The autonomic nervous system is the most important “conductor” of the body, which, together with the endocrine system, regulates all bodily functions that do not depend on conscious control. It was described 130 years ago, and it seemed that by now it had been studied almost thoroughly, at least anatomically and physiologically. However, now the French-British scientific team has come to the not unreasonable conclusion that there is a fundamental error in the classical concept of this system: the boundary between its sympathetic and parasympathetic divisions was drawn incorrectly.
The yin and yang of the autonomic nervous system
The autonomic, or autonomic, nervous system is divided into two divisions with almost opposite effects: the sympathetic, which is responsible for the stress response (“fight or flight”), and the parasympathetic, which maintains homeostasis (“rest and digestion”). These departments differ in development during the formation of the body, anatomical structure and biochemistry.
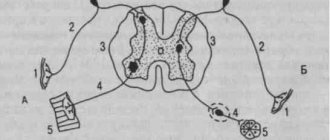
Signals from the autonomic system go from the corresponding nuclei of the central nervous system (brain and spinal cord) along nerve fibers to the neurons of the peripheral ganglia (nerve ganglia), which, in turn, transmit these signals to the internal organs.
In this case, the ganglia of the sympathetic system are located segmentally next to the spine, that is, its preganglionic nerve fibers are short and its postganglionic nerve fibers are long. The nerve nodes of the parasympathetic system are anatomically connected to the organs that they innervate, that is, its preganglionic fibers go along long nerves from the central nervous system, and postganglionic fibers are short.
In all preganglionic and parasympathetic postganglionic fibers, the neurotransmitter is acetylcholine, and in the sympathetic postganglionic fibers, norepinephrine.
A special department of the autonomic nervous system is the intestinal nervous system: in addition to the above structures, it also contains sensory and intercalary neurons, which is why some experts propose to separate it into its own vegetative department. But this is not about her now.
During development, sympathetic ganglia are formed as a result of direct migration of neural crest cells from the neural tube (the precursor of the central nervous system). The formation of parasympathetic ganglia depends on the growth of preganglionic nerve fibers, which deliver neuronal precursor cells to the site of the future ganglion. This difference in ganglion formation is associated with the expression of different transcription factors in future sympathetic and parasympathetic neurons.
Mediators of the sympathetic and parasympathetic nervous system
Read:- I. Neurogenic tumors from the nervous tissue itself.
- I. Opposing Philosophical Systems
- II. Immune system cells
- IV. Anatomy of the organs of the cardiovascular system
- IV. Endocrine system response to hypoglycemia
- V. Organs of the lymphatic system, immune system
- VI. Anatomy of the central nervous system
- VII. Anatomy of the peripheral nervous system
- A) with increased tone of the sympathetic nervous system
- A. Assessment of the state of the hypothalamic-pituitary-adrenal system
Acetylcholine is released in preganglionic fibers of both the sympathetic and parasympathetic nervous systems. It interacts with H-cholinergic receptors (nicotine-sensitive receptors) of neurons of the autonomic ganglia. As a result, excitation is transferred from the preganglionic fiber to the ganglion neuron. N-cholinergic receptors of ganglia, as a rule, are not blocked by curare-like substances (unlike skeletal muscles, where N-cholinergic receptors are highly sensitive to curare), but are blocked under the influence of ganglion blockers, for example, benzohexonium. Regarding nicotine, in small concentrations it excites H-cholinergic receptors, and in large concentrations it inhibits and blocks (including those contained in tobacco smoke).
In addition, the autonomic ganglion contains neuropeptides: methenkephalin, neurotensin, cholecystokinin, substance P, but they have a modulating effect.
Postganglionic fibers of the sympathetic nervous system, as a rule, are monoaminergic (the main transmitter is norepinephrine - 90%, adrenaline - 7% and dopamine - 3%). An exception is that acetylcholine is released in the postganglionic sympathetic fibers of the sweat glands, which interacts with M-cholinergic receptors (muscarine-sensitive), causing stimulation of the sweat glands and sweating.
In order for the effect of norepinephrine to manifest itself, it must interact with adrenergic receptors. There are alpha and beta adrenergic receptors. When interacting with the alpha adrenergic receptor, the permeability of the membrane for sodium ions changes, depolarization occurs and, as a result, excitation and enhancement of organ function. When interacting with beta-adrenergic receptors, there is an increase in potassium flow, hyperpolarization and, accordingly, inhibition and decrease in organ function. An exception is that the interaction of norepinephrine with cardiac beta-AR causes increased cardiac activity. In addition, NA, when interacting with the adrenergic receptor, can increase the activity of adenylate cyclase, which leads to the formation of cAMP (an intracellular messenger - intermediary). This leads to the activation of protein kinases, which are intracellular regulators of the synthesis of various proteins.
The mechanism of self-regulation of transmitter release - NA acts on the presynaptic membrane, which has alpha and beta AR. Interaction with alpha-AR reduces the release of the transmitter, and interaction with beta-AR increases the release of the transmitter (positive feedback).
The final effect depends on which population of adrenergic receptors predominates in the organ on the pre- and postsynaptic membrane.
Alpha-AR blockers - phentolamine, beta-AR - anaprilin (widely used to lower heart rate and blood pressure). Both types of receptors are divided into two subtypes alpha-1 and alpha-2, beta-1 and beta-2 AR. Antagonists:
alpha-1-AR - prazosin, droperidol
alpha-2-AR - rauwolsin, yohimbine
beta-1-AR - practolol, atenolol
beta-2-AR - butoxamine
In general, the sympathetic nervous system contributes to a significant increase in the body’s performance - glycogenolysis, lipolysis, and cardiovascular activity are enhanced, pulmonary ventilation is improved, and blood is redistributed from areas resistant to hypoxia to organs that need oxygen. At the same time, there is inhibition of the gastrointestinal tract, relaxation of the bladder, uterus, spasm of the sphincters, and dilation of the bronchi.
Postganglionic fibers of the parasympathetic nervous system are cholinergic. Acetylcholine, released in nerve endings, interacts with M-cholinoreceptors (muscarine-sensitive) of the effector organ. Muscarine is a fly agaric toxin that activates this type of receptor and causes the same effects as acetylcholine. There are 5 subtypes of M1-M5 cholinergic receptors.
M-ChR blockers - atropine and scopolamine, hemicholine.
Effects of the parasympathetic nervous system: increased gastrointestinal motility, contraction of the bladder muscles, relaxation of the sphincters, narrowing of the lumen of the bronchi, constriction of the pupil, inhibition of cardiac activity, dilation of the vessels of the genital organs, erection, increased secretion of all glands.
Date added: 2015-01-12 | Views: 2647 | Copyright infringement
| | | 4 | | | |
Intuition failed
Since the classic work of the British physiologist Walter Gaskell, it was believed that parasympathetic innervation is carried out by long cranial nerves (oculomotor, facial, glossopharyngeal and - main - vagus), originating in the nuclei of the midbrain and diencephalon and regulating the functioning of the eyes and nasal mucosa , glands and internal organs to the lower parts of the colon, as well as the sacral splanchnic nerves, which begin in the nuclei of the lateral horns of the sacral spinal cord and regulate the functioning of the pelvic organs.
The reason for this was some features of the sacral nerves. Anatomically, they are less branched than the sympathetic nerves of the thoracic and lumbar regions, their ganglia are located further from the spine, and they innervate internal organs that are not reached by the branches of the vagus nerve. Physiologically, the sacral nerves act on some organs in the opposite way to the thoracic and lumbar. And, finally, the organs pharmacologically innervated by them are sensitive to blockers of postganglionic acetylcholine receptors.
Classical idea of the structure of the sympathetic (red) and parasympathetic (blue) nervous systems
Anatomy of the Human Body, Henry Gray, 1918 / Wikimedia Commons
Share
The validity of classifying the sacral splanchnic nerves as a parasympathetic system has already been questioned, since the fibers of the cranial nerves extend from the central nervous system dorsally (from the back), and the sacral splanchnic nerves - ventrally (from the chest and abdomen), like sympathetic fibers. This, in turn, indicates different sources of their development in the embryonic period. However, this did not lead to the rewriting of textbooks.
What is the autonomic nervous system?
The autonomic nervous system is a set of nervous tissue formations that ensure continuous functioning of the human body in accordance with the needs of the external environment. It is the work of this part of the nervous system that is responsible for the timely release of hormones - organic compounds that certain organs perceive as a signal for some action. Thanks to this, a stable composition of the internal environment of the body is maintained, the functioning of the endocrine and exocrine glands, the lymphatic and circulatory systems and other important functional systems of the body is regulated.
All formations of the autonomic, or, as it is commonly called, the visceral or ganglionic nervous system, are divided into parasympathetic, sympathetic and metasympathetic sections.
The sympathetic part is located at a considerable distance from the innervated internal organs and is responsible mainly for the functioning of the organs of the cardiovascular system. Its central part is located in the thoracic and lumbar parts of the spinal cord, and the periphery is formed by numerous clusters of nerve cells that act as sensitive receptors and are located in the paravertebral and more distant nodes from the spine. Activation of this part of the nervous system occurs during stressful situations.
The parasympathetic department is responsible for inhibiting the activity of the cardiovascular system. Numerous peripheral anatomical formations of this department are located directly in the internal organs of the body, and the central ones are located in the brain and spinal cord. The fibers of this section of the ganglion system regulate the functioning of organs such as the eyeball, pupillary muscles, salivary and lacrimal glands, and the mucous membrane of the nasal cavity. An important part of the parasympathetic system is the tenth pair of cranial nerves, which consists of different types of nerve fibers and is responsible for the functioning of all internal organs, including the colon. The intestinal and pelvic organs are innervated by other fibers of the autonomic parasympathetic nervous system. Outside the regulation of this department are the sweat glands and vessels of the extremities.
The metasympathetic nervous system is represented by a combination of formations of nervous tissue located in the walls of internal organs and responsible for their ability to contract. Unlike other parts of the autonomic nervous system, it is not divided into central and peripheral parts and is characterized by a higher degree of autonomy from the central nervous system. Through bundles of nerve fibers of the metasympathetic nervous system, internal organs communicate with each other, thus influencing each other. For example, the lungs and stomach can directly influence the heart, and if central regulation is disrupted, continue to perform their physiological functions for some time. Under the control of this part of the nervous system are intestinal epithelial cells, capillaries, smooth muscle fibers, local endocrine and immune structures.
All parasympathetic activity comes from the head
130 years after Gaskell's paper, researchers at the Paris Research University of Sciences and Humanities and University College London convincingly confirmed such doubts by studying the development of pre- and postganglionic neurons in mice.
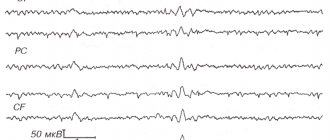
They found that, unlike parasympathetic neuron precursor cells, which express the transcription factors Sox10, Phox2b, Tbx20, Tbx2 and Tbx3, future pelvic ganglion cells express Sox10 and FoxP1, just like sympathetic neurons. Moreover, the formation of the pelvic ganglia turned out to be independent of preganglionic nerve fibers and occurred even in their absence, which is not typical for parasympathetic ganglia. The formation of these ganglia with and without preganglionic sacral fibers is shown in the video above and below, respectively.
On the 14th day of embryonic development, the synthesis of the vesicular acetylcholine transporter (VAChT) occurred in the neurons of the vagus nerve nuclei and there was no nitric oxide synthase (NOS), and in the spinal nuclei of the thoracic, lumbar and sacral nerves, the opposite was true.
The scientists also showed that pelvic ganglion neurons express the transcription factors Isl1, Gata3 and Hand1, like sympathetic ganglion cells, and do not produce the Hmx2 and Hmx3 factors, which serve as markers of parasympathetic ganglion neurons.
A new understanding of the structure of the sympathetic (red) and parasympathetic (blue) nervous systems
I. Espinosa-Medina et al., Science, 2016
Share
The results obtained eloquently indicate that the sacral splanchnic nerves and pelvic ganglia belong to the sympathetic nervous system. Thus, all parasympathetic innervation comes only from the cranial nerves, and the pelvic organs are deprived of it.