Causes of conditions associated with expansion of the subarachnoid space
All causes can be either congenital or acquired. In the first version, the pathology concerns infants. As for the second option, people of different age categories are susceptible to this. The following situations can lead to such conditions:
- Processes associated with inflammation of the meninges. We are talking about meningitis, meningoencephalitis, arachnoiditis. Moreover, all of them can be caused by both infectious and non-infectious causes.
- Traumatic injury to the skull and brain.
- Defects in the development of the central nervous system.
- Processes associated with hemorrhage localized under the meninges.
- Brain swelling.
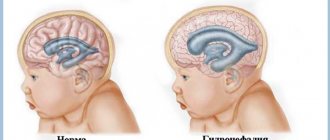
Inflammations associated with both the membranes and the brain itself lead to the formation of adhesions in the cranial cavity. Naturally, this disrupts the circulation of cerebrospinal fluid, complicates its outflow and leads to the formation of hydrocephalus. This, in turn, causes the expansion of not only the ventricles of the brain, but also the subarachnoid space.
When inflammation occurs, all pathomorphological and pathophysiological changes associated with it come to the fore. The permeability of the vascular walls increases significantly. The liquid part of the blood freely penetrates into the space between the cells, which forms swelling. In addition, the production of liquor itself increases significantly. Pathomorphologically, in this phase one can observe thickening and congestion of the meninges and expansion of the space under the meninges.
The manifestation of pathology in children varies and is determined by the severity of the process. You can suspect the presence of such a condition based on the following signs:
- In response to light and noise stimuli of medium intensity, the child responds with an extremely negative reaction.
- Such children experience frequent regurgitation.
- The child is excessively restless and has sleep disturbances.
- The pupils of the left and right eyes are different in size, and strabismus may occur.
- The size of the head clearly does not correspond to his age.
- The fontanel overgrows very slowly.
- The child often shudders, and tremor of individual parts of the body can be observed objectively.
As you can see, all these symptoms do not have any specificity and it is impossible to establish an accurate diagnosis using them alone. It is necessary to contact a pediatrician who will refer the child for a consultation with a pediatric neurologist.
As for adults, the dominant symptom will be headache. It can have varying degrees of intensity. It also differs in its duration. Dizziness, nausea, and inability to fully perform your professional duties with high quality may occur. The headache is especially severe in the morning.
At the peak of pain, the patient feels a pronounced pulsation. Sometimes vomiting occurs. Patients are restless and anxious. As intracranial pressure increases, headaches become more intense. Sleep is disturbed. Even if the patient manages to fall asleep, his sleep is intermittent and with obvious signs of anxiety. During the day, patients, on the contrary, show severe drowsiness.
This condition cannot continue indefinitely, and a moment comes when the symptoms characteristic of encephalopathy become clear. This is due to dystrophic changes in the cerebral cortex. Memory becomes worse, visual disturbances are observed, and the level of intelligence decreases. Patients constantly feel severe fatigue. Characterized by endless repetition of headache attacks.
If the perivascular spaces of the basal ganglia are expanded, changes in gait may be observed, coordination of movements may be significantly impaired, and fine motor skills may be impaired. As a result, ability to work and activity in lifestyle are impaired.
Causes of spots on MRI of the brain
When receiving images after an MRI of the brain, the patient examines them, despite the fact that he does not have the special knowledge to decipher the examination results. But even he becomes clear that there are some pathologies if he sees dots or spots of white color that stand out sharply against the general background. Let's find out what could be the causes of white spots on MRI images of the brain.
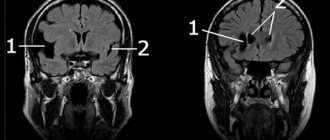
Perivascular spaces of Virchow-Robin
Perivascular spaces are fluid that accumulates along the blood vessels supplying the brain. Another name for them is criblures. Every person has them, but usually they are small and are not visualized on photographs of the organ being examined.
When cerebral circulation is impaired, the criblures expand. Because they are filled with cerebrospinal fluid. They contain a large number of hydrogen atoms. And in this area the response signal will be of high intensity, which can be seen in the photographs as a white spot.
Enlarged perivascular spaces are detected in many patients. Most often they are harmless. A neurologist can accurately determine whether criblures are dangerous in particular cases.
Demyelinating pathologies
Demyelination is a pathological process that affects the myelin sheath of nerve fibers. The nature of the damage depends on its cause. She may be:
- Congenital (hereditary predisposition to the disease).
- Acquired (demyelination develops as a result of inflammatory processes in the brain).
Here are the diseases that show demyelinating lesions in the brain on MRI:
- Myelinopathy;
- Leukoencephalopathy;
- Multiple sclerosis.
Typically, demyelinating lesions appear as multiple white spots. The patient may perceive them as criblures because they are similar. Only a specialist can distinguish them from each other based on the severity and localization of the increased signal.
Gliosis in the medulla
Gliosis of the brain is the process of replacing neurons with glial cells. This is not an independent disease, but a consequence of other diseases.
Pathology in the form of foci of gliosis on MRI is usually detected in the following diseases:
Glial cells perform the work that dead neurons were supposed to do. It is thanks to them that the functions of the nervous system are restored after injuries.
Single small lesions can only be detected on MRI. There are usually no other symptoms.
If the underlying disease continues to kill neurons, a clinical picture emerges, and MRI images already show multiple pathological foci of the brain.
MRI helps detect the presence of gliosis, but in most cases does not tell what caused the changes. The differential diagnosis of dyscirculatory encephalopathy and multiple sclerosis is especially difficult. To decipher the results, you will need the help of at least two specialists with extensive experience: a neurologist and a neuroradiologist.
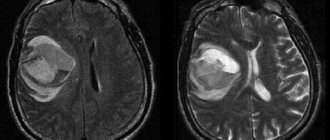
Brain swelling
White spots on an MRI may indicate swelling of the brain tissue. They develop against the background:
- tumors;
- injuries;
- ischemia;
- inflammation;
- hemorrhages.
At the initial stage of the disease, MRI reveals signs of perifocal edema in the form of light spots in the area of the affected area of the organ.
If normal blood circulation is not restored, generalized edema develops. The brain swells.
On an MRI, this is visible in a blurry picture in which the structures of the organ are not visible, since they all provide a high-intensity signal to the tomograph.
Sites of Alzheimer's disease
MRI can be used to diagnose and monitor the progress of Alzheimer's disease. Focal formations in this disease are not white, but almost black. This is due to atrophic processes occurring in the organ, which begins to decrease in size.
The affected areas do not respond well to the radio signal sent to them, so they are called low signal intensity areas. Dystrophy of the posterior parts of the brain is especially well visualized.
Magnetic resonance imaging reveals structural abnormalities in the brain.
Therefore, this research method is useful in diagnosing diseases that cause changes in the structure of the organ and the blood vessels that penetrate it.
Anyone can distinguish an image of a healthy brain from an image with pathological foci. But only a doctor can make a diagnosis after a long study of the MRI results.
Source: //diagme.ru/mrt/golova-i-sheya/ochagi
Compound
Perivascular spaces are gaps containing interstitial fluid that span between blood vessels and their host organ, such as the brain, that they penetrate and serve as extravascular channels through which solutes can pass. Like the blood vessels around which they form, perivascular spaces occur in both the brain's subarachnoid space and subpial space.
The perivascular spaces surrounding arteries in the cerebral cortex and basal ganglia are separated from the subpial space by one or two layers of the leptomeninges, respectively, as well as the pia mater. By virtue of the leptomeningeal cell layer, the perivascular spaces belonging to the subarachnoid space are continuous with those of the subpial space.
The direct connection between the perivascular spaces of the subarachnoid space and subpial space is unique to the cerebral arteries, since no leptomeningeal layers surround the cerebral veins. Using a scanning electron microscope, it was determined that the spaces surrounding the blood vessels in the subarachnoid space are not continuous with the subarachnoid space due to the presence of mater PIA cells connected by desmosomes.
Perivascular spaces, especially around fenestrated capillaries, are found in many organs, such as the thymus, liver, kidney, spleen, bone, and pineal gland. Particularly within the brain circumventricular organs—subfornical organs, area postrema, and median eminence—large perivascular spaces are present around fenestrated capillaries, indicating that the spaces serve a dispersive role as brain- or blood-transmitting messengers.
Perivascular spaces can be enlarged to a diameter of five millimeters in healthy individuals and do not imply disease. When increased, they can impair the function of the areas of the brain to which they project. The stretch may occur on one or both sides of the brain.
Perivascular spaces differ on MRI in several key features. The spaces appear in contrast to round or oval objects with a signal intensity visually equivalent to that of the cerebrospinal fluid in the subarachnoid space. Additionally, the perivascular space has no mass effect and is located along the blood vessel around which it forms.
Disseminated encephalomyelitis
Disseminated encephalomyelitis (DEM) is an acute pathology of the central nervous system. In this disease, the myelin sheath of nerve fibers is destroyed. The perivascular Virchow-Robin spaces are dilated due to damage to the white and gray matter. The MRI image shows foci of demyelination.
This pathology is of autoimmune origin. The clinical picture of the disease resembles signs of multiple sclerosis. Patients experience gait and movement disturbances, speech disorders, dizziness, and inflammation of the optic nerve.
Unlike many other demyelinating diseases, REM is treatable. Patients are prescribed corticosteroids to suppress the autoimmune reaction:
- "Prednisolone";
- "Dexamethasone";
- "Metypred."
After a course of therapy, 70% of patients experience complete recovery. In advanced cases, patients may still experience the consequences of the disease: impaired sensitivity of the limbs, gait disturbances, and visual disturbances.
function
One of the most basic roles of the perivascular space is to regulate the movement of fluid in the central nervous system and its drainage. The gaps eventually drain fluid from the neuronal cell bodies into the cervical lymph nodes. Specifically, the "Tide Hypothesis" proposes that cardiac contraction creates and maintains pressure waves to modulate flow to and from the subarachnoid space and perivascular spaces. Acting as a sort of sponge, they are essential for signal transmission and extracellular fluid maintenance.
Another function is as an integral part of the blood-brain barrier (B). While Bs are often described as tight junctions between endothelial cells, this is a simplification that neglects the complex role that perivascular spaces take in separating venous blood from the brain parenchyma.
Often, cell debris and foreign particles that are impermeable to B will get through the endothelial cells, only to be phagocytized into the perivascular spaces. This is true for many T and B cells as well as monocytes, giving this small fluid-filled space an important immunological role.
Perivascular spaces also play an important role in immunoregulation; They contain not only interstitial and cerebrospinal fluid, but they also have a constant flow of macrophages, which is regulated by mononuclear cells through the blood, but do not pass through the basement membrane of the glial membrane limiting.
Likewise, as part of its role in signal transduction, the perivascular spaces contain vasoactive neuropeptides (VNS), which, in addition to regulating blood pressure and heart rate, have an important role in the control of microglia. ANS serves to prevent inflammation by activating the enzyme adenylate cyclase, which then produces cAMP.
The production of cAMP mediates the modulation of autoreactive T cells by regulatory T cells. The perivascular space is a susceptible space for VN compromise and, when their function is reduced to a space, the immune response is negatively affected and the potential for increased degradation. When T cell inflammation begins, astrocytes begin to undergo apoptosis, due to their CD95 receptor to open the glial limiting membrane and let T cells into the brain parenchyma.
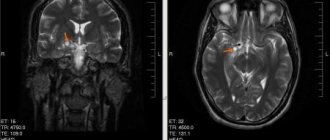
Ischemic conditions
With ischemia, the blood supply to the brain deteriorates. This is usually a consequence of atherosclerotic changes in the vessels. The patient periodically experiences dizziness, double vision, motor coordination disorders, speech and memory disorders. Due to changes in the vessels, the spaces around their walls also expand.
Patients are prescribed nootropic drugs (Piracetam, Cerebrolysin, Actovegin), as well as drugs that normalize metabolism in brain cells (Cortexin, Ceraxon). In this case, it is very important to carry out etiotropic treatment of atherosclerosis with statins. The drugs Lovastatin, Atorvastatin, and Simvastatin are prescribed. This therapy eliminates the cause of ischemia.
Clinical significance
The clinical significance of perivascular spaces comes primarily from their tendency to expand. The importance of expansion would hypothetically be based on changes in shape rather than size. Enlarged spaces are observed most often in the basal ganglia, in particular on the lenticulostriate arteries.
They have also been observed along the paramedian mesencephalothalamic artery and substantia nigra in the mesencephalon, the region of the brain below the insula, the dentate nuclei in the cerebellum, and the corpus callosum, as well as the region of the brain immediately above it, the cingulate gyrus. In clinical use of MRI, it has been shown in several studies. that perivascular space distension and lacunar streaks are the most commonly observed histological correlates of signaling abnormalities.
Dilatation is most frequently and closely associated with aging. Dilatation of perivascular spaces correlates better with age, even when concomitant factors including hypertension, dementia, and white matter lesions are considered. In older adults, for example, dilatation correlates with many symptoms and conditions that often affect the arterial vascular wall, including hypertension, atherosclerosis, cognitive decline, dementia, and low postmortem brain weight.
In addition to dilatation among older people, dilatation in young people can also be observed in healthy people. This phenomenon is rare and there have been no observed associations in such cases with reduced cognitive function or white matter abnormalities. When extended VRS is observed in the callosum, there is generally no neurological deficit associated. They are often observed in this area as cystic lesions with cerebrospinal fluid type.
Symptoms of dilatation
Extreme dilatation has been associated with a number of specific clinical symptoms. In cases of severe dilatation in only one hemisphere, symptoms reported include nonspecific syncope attacks, hypertension, positional vertigo, headache, early recall impairment, and hemifacial tics.
Symptoms associated with severe bilateral dilatation include ear pain (which has reportedly resolved on its own), dementia, and seizures. These data were collected from case studies of individuals with severe VRS dilatation. Considering the anatomical abnormality presented in such cases, these results were considered surprising in that the symptoms were relatively mild.
In most cases there is really no mass effect associated with some VRS dilatation. The exception is the mildness of clinical symptoms associated with VRSOM dilatation, when there is extreme dilatation in the lower mesencephalon at the junction between the substantia nigra and the cerebral stalk.
In such cases, mild to moderate obstructive hydrocephalus was reported in most patients. Associated symptoms ranged from headaches to symptoms more severe than those only discussed in cases of dilation of the cerebral hemispheres. Other common symptoms associated with HRMS dilatation include headaches, dizziness, memory impairment, poor concentration, dementia, visual changes, oculomotor abnormality, tremors, seizures, limb weakness and ataxia.
Dilatation is a typical characteristic of a number of diseases and disorders. These include diseases from metabolic and genetic disorders such as mannosidosis, myotonic dystrophy, Lowe syndrome, and Coffin-Lowry syndrome. Dilatation is also a common characteristic of diseases or disorders of vascular pathologies, including CADASIL (cerebral autosomal dominant arteriopathy with subcortical infarcts and leukoencephalopathy), hereditary infantile hemiparesis, retinal arteriole tortuosity and leukoencephalopathy, migraine, and vascular dementia.
And disorders of the third group, usually associated with VRSOM dilatation, are neuroectodermal syndromes. This includes polycystic brain disease associated with ectodermal dysplasia, frontonasal dysplasia and Joubert syndrome. There are four different groups of disorders commonly associated with sprains that include autism in children, Megalencephalopathy, Secondary Parkinson's disease, new-onset multiple sclerosis, and chronic alcoholism.
Perivascular spaces are dilated - what is it? Causes and treatment
If brain pathology is suspected, patients are prescribed magnetic resonance imaging. Often the study results indicate that the patient has dilated perivascular spaces. How dangerous is this? And what diseases could such a sign indicate? We will consider these questions in the article.
What it is
Perivascular spaces are located between the walls of blood vessels and the white matter of the brain. These formations are also called criblures or Virchow-Robin spaces. They are filled with cerebrospinal fluid and regulate the outflow of cerebrospinal fluid.
Normally, criblures are so small that they are not visible on an MRI image. However, there are cases when examination reveals expanded perivascular spaces. What does this diagnostic result mean? This suggests that criblures are visualized during an MRI examination. They look like white spots in the photo.
Causes
Enlarged perivascular Robin-Virchow spaces are not always a sign of pathology. This diagnostic result is also observed in completely healthy people. Most often, expansion of criblures is observed in elderly patients and is associated with age-related changes in the brain.
However, in some cases, dilated perivascular spaces may be a sign of the following diseases and conditions:
- brain atrophy;
- leukoaraiosis;
- cerebral ischemia (including cerebral infarction);
- disseminated encephalomyelitis.
In elderly people, expansion of criblures is often observed with hypertension, atherosclerosis, and dementia. These pathologies are usually accompanied by memory impairment and other cognitive impairment.
What to do if the MRI results indicate that you have dilated perivascular Virchow-Robin spaces? It is necessary to show the transcript of the study to a neurologist. Only a specialist can determine whether this is a variant of the norm, an age-related feature, or a sign of pathology.
There are cases when MRI does not reveal any changes in the brain, but the image shows dilated perivascular Virchow-Robin spaces. What does this mean? As a rule, such a sign does not indicate pathology. Doctors consider an increase in criblures only in combination with other changes identified during an MRI examination.
If necessary, the doctor may prescribe additional tests:
- multislice computed tomography;
- vascular angiography;
- Dopplerography;
- cerebrospinal fluid examination.
Let's take a closer look at the most common diseases and conditions that can lead to expansion of criblures.
If the patient’s perivascular spaces are expanded and the volume of the brain is reduced, then doctors talk about organ atrophy. Most often this is a sign of the following diseases:
- senile dementia;
- atherosclerosis;
- Alzheimer's disease.
In these diseases, neurons die. This is accompanied by memory impairment, mental impairment, and mental disorders. Typically, such diseases occur in elderly patients.
In some cases, dilated perivascular Virchow-Robin spaces are detected in newborns. This may be a sign of serious genetic diseases accompanied by the death of neurons.
How to treat such pathologies? After all, it is no longer possible to restore lost neurons. You can only slow down the process of death of nerve cells. Patients are prescribed the following drugs for symptomatic therapy:
- nootropics: “Piracetam”, “Cavinton”, “Nootropil”;
- sedatives: “Phenazepam”, “Phenibut”;
- antidepressants: Valdoxan, Amitriptyline.
The prognosis of such pathologies is usually unfavorable, as brain atrophy and neuronal death progress.
Leukoaraiosis
Doctors call leukoaraiosis a thinning of the white matter of the brain. Due to structural changes in the nervous tissue, patients have enlarged perivascular spaces. This is also a sign of diseases characteristic of older people:
- hypertension;
- atherosclerosis;
- senile dementia.
Changes in the white matter of the brain cause cognitive impairment. Patients are treated symptomatically with nootropic drugs. These drugs improve the nutrition of neurons and stop their death. For atherosclerosis, statins are indicated. For high blood pressure, antihypertensive drugs are prescribed.
Ischemic conditions
With ischemia, the blood supply to the brain deteriorates. This is usually a consequence of atherosclerotic changes in the vessels. The patient periodically experiences dizziness, double vision, motor coordination disorders, speech and memory disorders. Due to changes in the vessels, the spaces around their walls also expand.
Patients are prescribed nootropic drugs (“Piracetam”, “Cerebrolysin”, “Actovegin”), as well as drugs that normalize metabolism in brain cells (“Cortexin”, “Ceraxon”). In this case, it is very important to carry out etiotropic treatment of atherosclerosis with statins. The drugs Lovastatin, Atorvastatin, and Simvastatin are prescribed. This therapy eliminates the cause of ischemia.
Brain infarction
Often the perivascular spaces are dilated in patients who have suffered a cerebral infarction. This disease is a consequence of prolonged ischemia. In some cases, cerebral infarction is asymptomatic and goes unnoticed by the patient. Its consequences can only be seen in an MRI scan.
It is important to remember that if the patient has risk factors (high blood pressure, atherosclerosis, diabetes), then the heart attack may recur in severe form. To prevent a recurrent attack of acute ischemia, patients are prescribed antihypertensive medications, hypoglycemic agents, and blood thinners.
Disseminated encephalomyelitis
Disseminated encephalomyelitis (DEM) is an acute pathology of the central nervous system. In this disease, the myelin sheath of nerve fibers is destroyed. The perivascular Virchow-Robin spaces are dilated due to damage to the white and gray matter. The MRI image shows foci of demyelination.
This pathology is of autoimmune origin. The clinical picture of the disease resembles signs of multiple sclerosis. Patients experience gait and movement disturbances, speech disorders, dizziness, and inflammation of the optic nerve.
Unlike many other demyelinating diseases, REM is treatable. Patients are prescribed corticosteroids to suppress the autoimmune reaction:
- “Prednisolone”;
- “Dexamethasone”;
- “Metypred.”
After a course of therapy, 70% of patients experience complete recovery. In advanced cases, patients may still experience the consequences of the disease: impaired sensitivity of the limbs, gait disturbances, and visual disturbances.
Prevention
How to prevent the above pathologies? It can be concluded that older patients are more susceptible to such diseases. Therefore, all people over 60 years of age need to regularly visit a neurologist and undergo an MRI examination of the brain.
It is also important to constantly monitor blood cholesterol levels and blood pressure. After all, diseases accompanied by pathological changes in the white matter most often develop against the background of atherosclerosis and hypertension.
Source: //FB.ru/article/412408/perivaskulyarnyie-prostranstva-rashshirenyi—what-eto-takoe-prichinyi-i-lechenie
Kidneys as a factor of pathology
Kidney pathology can cause a moderate edematous syndrome, in which there will be a situation associated with the expansion of the spaces under the meninges. Sometimes this may be due to poisoning with heavy metal salts. Chronic alcohol intoxication may also be a cause.
Of course, all these conditions are more typical for adults. In children, the predominant causes are congenital anomalies. The cause may also be birth trauma, which disrupts the circulation of fluid in the cranial cavity.
Prevention
How to prevent the above pathologies? It can be concluded that older patients are more susceptible to such diseases. Therefore, all people over 60 years of age need to regularly visit a neurologist and undergo an MRI examination of the brain.
It is also important to constantly monitor blood cholesterol levels and blood pressure. After all, diseases accompanied by pathological changes in the white matter most often develop against the background of atherosclerosis and hypertension.
Current research
Much of the modern research concerning Virchow-Robin spaces is due to their well-known tendency to expand. Research is currently being carried out in order to determine the exact cause of dilatation in these perivascular spaces. Current theories include mechanical trauma resulting from cerebrospinal fluid pulsation, elongation of ectactic penetrating blood vessels, and abnormal vascular permeability leading to increased fluid exudation.
Further research has implicated shrinkage or atrophy of surrounding brain tissue, perivascular demyelination, coiling of arteries as they age, changes in arterial wall permeability, and obstruction of lymphatic drainage pathways. Additionally, insufficient fluid drainage and damage to ischemic perivascular tissue, resulting in an ex-vacuum effect, have been proposed as possible causes for advanced ARSA.
Recent and ongoing research has found an association between increased VRS and a number of diseases.
Leukoaraiosis
Doctors call leukoaraiosis a thinning of the white matter of the brain. Due to structural changes in the nervous tissue, patients have enlarged perivascular spaces. This is also a sign of diseases characteristic of older people:
- hypertension;
- atherosclerosis;
- senile dementia.
Changes in the white matter of the brain cause cognitive impairment. Patients are treated symptomatically with nootropic drugs. These drugs improve the nutrition of neurons and stop their death. For atherosclerosis, statins are indicated. For high blood pressure, antihypertensive drugs are prescribed.
story
The appearance of perivascular spaces was first noted in 1843 by Durand-Fardel. In 1851, Rudolf Virchow was the first to provide a detailed description of these microscopic spaces between the outer and inner/middle lamina of cerebral vessels. Charles-Philippe Robin confirmed these findings in 1859 and was the first to describe perivascular spaces as canals that existed in normal anatomy.
For many years after Virchow-Robin spaces were first described, it was believed that they were in free communication with the cerebrospinal fluid in the subarachnoid space. It was later shown using electron microscopy that the pia mater serves as a separation between the two.
When using MRI, measuring signal intensity differences between the perivascular spaces and the cerebrospinal fluid supported these findings. The research technologies continue to expand, so that information regarding their function, anatomy and clinical significance has also been made available.
Additional diagnostic methods
What to do if the MRI results indicate that you have dilated perivascular Virchow-Robin spaces? It is necessary to show the transcript of the study to a neurologist. Only a specialist can determine whether this is a variant of the norm, an age-related feature, or a sign of pathology.
There are cases when MRI does not reveal any changes in the brain, but the image shows dilated perivascular Virchow-Robin spaces. What does this mean? As a rule, such a sign does not indicate pathology. Doctors consider an increase in criblures only in combination with other changes identified during an MRI examination.