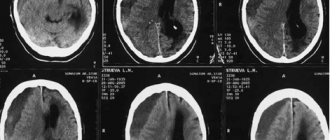
Schematic representation of a brain hematoma located above the hard shell of the latter (epidural). Intracranial hemorrhage is a serious pathology that requires prompt assistance from specialized specialists. The danger of a hematoma is that it disrupts the blood supply to the brain and damages nerve tissue due to local pressure. Pathology in cases of late seeking medical help or inadequate treatment leads to displacement of organ structures due to increased intracranial pressure, which is a serious threat to human life. The insidiousness of the disease is that sometimes symptoms may not appear immediately, and precious time will be lost. If the dynamics of hemorrhage development is negative, the patient has a high chance of dying, despite competent treatment carried out in full. A brain hematoma causes severe pain. As intracranial pressure increases, nausea, vomiting, impaired consciousness, convulsions occur, focal neurological symptoms appear (the size of the pupils changes, paresis develops, sensory disturbances develop, reflexes increase, pathological signs manifest, etc.). The negative dynamics of the course of intracranial hematomas is characterized by a coma, disturbances in the functioning of the cardiovascular system and respiratory arrest. Often, accurate diagnosis of the localization of the pathological process is difficult due to the rapid change in blood volume at the site of injury after a head injury. The main method used by doctors to quickly and informatively assess the state of the brain is computed tomography. There are several classifications of hemorrhages depending on the location, source and timing of the process. Thanks to CT, it is possible to determine the nature of the brain hematoma, the degree of duration of the pathology and the involvement of surrounding tissues. MRI allows you to see very severe damage to the axons of nerve cells or evaluate recovery processes in the long-term period of a traumatic disease. The use of MRI makes it possible to differentiate ischemic and hemorrhagic strokes, when it is not entirely clear whether there is a hematoma in the cranial cavity.
What is an intracerebral hematoma
An intracerebral hematoma is a limited spherical accumulation of liquid blood in the brain tissue, as well as its clots, resulting from the rupture of a blood vessel with the subsequent formation of a hematoma in the brain tissue. In cases of trauma, the hematoma may also have inclusions of cerebral detritus (elements of brain matter and bone tissue that have entered the wound of foreign bodies).
Typically, the growth of an intracerebral hematoma is observed during the first two to three hours that have passed since the onset of hemorrhage (the time may increase if there are blood clotting disorders). Typically, hematomas of this type are often localized in the frontal and temporal lobes of the brain, much less often in the parietal lobes. At the same time, intracerebral hematomas of traumatic origin are often fixed closer to the surface of the brain, and those associated with pathology of vascular origin are in its depth.
What does an MRI show during and after a stroke?
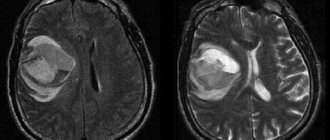
Magnetic resonance imaging for stroke allows you to find out which part of the brain was affected by acute cerebrovascular accident, what is its extent, location and volume. Together with other prognostic signs, these data are important for subsequent prognosis and assessment of the patient’s condition, choice of treatment tactics and assessment of the results of therapy.
MRI is also excellent for follow-up of treatment results. The study can be repeated as many times as necessary for the doctor, without harm to the patient’s health. By observing changes in the images, you can evaluate the effectiveness of the treatment and, if necessary, make its correction. Everything that an MRI shows in a stroke can help doctors, including in preparing for surgical treatment.
Reasons for the formation of intracerebral hematoma
The main reasons causing hemorrhage into the brain tissue and the formation of intracranial hematoma can be considered:
- traumatic brain injuries
- sharp increase in intravascular pressure
- rupture of cerebral aneurysm
- the presence of brain tumors that provoke arrosive bleeding
- pathology of vascular development (arteriovenous malformation)
- impaired elasticity of vascular walls (caused by atherosclerosis, diabetes, systemic vasculitis)
- the presence of diseases of the circulatory system associated with changes in blood viscosity and fluidity
- taking anticoagulants
Mechanism of occurrence
The described disease can manifest itself due to the following factors:
Rupture of vascular walls due to injury (for example, head injury, concussion, etc.).- Post-traumatic diapedesis at the point of contusion.
- Deformation of an aneurysm or arterial-venous malformation due to tumor formation (stroke, hypertension, atherosclerosis, etc.).
- Changes in the rheological functions of blood vessels during hemophilia, leukemia, painful conditions of the liver and others.
What are the symptoms of intracerebral hematoma formation?
Typically, the first symptoms begin to appear from the onset of hemorrhage, although their intensity directly depends on the severity of the lesion. Sometimes, from the moment the hematoma forms until characteristic symptoms are observed, a time may pass (from several hours to months), called the “light interval.” It is customary to distinguish symptoms:
1. cerebral – manifests itself:
- headache of sufficient intensity
- dizzy
- nausea, vomiting
- general weakness and drowsiness
- confused consciousness (sometimes preceded by psychomotor agitation), with a possible transition to coma (as with hemorrhage in the ventricles of the brain)
2. focal – correlated with the volume and localization of the hematoma, manifests itself:
- speech disorders
- difficulty swallowing
- hearing disorders (hard of hearing) and vision (nystagmus, drooping upper eyelid)
- behavior disorder
- loss of sensation in the limbs
- epilepsy attacks
- memory loss
- increased temperature (when blood enters the ventricles of the brain)
Useful facts
An intracerebral bruise may have a liquid texture or consist of coagulated blood. In certain situations, in addition, detritus may be present in the bruise in much smaller quantities. The total volume of liquid can reach 100 ml. The increase in the diameter of the hematoma continues for several hours after the onset of hemorrhage, and during a failure of the coagulation function much longer. After the formation of the lesion, the process of compression of adjacent tissues begins, which subsequently leads to necrosis.
In addition, the occurrence of such a phenomenon affects the increase in the level of intracranial pressure and becomes a source of swelling. It can cause displacement of certain structures and the formation of dislocation syndrome if the bruise is large. Bleeding can lead to a reflex spasm and the onset of ischemia, first affecting the nearby cavities. Ischemia is considered an additional damaging cause, which shapes the progression of abnormal deformations far beyond the boundaries of the formation. According to average statistical information, in almost 14% of cases there is a breakthrough into the ventricles and hemorrhage.
Why is the formation of an intracerebral hematoma dangerous?
The formation of this pathology (even a small one) leads to compression of the surrounding brain tissue, which (depending on the size and location of the hematoma) can result in subsequent serious damage, even necrosis. In addition, an increase in intracranial pressure serves as a provoking factor for the development of cerebral edema. Due to displacement of brain structures, a large intracerebral hematoma often causes dislocation syndrome (a set of symptoms associated with this condition) in patients. It is also possible for a hematoma to break through into the ventricles of the brain. Since cerebral hemorrhage causes a reflex response spasm of cerebral vessels, this leads to the development of cerebral ischemia (starting from the areas closest to the hematoma). Further, pathological processes can spread to other systems of the body, affecting, first of all, the most problematic areas of the patient.
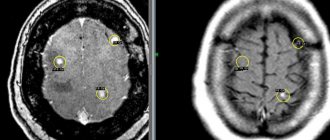
What does blood look like on MRI?
In medical practice, the following types of intracranial hemorrhages occur:
- intraparenchymal hematoma - the formation is caused by rupture of blood vessels due to hemorrhagic stroke (most often due to high blood pressure), traumatic destruction of the artery, inflammatory destruction of the vascular wall, etc. In the images, the hemorrhage is locally located among the white matter of the brain, without connection with damage to the bone structures of the skull, even if the pathology occurred after a head blow;
Intracerebral hematoma due to hemorrhagic stroke (indicated by arrows)
- subarachnoid hemorrhage (SAH) - occurs as a result of a violation of the integrity of a vessel located on the surface of the brain in the subarachnoid space (for example, when a saccular aneurysm ruptures). The main pathological symptoms are considered to be a sudden severe headache, nausea with vomiting and photophobia, depression of consciousness up to coma. This type of hemorrhage provokes vasospasm. In the images, the SAH is located on the surface of the brain;
- subdural hematoma is localized under the dura mater. It differs in the shape of the sickle when visualized on magnetic resonance or computed tomography. Occurs as a result of rupture of veins after injuries, taking anticoagulants, ventricular bypass, and is characterized by a high percentage of deaths. Causes severe displacement of the brain due to intracranial pressure;
- epidural hematoma - usually determined after traumatic injuries. It is localized under the fracture area, between the bones of the skull and the dura mater of the brain. Visually it looks like a biconvex lens;
- intraventricular hemorrhage - primary (formed by a tumor, aneurysm, angioma, etc.) and secondary (as a consequence of the breakthrough of blood from the area of hematoma formation into the ventricular cavity with a large volume of the first);
Treatment of intracerebral hematoma
The optimal treatment for this pathology, based on the individual condition of the patient, is chosen by the neurosurgeon. It can be conservative or surgical, depending on the severity and observed clinical manifestations.
Conservative therapy. It is usually used when the size of the intracerebral hematoma does not exceed 3 cm, and the pathology itself does not compress the medulla oblongata, and under the obligatory condition of the absence of dislocation syndrome. The therapeutic actions of the conservative method consist of the administration of hemostatic agents and drugs that reduce vascular permeability, as well as diuretics that reduce intracranial pressure (while simultaneously monitoring the electrolyte composition of the patient’s blood). Preventive measures are also taken to prevent the development of thromboembolism and correct arterial blood pressure.
Surgical intervention. Indicated for:
- large hematoma
- severe focal symptoms (especially in the presence of dislocation syndrome)
- compression of the brain stem
- disturbance of consciousness
Surgical treatment consists of transcranial removal of the hematoma (by opening the skull), or endoscopic evacuation is performed, which is less traumatic for the patient. Next, antibiotic therapy and restorative treatment are indicated.
Rehabilitation period
In order to prevent seizures and other consequences after surgery to remove a brain hematoma, drug therapy is carried out. Rehabilitation is aimed at restoring brain functions and normal functioning of the body. Includes physical therapy, psychotherapy, therapeutic exercises (the use of robotic simulators to restore motor activity, train fine motor skills and limb movements), massage and other activities.
The appearance of foci of hemorrhage in brain tissue is associated with damage to the integrity of elements of the vascular system, most often as a result of trauma in the head area or as a result of cerebrovascular diseases. The degree of threat to the life and health of the patient depends on the volume and size of the hematoma, the speed of medical care and surgical treatment.
174
Is there a way to prevent intracerebral hematoma?
Typically, preventive measures to prevent intracerebral hematoma are reduced to the maximum exclusion of the factors that provoke it (especially with a potential predisposition to hemorrhagic stroke). Therefore, the doctor may recommend to the patient:
- control of blood and intracranial pressure
- giving up bad habits (in particular, smoking and alcohol abuse)
- relaxation practice (to successfully overcome stress)
- moderate exercise and walking
It is important to remember that intracerebral hematoma is a very insidious pathology due to its consequences. That is why it is so important for the patient to visit a modern clinic in a timely manner for proper diagnosis and treatment.
Experienced medical specialists are always ready to come to your aid at the slightest suspicion of this disease! Don't waste your precious time and be healthy!
Diagnostic options
With the help of new-fangled clinical devices, doctors have a large number of opportunities to conduct research on patients with the presenting disease. Thanks to such devices, doctors can study not only the formation itself, but also understand what causes the development. The main technology used by specialists in the capital’s medical institutions is computed tomography. Often, on the images obtained, experts see the pathology in the form of a round or oval lesion. If deviations from the norm occurred due to damage, then, as a rule, uneven boundaries are visible in photographs.
In case of diameter reduction, magnetic resonance scanning is used. In some situations, this examination may give erroneous readings, which is why doctors prefer to use two tests simultaneously. At certain points, angiographic examination or MR angiography is performed to determine vascular disorders and the formation of aneurysms.