocrine diseases, and be one of the manifestations of hypovitaminosis.
Symptoms of neuralgia of the submandibular and sublingual nodes
The first manifestations of the disease will be paroxysmal pain (paroxysms) on the side of the inflamed ganglia. The duration of a painful attack varies from several minutes to an hour.
The pain syndrome is characterized by intensity and pulsation in the area of localization of the affected ganglia. A distinctive feature of most vegetative ganglionitis of the face and head is a tendency to expand pain.
The stronger and more advanced the inflammatory process, the more extensive areas are affected by pain during paroxysm.
Attacks begin from the inflamed node in the area of the root of the tongue and tonsils, then the pain spreads and occupies increasingly larger areas - over the entire half of the head, neck, collarbone, shoulder and arm. The occurrence of pain can be triggered by tension in the facial muscles and thermal effects, that is, during a conversation or eating hot, spicy food.
Neuralgia of the submandibular and sublingual nodes is divided into two stages:
- The initial ganglioneuralgic phase of neuralgia of the sublingual and submandibular ganglia: characterized by the paroxysmal pain described above, may be accompanied by swelling, increased sensitivity of the tongue and mucous membranes of the oral cavity. The pain may migrate to various areas of the head and upper torso.
- The ganglioneuritic phase of ganglion neuralgia is already a transition to a chronic form. At this stage of the development of the disease, dull pain in the affected side is constantly present, disturbances in salivation, trophic ulcers appear, possible decrease in sensitivity and signs of autonomic neurological Bernard-Horner syndrome.
In some cases, during a severe painful attack, patients experience such manifestations of the disease as chills, increased heart rate, increased blood pressure, gastrointestinal spasms, nausea, vomiting, feelings of anxiety and fear.
The chronic form of the disease is the most dangerous, fraught with peripheral circulatory disorders, spasms and autonomic changes in nerve endings in the submandibular and sublingual area, as well as in nearby areas.
Diagnosis of neuralgia of the submandibular and sublingual nodes
A neurologist can detect and diagnose diseases of the vegetative nodes during a personal examination of the patient. To establish an accurate diagnosis, topical diagnostics is used, which includes:
- patient interview;
- analysis of complaints;
- examination using palpation and additional techniques;
- as well as identifying objective signs of pathology.
Since there are several vegetative nodes in the head and face area, and the symptoms of their diseases are very similar, the main task of the neurologist during the initial examination will be to identify the location of the disease.
Using sliding and fixing palpation, the specialist identifies the localization of the pathological process. Sometimes pinching or superficial pain stimulation methods are used for accurate diagnosis.
If the doctor has doubts about the results of topical diagnostics, a diagnostic blockade technique is used, which makes it possible to absolutely accurately establish the source and localization of neuralgia.
The blockade is carried out on an outpatient basis by injecting local anesthetics (novocaine, lidocaine, trimecaine) into the painful area.
Pain relief for a while allows the doctor to make an accurate diagnosis.
Symptoms of neuralgia of the submandibular and sublingual nodes often have similar symptoms to inflammation of the gums and internal structure of the teeth. To rule out dental diseases, you may need to consult a specialist in this field.
Treatment of neuralgia of the submandibular and sublingual nodes
Complex therapy of the disease is carried out under the supervision of a specialist. The methods, manipulations and drugs used in treatment depend on the degree and form of the disease, as well as the reasons that provoked its occurrence.
- Etiological therapy is the elimination of foci of infection and other causes that provoked the disease. If necessary, treatment is carried out with the involvement of specialized specialists if the cause of the disease is chronic pathologies of internal organs.
- Pathogenic therapy is drug treatment using methods for therapeutic blockade, drugs to improve blood circulation and tissue metabolism, vitamins and antispasmodics. During the treatment, blockers of the cholinergic system, ganglion blockers, and adrenergic blockers are used.
- Sympathetic therapy is the removal of acute painful symptoms for general and mental recovery. For treatment, sedatives and hypnotics are used, and in rare cases, antidepressants.
An important step in the treatment of neuralgia of the submandibular and sublingual nodes will be physiotherapeutic methods and reflexology - laser therapy, cryotherapy, acupuncture, electrophoresis, galvanization, etc.
Inflammation of the lower and upper jaw
Inflammatory process in the jaw
Inflammation of the jaw is a serious disease that can have serious consequences. When the first symptoms appear, you should immediately consult a doctor and begin treatment. Inflammation of the jaw is the cause of many complications, although it is not so common in dental practice.
The etiology of the disease is different, but often the cause of its appearance is infection. Treatment of the inflammatory process can take quite a long period of time, even with timely diagnosis.
Classification of the disease
The inflammatory process in the jaw can be classified into several types:
- Osteitis. In this case, the spongy substance in the bone tissue becomes inflamed. It does not last long and takes the form of periostitis.
- Periostitis . The inflammatory process is localized in the periosteal tissue of the jaw and is the result of a complication of periodontitis. Speaking about the clinical picture, the following symptoms can be identified:
- The gums around the diseased tooth begin to swell, it becomes hyperemic and swollen;
- strong painful sensations appear;
- it is possible to discharge purulent contents from the swollen gums.
If a purulent cavity occurs, fistulas may form to allow the pus to escape. In advanced situations, an intensification of the pathological process and purulent inflammation of bone tissue is possible.
- Osteomyelitis. In this case, all layers of bone tissue are affected, and most often this is observed in the lower jaw.
The disease with neuritis is especially difficult, i.e. when the trigeminal nerve is also involved in the process. If inflammation of the jaw nerve occurs, the symptoms are expressed in excruciating pain, mainly on one side of the face.
Inflammation of the nerve under the jaw
There are also several forms of jaw inflammation:
- Acute course of the disease. Pain and inflammation are localized in one place. Symptoms of body intoxication appear quite sharply.
- In the subacute form, the patient feels a little better and may think that the disease has subsided, but this is not so. The inflammation still continues, it’s just that a fistula has formed and pus has broken through, so the pain has subsided somewhat.
- In the chronic form there are no special clinical symptoms, but during this period there is a great danger to the patient’s health, since untreated inflammatory foci can cause more serious complications.
It is very important to notice the disease in time and consult a doctor for help.
Causes of pathology
Maxillofacial inflammation can occur for many reasons. They can be divided into several groups, which will be presented in the table below.
| Pathway of inflammation transmission | Characteristic | Causes |
| Odontogenic | Transmission occurs through infection through diseased teeth. This develops as follows: pathogenic microorganisms approach the root canal through the pulp, periodontitis appears. The inflammatory process then spreads to the periosteal tissue, and then affects all layers of the bone. In this case, there is also a great danger of infection (usually anaerobic bacteria, streptococci, staphylococci) entering the lymph nodes with subsequent infection | The following diseases can provoke such a disorder:
|
| Hematogenous | Infection of the jawbone occurs primarily through the blood. If there is a pathological focus in any organ or system, the infection through the circulatory system can reach the bone tissue of the jaw and cause its inflammation. First, the bone itself may be affected, and then the teeth. Most often, this route of transmission occurs against a background of weakened immunity. | This includes:
|
| Traumatic | Appears as a result of physical damage to the jaw bone | Mechanical damage can occur as a result of the following reasons:
|
Causes of jaw inflammation
There are also several predisposing factors that can trigger the development of an inflammatory process in the jaw:
- poor nutrition, stress and overwork, leading to a weakening of the body’s defenses;
- hypothermia;
- the presence of carious teeth (the more there are, the higher the risk of developing the disease);
- the presence of acute or relapse of chronic inflammatory foci, etc.
What symptoms accompany the inflammatory process?
The clinical picture depends on how severe the inflammatory process is and how the severity of its course is assessed.
Speaking about the general group of symptoms, we can highlight the following signs:
- symptoms of intoxication of the body appear (body temperature rises, the patient feels weak, apathetic, his sleep is disturbed and his appetite disappears);
- around the inflamed area there is hyperemia of the skin, as well as swelling and pain when pressed;
- with strong compression of the upper and lower jaw, you can hear a crunch;
- due to possible displacement of the jaw bones, distortion of facial shape occurs;
- severe pain occurs when eating or talking;
- after sleep, it is difficult for the patient to open his mouth;
- Dizziness, headaches, and decreased sound acuity may occur;
- pain occurs with irradiation to the back of the head, ear, temple.
Attention: the chronic course of the disease occurs with less severe symptoms. The pain is characterized by less severe and sharp pain that occurs during sleep or in the morning.
Pain increases when eating or talking.
If the inflammatory process occurs in a purulent form, a dense formation is formed, in the place of which the skin becomes stretched with a bright red tint.
If inflammation of the maxillofacial nerve occurs, the clinical picture may be supplemented by the following symptoms:
- cyclical acute excruciating pain that occurs in attacks, especially when chewing food, talking, while washing, etc.
- the face may turn red at the time of pain, drooling or lacrimation may occur;
- There may also be pain in the tooth if the second or third branch of the innervation of the trigeminal nerve is affected.
Any warning symptoms should not be ignored by a specialist. Only a doctor can adequately assess the extent of the lesion, its cause and prescribe treatment.
A few facts worth noting
To understand the disease in more detail, we offer you several important points:
- The pathology most often occurs in an acute form.
- In the case of dental origin of the inflammatory process, the affected gum will turn red, become swollen and painful. When purulent masses penetrate into the gum area, it may recede and loosen the tooth.
- If the inflammation is localized in the premolars and molars, the lip, wings of the nose and the bottom may swell.
- With a palatal purulent lesion, swelling of the lymph nodes in the submandibular region will be noticeable. Such inflammation is often provoked by carious processes in the roots of molars and premolars, and incisors. It can spread to the area of the pharynx, tongue and the entire oral mucosa, and with an increase in the volume of purulent exudate, any meal or attempt to speak can be very painful. When the tissue thins and the thin film breaks through, purulent masses enter the oral cavity, and then can reach the gastrointestinal tract, and this is fraught with other serious complications.
- Odontogenic inflammation of the maxillary sinus can affect the area of the eyes and eyelids, and swelling can spread to the cheekbones, temples and cheeks. Swelling of the eyelids leads to narrowing of the palpebral fissures.
- The inflammatory process in the parotid region often provokes damage to the salivary glands.
Attention: The abundance of purulent exudate is a fundamental factor in the appearance of intoxication of the body, as well as in the occurrence of phlegmon, and then an abscess. These conditions threaten not only the patient’s health, but also his life.
Diagnostic and treatment methods
In its acute form, it is much easier to recognize the disease than in its chronic form, since the symptoms are pronounced and not as erased as in the latter case.
When visiting a doctor, the patient may be offered the following diagnostic methods:
- laboratory research;
- magnetic resonance imaging (MRI);
- external examination of the patient, palpation and history taking;
- conducting ultrasound diagnostics;
- computed tomography (CT);
- X-ray examination;
- examination by highly specialized doctors (ophthalmologist, otolaryngologist, etc.).
Instructions for treating an inflammatory process in the jaw always involve an integrated approach. In the presence of an infectious agent, the use of antibacterial drugs is always required, and in the presence of purulent exudate, consultation with a facial surgeon is necessary.
If an opening is necessary, inflammation under the jaw or in any other area is eliminated by creating space for the drainage of pus, and then cleaning the area and administering antibiotics to prevent relapse.
At the time of therapy, the jaw is provided with complete rest. This point can be achieved by applying a sling-shaped bandage for 2-3 days or a special plate between the teeth.
The diet must be high in calories, and the food must be of a liquid consistency at the optimal temperature. In case of severe pain, painkillers are prescribed, the price of which can be either low or quite high.
Also in the treatment of pathology it is possible to use the following methods:
- physiotherapeutic procedures;
- compresses with bee venom;
- electrophoresis with medications containing iodine;
- paraffin therapy;
- use of traditional methods.
Maxillofacial inflammation requires an immediate visit to the doctor. The use of decoctions alone or self-medication can provoke serious complications, and even in the case of a later recovery, the disease will become chronic and thus ensure fairly frequent relapses for many years to come.
Do not forget that next to the jaw there are eyes, canals and maxillary sinuses, which communicate with the meninges. Damage to sensitive cells in this area is fatal, so you should take your health more seriously.
Source: https://Denta.help/hirurgicheskaya/vospalitelnye/vospalenie-chelyusti-396
Symptoms
Symptoms of inflammation of the trigeminal nerve can be divided into conditional primary and secondary symptoms.
Pain syndrome
The first and main symptom of inflammation of the trigeminal nerve is pain. It can torment the patient for several days, weeks or months. After some time, even without appropriate treatment, pain may disappear, but this in no way indicates that the disease has receded.
Painful sensations when the trigeminal nerve is damaged appear in the form of acute, piercing, short-term spasms. Such spasms are almost impossible to calm by taking painkillers. They can occur during palpation of the face, chewing, facial expressions, or simply out of the blue.
Pain with trigeminal neuralgia is conventionally divided into two types:
- Typical.
- Atypical.
Symptoms of inflammation of the upper and lower jaw nerves and their treatment tactics
In the facial part, the largest is the trigeminal nerve. It received its name due to the presence of 3 branches emerging from its node in the temple area: orbital (above), maxillary (middle) and mandibular (bottom). They provide tissue sensitivity and muscle movement on the head. For various reasons, inflammation can affect the entire trigeminal nerve or 1-2 of its branches.
Introduction
Conservative treatment involves the use of drugs of different types of action on the fibers of the facial part of the head. Inflammation is relieved with hormonal, anticonvulsant, antibacterial (if it is caused by pathogenic microflora) and anti-inflammatory drugs.
Disease of the jaw nerve often manifests itself as a result of injury or hypothermia, especially in the facial area of the head. Disorders of the functioning of the trigeminal nerve often arise due to damage to the fibers by the herpes virus.
Neuralgia symptoms can last more than 24 months. To overcome intoxication due to an inflammatory process affecting the trigeminal or other facial nerve, it is necessary to adhere to a diet throughout the entire recovery period. In some cases, fasting is included in treatment to detoxify the body.
Symptoms of inflammation
If the functioning of at least one branch of the trigeminal nerve is disrupted, the superficial and/or deep sensitivity of the corresponding facial region is completely or partially lost.
The pathology manifests itself in the same way: muscles contract incompletely or unevenly or there is tonic tension (prolonged spasm), discomfort, decreased (anesthesia) or increased (hyperesthesia) tactile sensitivity.
Symptoms of inflammation of the maxillary nerve are associated with the disappearance of skin sensitivity in the following areas:
- lower eyelid;
- upper cheek area;
- maxillary sinus;
- at the outer corner of the eye;
- lateral area of the face;
- mucous membrane in the area of the wings of the nose;
- the upper jaw and the teeth and lips located on it.
Additional symptoms: sharp or aching pain, involuntary twitching of the lower eyelid (tic) appears in the area of the affected branch II. If pain is added in the eye area and the entire area above it (under the eyebrow, on the forehead), it means that the inflammation has affected the orbital nerve.
Symptoms of damage to the III (mandibular) branch:
- loss of sensation;
- paresis or paralysis of the masticatory muscle;
- asymmetry of the muscular contour.
The susceptibility of soft and hard tissue in the area of the lower jaw and the mucous membranes adjacent to it in the oral cavity increases or decreases.
Inflammation of the nerve causes symptoms such as pain on palpation or loss of tactile sensations in the area of the outer and inner side of the lower lip, as well as the cheek.
The lesion may affect the gums, teeth, mandibular bone (from the chin to the corner under the earlobe), tongue and sublingual area.
Symptoms of paresis or paralysis due to nerve inflammation:
- reduced strength of chewing muscles (weak bite);
- the mouth is slightly open, while the jaw is shifted towards the source of the disease;
- the mandibular reflex is impaired (the speed of pulling the jaw upward).
However, when one of the branches is inflamed, symptoms often appear in the adjacent area of the face. If, for example, the middle nerve is affected, stronger pain and other sensations may appear in the area of the I and III branches. When the inflammation affects the gasser node itself or its root, the pathology spreads completely to one side, rarely to both parts of the face.
Symptoms of neuritis are expressed as a tic with increased attacks of sharp pain. It can be acute, paroxysmal, limited to one area or covering half of the face on the affected side. Additionally, the vasomotor reaction of the vascular system and secretory function are disrupted, since the central nervous system is always connected to all tissues and glands of the body. In this case, it is the thyroid gland.
Diagnosis and treatment of inflammation of the jaw nerves
If the patient complains of various discomforts in the area of the facial nerve, the doctor checks the sensitivity of this area and the correct movement of the muscles. To begin adequate treatment, the doctor first collects anamnesis, examines the person, and, if necessary, prescribes tomography: MRI, CT.
Research methods:
- touching the surface of the skin with a cotton swab (tactile reaction);
- tingling with a needle in the Zelder area (pain sensitivity);
- palpation of the path of the branches;
- please clench and unclench your jaws, open and close your mouth (motor ability).
When diagnosing, it is important to determine the degree of functioning of all branches of the trigeminal nerve. The doctor also examines the strength of the jaw and conjunctival reflex.
Therapy using official medicine methods
The trigeminal nerve, regardless of which branch is affected by inflammation, is treated comprehensively. To eliminate the causes, the doctor, taking into account the complexity of the process, may choose a method of drug therapy or surgical intervention. Treatment involves dietary nutrition, physiotherapy, and the use of herbal remedies (herbs).
Pain is relieved with medications such as Carbamazepine, Gabapentin, Oxcarbazepine, Clonazepam, Baralgin, Nimesil, Trimecain, Ibuprofen and other drugs with a similar effect on the facial and trigeminal nerve.
Treatment rarely includes narcotics for pain relief if classical analgesics are ineffective.
Suitable sedatives include Sodium hydroxybutyrate and Amitriptyline. Additionally, Rosolacrit, vitamin preparations with a predominance of vitamins B6, B12, and immune-stimulating agents (Echinacea purpurea and others) are prescribed.
Drug treatment of inflammation that has developed for other reasons:
- for herpes infection - Gerpevir, Laferon;
- due to atherosclerosis - Atoris, Rosuvastatin.
When a patient's inflammation is caused by multiple sclerosis, medications are prescribed that should restore the nerve, more precisely, its myelin sheath. Treatment of vessel aneurysm is carried out only by surgical methods.
Treatment using traditional medicine methods
At home, therapy is carried out with regular consultations with a neurologist. Inflammation of the nerves is treated with herbs together with medications, physiotherapy, and other methods. Heat compresses are allowed to be used only if there is no purulent focus in the facial area.
When treating inflammation of the nerves, the following drugs can be used:
- bay oil (to lubricate);
- beet juice (gauze pads in the ear);
- marshmallow root, fresh wormwood (compresses);
- hibiscus, chamomile (tea);
- aloe juice (inside).
Externally, folk remedies are applied to areas of nerve damage, to the submandibular lymph nodes, maxillary sinuses, and into the ear canal. Before starting treatment, be sure to familiarize yourself with the contraindications of the herbal medicine.