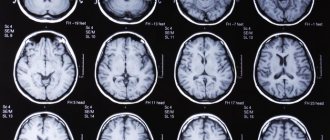
Before moving on to the issue of rehabilitation after neurosurgery and traumatic brain injuries, you need to have a clear understanding of both.
Traumatic brain injury (TBI) is a set of contact injuries (soft tissues of the face and head, skull bones and facial skeleton) and intracranial injuries (damage to the substance of the brain and its membranes), having a single mechanism and age of formation. TBI is the third most common cause of death in the country (after cancer and cardiovascular diseases).
Neurosurgical surgery involves surgical treatment of diseases of the central and peripheral nervous system that arise both as a result of TBI or independently. The consequence of severe TBI and any neurosurgical intervention is a disruption of brain function of varying duration and severity, requiring further rehabilitation under the supervision of a neurologist. The rehabilitation program after TBI is highly individual and depends on the severity of the injury, the period of occurrence and the nature of the complications.
Treatment of brain tumors
Modern oncology has three main methods of treating intracranial tumors:
- surgical intervention;
- radiosurgery and radiation therapy;
- chemotherapy method.
A radical way to get rid of a tumor is brain surgery. Methods such as chemotherapy and radiation therapy are concomitant effects on the site of pathology before or after surgical treatment.
Radiosurgery is a method of radiation therapy that allows you to cope with a tumor without surgery. Advanced equipment such as cyberknife and gamma knife are used to perform radiosurgery.
Indications and contraindications for surgery
When treating a brain tumor, neurosurgery is sometimes not only indicated, but also necessary if:
- as a result of the growth of education, pressure is placed on vital parts of the brain;
- there is a significant risk of the cancer progressing to the stage of metastasis;
- the localization of the tumor allows it to be removed without significant impact on surrounding tissues and blood vessels of the brain and with a low risk of complications;
- the benign tumor has stopped growing, but at the same time has a negative effect on certain areas of the brain; symptoms of compression of blood vessels and nerve endings are noted.
Brain surgery is contraindicated if:
- exhaustion of the body associated with the patient’s age or long-term illness;
- extensive damage to the brain with tumor growth into surrounding tissues, including if cancer cells have grown into the bone tissue of the skull;
- the presence of metastases in other organs;
- localization of the tumor, which excludes the possibility of its surgical removal;
- the risk of reducing life expectancy after surgical treatment, if without surgery this period is longer.
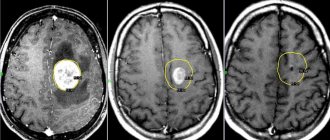
In order to detect contraindications to surgical intervention, a number of additional studies are prescribed, for example, general tests, electrocardiogram, computed tomography, fluorography, angiography.
Contraindications may be temporary, that is, they can be eliminated. So, before the operation it is recommended to carry out some stabilizing measures:
- Reducing increased intracranial pressure. This can be done with medication already on the operating table, during anesthesia.
- Stabilization of the patient’s general condition – normalization of blood pressure, functioning of the cardiovascular and respiratory systems.
- Before the operation, a biopsy is also performed - material is taken for histological examination, that is, a piece of the tumor is sent for examination to clarify the type of tumor. This type of diagnosis can be dangerous due to bleeding. A biopsy is prescribed only for lymphomas (primary) and germ cell cancer.
What will happen to the wound?
A scar will remain on the scalp, but the advantage of this arrangement is that it can be masked with a hairstyle; after a week the scar will not be visible.
Scars may not remain with minimally invasive intervention through the nasal passages or blood vessels; treatment of such wounds is easier.
The dressing is carried out in the hospital on the first day, then a dry cloth - pad accompanies the patient at home. The bandage should not be allowed to get wet; the patient should be helped to keep the bandages dry. You can resort to careful hair washing after a week.
It is important to comply with sanitary standards and wash your hands with soap and water before touching the bandage: this applies to the patient, caregivers and medical staff.
After healing, a thin scar in the form of a white stripe remains at the intervention site, which is successfully hidden in the hair.
Types of surgeries to remove a brain tumor
Removal of intracranial tumors can be carried out in several ways. The main types of operations to remove a brain tumor:
- endoscopic trepanation;
- craniotomy (open craniotomy);
- stereotactic radiosurgery.
Depending on the type of operation, the neurosurgeon makes a decision on the course of the intervention, the type of anesthesia, calculates possible risks and warns the patient about them.
Craniotomy
Craniotomy, or open craniotomy, is usually performed under general anesthesia, but in some cases local anesthesia may be used.
The clear consciousness of the patient during surgery allows the neurosurgeon to control the psychological and physical state of the patient while working on the brain. For example, control of the sensitivity of the limbs, preservation of vision, speech, hearing.
The operation begins with dissection of the soft tissues of the head. Next, it is necessary to remove the bone fragment at the site of the tumor. Excision of the tumor is carried out with a laser, which allows you to simultaneously stop the blood supply to the tumor and stop the bleeding.
After the tumor is completely removed, the bone fragment is placed in place and fixed with metal structures (screws, plates). If cancer cells grow into the thickness of the skull bones, all affected areas are removed, and the hole is closed with an artificial implant (titanium, porous polyethylene).
Brain surgery can last several hours. For the purpose of constant monitoring, the patient is recommended to spend about 2 weeks in the intensive care unit for timely assistance in case of deterioration of the general condition.
Endoscopic trepanation
The location of the tumor in a hard-to-reach place does not allow its removal using an open method.
The operation is performed by inserting an endoscope through an incision in the upper palate or nasal passage. A tumor in the brain, for example, in the area of the pituitary gland, is removed with a special attachment. The excision process is controlled by a sensor on the endoscope. Readings from the sensor are displayed on the monitor, which minimizes damage to surrounding brain tissue.
After the endoscope is removed from the skull, minor hemorrhages may be detected. If the bleeding does not stop, the surgeon decides on the need for craniotomy. A favorable outcome of the operation is characterized by the patient emerging from anesthesia without any complications.
Stereotactic radiosurgery
This method of treating brain tumors allows you to remove the tumor without craniotomy and without anesthesia. The neurosurgeon acts on the tumor with a directed beam, which consists of gamma radiation (gamma knife), a beam of photons (cyberknife) or a stream of protons.
The tumor removal procedure lasts about an hour until all malignant cells are destroyed. The duration of exposure depends on the size of the tumor. The advantage of this method of treatment is that it is not tied to the location of the tumor.
The tumor removal procedure involves exposing cancer cells to ionizing radiation. A course of treatment using a cyberknife is carried out over several days (3-5), depending on the size of the tumor. Each procedure lasts between one and a half hours.
In this case, the patient does not feel any discomfort. Hospitalization for the duration of treatment is not required, since the patient can visit the clinic at the appointed time, undergo a course of radiation exposure and go home. The Gamma Knife procedure is performed under local anesthesia, but hospitalization is also not required.
Complete removal of skull bone fragments
This type of surgery is used when it is necessary to gain access for surgical removal of a tumor through the base of the skull.
Neurosurgeons rarely resort to this method, since the operation is quite complex and there is a high risk of developing various complications. Such surgical intervention is practiced only after consultation with other specialists - otolaryngologist, plastic surgeon, maxillofacial surgeon.
Anesthesia
In almost all cases, the patient is given general anesthesia. An endotracheal tube is inserted into his throat, which is necessary to maintain breathing. Throughout the entire operation, the patient will be in a state of sleep and will not feel anything.
Sometimes the patient is required to be conscious. For these purposes, local anesthesia is used or the patient is taken out of sleep for some time. By asking questions, the doctor checks the activity of the brain and also determines whether certain centers that are responsible for speech, thinking and memory have been affected.
Stereosurgery is performed under local anesthesia or without anesthesia at all, since no punctures or incisions are required in this case.
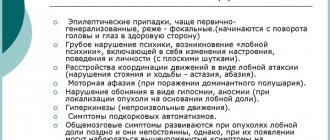
Possible consequences and complications
Complications after surgery to remove a tumor in the brain can lead to a significant deterioration in the patient’s health.
But if the operation is carried out correctly and professionally, the likelihood of consequences developing is low. More often, complications appear after open excision of a brain tumor (craniotomy):
- loss of functions for which the area of the brain in which the operation was performed was responsible;
- incomplete excision of the tumor - repeated surgery may be required;
- wound infection and penetration of pathogens into brain tissue;
- side effects associated with intracranial bleeding;
- swelling of the brain, which leads to epileptic seizures, hypoxia and circulatory disorders.
During surgical intervention, dysfunctions of certain areas of the brain are possible, which manifest themselves:
- decreased visual acuity or complete loss;
- impaired motor functions (partial or complete paralysis);
- disorders of the vestibular apparatus;
- partial or complete amnesia (short-term, long-term);
- influence on the process of urination;
- the appearance of symptoms of mental disorders;
- speech disorders.
Complications and consequences can be either permanent or temporary with the proper course of rehabilitation therapy.
For example, if after surgery there is a partial loss of motor functions, then in 60% of cases mobility is completely restored. Lost vision returns in 86% of patients. The percentage of occurrence of mental disorders after removal of a brain tumor is extremely low. The risk of any abnormalities persists for 3 years after surgery.
The percentage of patients who lose the ability to communicate is only 6%. At the same time, a person loses the skills to care for himself independently, and his mental abilities are extremely reduced.
The result of the operation depends on a large number of factors - the patient’s age, the presence of concomitant diseases, and general health. The worst case scenario is death.
Alarming symptoms
Problems with hemostasis and blood clotting cause severe bleeding. The resulting hematoma is removed with a second operation, thus solving the problem of a bleeding vessel.
The norm is manifestations of dyspeptic disorders: nausea, vomiting. If the patient tries to stand up or raise his head, he may feel dizzy.
Dangerous symptoms are:
- Severe persistent headache
- Decrease in heart rate
- Convulsions
- Pupil dilation.
Look closely and listen to the patient; in case of danger, call a doctor immediately.
Rehabilitation in the postoperative period
Removal of a brain tumor is a fairly serious operation, after which the patient may be unable to work for a long time.
Therefore, it is extremely important to think through all the nuances of restoring the functions of the patient’s body. Rehabilitation after brain surgery depends on the severity of the disease, the age of the patient, and the individual characteristics of the body. The following specialists take part in the rehabilitation process:
- exercise therapy instructor;
- neurosurgeon;
- oncologist;
- speech therapist;
- neurologist;
- psychologist;
- ophthalmologist;
- physiotherapist.
If it is necessary to use chemotherapy or radiation therapy, the involvement of specialists such as a radiologist or chemotherapist is required.
Rehabilitation after removal of a brain tumor begins almost immediately after surgery. Even the slightest delay can affect the restoration of brain activity, and the damage will become irreversible.
Drug therapy is also used for recovery. As a rule, the list of medications consists of drugs that prevent relapses.
The use of supporting agents will help speed up the rehabilitation process after radiation therapy. Since this treatment method can negatively affect the functions of the hematopoietic organs, it is useful to take substances that increase hemoglobin levels and have an antianemic effect - gelatin preparations, folic acid, vitamin B12.
Predictions for speech disorders
After a stroke, it is possible to talk about three outcomes:
- Recovery. Only one in 5 stroke patients can return to work. In addition, after a stroke there is a high risk of having another stroke. 50% have a second stroke within 5 years.
- Disability. Stroke is one of the leading causes of loss of ability and disability in Russia.
- Death. 30% of patients die within a month after a stroke.
A prognosis for a particular patient can only be made by assessing the location and extent of necrosis and ischemia, the cause of the stroke and the general condition of the patient.
Stroke is a serious and very common condition. After a stroke, a person faces a long rehabilitation period. However, the right approach to recovery, rational drug therapy, help from specialists and loved ones can help a person rehabilitate and live a full life.