Midbrain lesion syndromes.
Quadrigeminal syndrome. When the midbrain is damaged on both sides, there is a violation of upward gaze rotation, combined with a weakening or absence of a direct and friendly reaction to light on both sides and with a violation of the convergence of the eyeballs.
When the pathological focus is localized in one half of the midbrain, the following syndromes may occur.
Knapp syndrome - dilation of the pupil (paralytic mydriasis) on the side of the pathological process in combination with central hemiparesis on the opposite side, manifests itself when the autonomic portion of the third cranial nerve or the parasympathetic nucleus of the midbrain, as well as the pyramidal tract, is affected,
Weber's syndrome is an alternating syndrome that occurs when the base of the cerebral peduncle is damaged in the area where it crosses the oculomotor nerve root. It manifests itself on the affected side as paresis or paralysis of the external and internal muscles of the eye (ptosis of the upper eyelid, ophthalmoparesis or ophthalmoplegia, mydriasis); on the opposite side there is central hemiparesis
Benedict's syndrome is an alternating syndrome when the pathological focus is localized in the tegmentum of the midbrain, at the level of the nuclei of the oculomotor nerve, the red nucleus and the cerebellar-red nucleus connections. It manifests itself on the affected side as pupil dilation in combination with paralysis of the striated muscles innervated by the oculomotor nerve, divergent strabismus, ptosis, and on the opposite side - intentional tremors, sometimes hyperkinesis of the choreoathetosis type and hemihypesthesia.
Superior red nucleus syndrome (Fua syndrome) occurs if the pathological focus is located in the tegmentum of the midbrain in the area where the upper part of the red nucleus is located, and manifests itself on the opposite side as cerebellar hemitremor (intentional tremors), which can be combined with hemiataxia and choreoathetosis. The oculomotor nerves are not involved in the process.
Inferior red nucleus syndrome (Claude syndrome) is an alternating syndrome caused by damage to the lower part of the red nucleus, through which the root of the third cranial nerve passes. On the side of the pathological process, there are signs of damage to the oculomotor nerve (ptosis of the upper eyelid, dilated pupil, divergent strabismus), and on the opposite side there are cerebellar disorders (intentional tremors, hemiataxia, muscle hypotonia).
Nothnagel syndrome is a combination of signs of damage to the nuclear apparatus of the oculomotor nerve with hearing loss and cerebellar ataxia, which can be observed on both sides and at the same time be unevenly expressed. Cerebral aqueduct syndrome—retraction and trembling of the eyelids, anisocoria, convergence spasm, vertical gaze paresis, nystagmus—a manifestation of damage to the gray matter surrounding the cerebral aqueduct, signs of occlusive hydrocephalus.
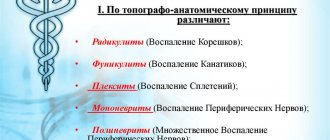
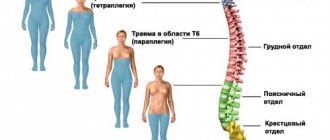
3.polyneuritis and polyneuropathy. Etiology, pathogenesis, clinical picture, diagnosis, treatment, prevention.
Polyneuritis is multiple lesions of peripheral nerves, leading to motor, sensory and autonomic disorders in the areas of innervation of the affected nerves: peripheral paresis of the upper and lower extremities, sensitivity disorders (initially paresthesia, hyperesthesia, then hypoesthesia, anesthesia) in the distal extremities, pain in the course of nerve trunks, cyanosis, pallor or hyperhidrosis of the skin of the hands and feet, brittle nails, hair loss.
Etiology: infections, neuroallergies, intoxication, drug-induced vasculitis, collagenosis, malignant neoplasms, vitamin deficiency, obstruction of internal organs (DM, liver failure, kidney disease, uremia), genetics.
By type of lesion: axonopathies, demyelinating neuropathies.
Course: acute - several days, subacute - several weeks, chronic - several months.
Diagnostic criteria for Guillain-Barré syndrome:
Required for diagnosis:
Progressive muscle weakness in more than one limb;
Tendon areflexia;
Increased protein in the cerebrospinal fluid after 1 week of illness with cytosis of up to 10 cells.
Supporting diagnosis:
Progression of muscle disorders up to 1 month;
Relative symmetry of the lesion;
Sensory disorders with a predominance of muscle-articular sensation;
Damage to cranial nerves (usually 7 pairs);
Recovery from 2-4 weeks of illness;
Autonomic disorders (tachycardia, arrhythmia, postural hypo- and hypertension;
No fever.
Signs that raise doubts about the diagnosis: Severe persistent asymmetry of motor disorders.
2. Persistent dysfunction of the sphincters.
3. The presence of more than 50 leukocytes in the cerebrospinal fluid.
4. A clear level of sensory impairment.
Diagnostics: EMG (no changes => this is a pathology of the muscle itself.)
Treatment: exchange plasmapheresis, hemosorption, antiviral, corticosteroids, anticholinesterase, desensitizing, detoxification, dehydration, correction of metabolic disorders, vitamins, physiotherapy.
Specific and nonspecific prevention of tick-borne encephalitis.
Prevention of acute forms of TE
Prevention: specific: vaccination, especially for persons working in endemic areas; passive-antiencephalitic immunoglobulin; active.
Non-specific: fight against ticks, light-colored clothes with long sleeves, pants directed, san educational work, avoid tall grass, move in the center of the path.
Prevention of chronic forms of TE
Prevention: adequate treatment of acute TE, clinical observation of those who have recovered from the acute form of TE for 2-3 years, for 2-3 years you cannot: vaccinations, physiotherapy, sudden climate change, overheating, pregnancy, alcohol abuse. restorative, immunomodulating therapy.
Ticket No. 34
Dysfunction of midline brain structures according to EEG
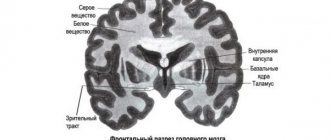
The concept of “midline brain structures” in electroencephalography combines the formations of the medulla oblongata, pons, midbrain, thalamus and hypothalamus, as well as in some cases some sections of the mediobasal formations included in the so-called limbic system (hippocampus, amygdala, orbital cortex, anterior parts of the cingulate gyrus ), and the transverse commissures of the brain, uniting these formations, located in the two hemispheres. There are a number of practical and theoretical justifications for including the listed entities into a unified system. As numerous experimental and clinical studies show, the activity of these formations is characterized by a high degree of interaction between homologous nuclei and formations of the two hemispheres, as well as systems located vertically.
Thus, there is numerous evidence that the modulating influence of limbic formations on the level of functional activity of the brain, the function of attention and the regulation of affective tone is carried out through the systems of the ascending reticular formation of the midbrain. The somnogenic mechanisms of the forebrain also realize their action indirectly through the caudal deactivating and thalamic synchronizing mechanism of the reticular formation1. Experimental studies and EEG recordings in patients through long-term implanted electrodes have also shown bilateral involvement in the pathological activity of the mediobasal limbic systems when the dominant pathological source of impulse is localized in one of the hemispheres, and most often this secondary bilateral synchronization and generalization of pathological activity is realized through the reticular stem and thalamic mechanisms 23. All this information is of great importance for understanding the origin of changes in the EEG with damage to the midline structures of the brain.
These brain structures can be involved in the pathological process in certain types of encephalitis that selectively affect the brainstem, in circulatory disorders in the system of vertebrobasilar arteries that supply the brainstem, in tumors of both the brainstem itself and adjacent formations (cerebellum, base of the skull, pineal gland) , pituitary gland)4.
Rice. 1. EEG of a 34-year-old patient with a brainstem tumor
slowing down the main rhythm to 7-8 Hz. Bilaterally synchronous bursts of 4 Hz θ waves in all leads.
Due to the diffuse and symmetrical projections of the midline brain structures onto the cortex, the changes in electrical activity that occur when they are involved in the pathological process are diffuse and bilaterally synchronous. The most typical sign of damage to the midline structures of the brain is generalized bilateral synchronous θ- and δ-waves. Depending on the severity of the lesion, they can be more or less constant, or occur periodically or in outbreaks (Fig. 1). In this case, the pathological activity is more regular and symmetrical, the lower in the trunk the pathological focus is localized.
Obviously, this is due to less differentiation of the influences of the lower brainstem (rhombencephalic and mesencephalic) parts of the reticular formation on brain activity than the influences of higher lying thalamic and limbic mechanisms56.
Rice. 2. EEG of a 66-year-old patient with a tumor of the posterior cranial fossa
Bilaterally synchronous generalized bursts of a-waves with an amplitude of up to 200 µV in the occipital regions.
In some cases, damage to the midline structures of the brain can manifest itself as bilaterally synchronous generalized bursts of high-amplitude (above 100-120 μV) α-waves (Fig. 2) or β-oscillations with an amplitude of more than 30 μV (Fig. 3).
Rice. 3. EEG in case of cerebrovascular accident in the basilar artery basin
Bilaterally synchronous bursts of p-like oscillations with an amplitude of up to 80 μV.
With damage to the lower brain stem of traumatic, desontogenetic and vascular origin, apparently, due to dysfunction of reticular synchronizing mechanisms, changes in the type of desynchronization can be observed on the EEG78. In the absence of an α rhythm, low-amplitude (<20 μV), polymorphic, predominantly high-frequency activity is recorded in all leads. Low-amplitude EEGs are a normal variant. In this regard, they can only be interpreted as a manifestation of brainstem damage if the clinic is taken into account. The EEG conclusion in this case should be conditional; categorical formulations are unacceptable (Fig. 4).
Rice. 4. EEG for circulatory failure syndrome in the vertebrobasilar system
There is no a-rhythm on the EEG. All leads record activity with a frequency of 13-25 Hz and an amplitude not exceeding 25 μV. Low-amplitude EEG is a normal variant. In the context of clinical data, a decrease in EEG amplitude with a predominance of fast rhythms may indicate dysfunction of brainstem structures.
As a rule, the EEG does not allow us to speak with certainty about the level of damage, since the nature of its changes depends on the specific involvement of synchronizing or desynchronizing mechanisms, localized at all levels, from the bulbar to the frontal limbic cortex, on the nature of this involvement (exciting or destructive), from neurodynamic changes in the interaction of multiple brain nonspecific systems in pathology and, finally, most importantly, from the massiveness of damage to brain structures. However, the experience of many years of diagnostic use of EEG in many laboratories around the world, in some cases verified by special model experimental studies on animals, allows us to outline some general patterns of relationships between certain types of lesions and certain levels of brainstem-median structures.
Brainstem lesion
In this context, by brainstem we mean the international definition, which includes sections ranging from the medulla oblongata to the midbrain inclusive. Considering the limited volume of this formation, most pathological processes always involve, to one degree or another, several of its levels or influence them, therefore it is practically impossible to narrowly isolate changes characteristic of limited sections. It seems reasonable to at least analyze in more detail the data based on cases where the level of the lesion was accurately verified by imaging methods (CT, NMRI) and on autopsy. First, we will analyze the data for ischemic disorders, since they do not cause dislocation and liquorodynamic effects at a distance, which makes it possible to associate the observed EEG changes with the affected structure.
Thrombosis of the basilar artery causes infarctions mainly of the medulla oblongata and the pons; the midbrain and higher levels are affected to a lesser extent, since compensation there occurs through the circle of Willis. Thus, these disorders can be considered as a model of predominant damage to the lower brainstem level (medulla oblongata and pons). They are usually not accompanied by the appearance of slow oscillations in the EEG. In half of the cases, the a-rhythm is preserved with normal reactions to afferent stimulation; in some cases, low-amplitude EEG is observed. A number of observations have described chronic insomnia, which is adequate to the idea of the role of the bulbo-pontine synchronizing reticular formation in the organization of slow-wave sleep. Due to damage at the pontine level to structures associated with the REM stage of sleep, disturbances in the form of its absence, reduction in duration, or dissociation of its components may be observed. Slow oscillations are observed with the addition of ischemic softening at a higher mesencephalic and (or) diencephalic level910111213.
When predominantly affected at the mesencephalic level, generalized bilateral synchronous slow waves or a beta coma pattern with a sleep pattern are observed. With limited mesencephalic destruction, slow-wave activity alternates with periods of normal alpha rhythm, and changes in stages with the presence of REM sleep are noted in the sleep pattern. This is obviously due to the preservation of the pontine mechanism of REM sleep and thalamic nonspecific systems for generating a-activity14.
With massive destructive bilateral lesions of the brainstem including the midbrain, a picture of α-coma occurs. It is assumed that in these cases, the preservation of α-activity is due to the intactness of the thalamo-cortical systems of its generation, and the total destruction of lower-brain synchronizing and mesencephalic desynchronizing mechanisms with the simultaneous switching off of specific and nonspecific systems of ascending activation determines the autonomy and unresponsiveness of the EEG15.
It should be noted that the data presented above relate to irreversible destructive, often vital, disorders. In cases where the disorders manifest themselves mainly as clinical symptoms without gross morphological disturbances of the stem structures, EEG changes can be milder and have a transient nature, according to the phase of the pathological process.
Here it is appropriate to discuss the opinion, widespread in Russian literature and practice, that lesions of the caudal sections of the trunk lead to the appearance of bilaterally synchronous slow or hypersynchronous waves in the posterior sections, and lesions of the rostral sections of the trunk - in the anterior sections1617. Analyzing the quoted messages, the following conclusions can be drawn:
- observations concern the children's age group;
- in the above cases, occlusive hydrocephalus of the third ventricle of the brain occurs;
- In not a single case are there pathohistologically verified indications of damage to specific stem structures, and in a number of the reported observations there is no adequate noso-syndromic diagnosis;
- analysis of the reported EEGs suggests that slow activity in the posterior leads fully corresponds to the characteristics of the “slow α-variant” of the EEG.
Thus, it is obvious that the discussed EEG changes cannot be interpreted specifically as a manifestation of the pathology of the lower brainstem. In cases of occlusive lesions at the level of the posterior cranial fossa, they are a symptom at a distance - a consequence of dysfunction of the thalamic nuclei surrounding the third ventricle and associated with the generation of the α rhythm, as a result of mechanical hydrocephalic and hyperhydration effects18. In childhood and adolescence, the slow αa variant is much more common than in adults and reflects a significant variation in the rate of maturation of normal midline structures19. In conditions of hypertensive hydrocephalus of the third ventricle, which occurs in the publications cited above, a delay in the normal increase in the frequency of the dominant rhythm is a natural consequence of dysfunction of the diencephalic, i.e. rostral midline brain structures, and not a direct result of unproven damage to the lower brainstem levels. Thus, the idea of a predominant predominance of bilateral synchronous oscillations in the anterior sections with rostral lesions, and in the posterior sections with caudal lesions of the trunk, seems unfounded, and diagnostic conclusions based on this criterion are arbitrary and inadequate.
To summarize, we can say that EEG changes with damage to brain stem structures are symmetrical in nature and, with the exception of disturbances such as desynchronization and, accordingly, a decrease in amplitude, are manifested by high-amplitude bilaterally synchronous a-waves, bilaterally synchronous slow waves or bursts of high-amplitude oscillations. In this case, the higher the lesion is localized, the greater the probability of the appearance of slow waves, the amplitude and degree of frequency slowdown:
- lower brainstem lesions are most often manifested by low-amplitude EEG or high-amplitude α-oscillations,
- lesions of the middle level of the trunk - θ-waves,
- upper trunk (midbrain and mesodiencephalic junction) - δ waves. The lower the level of damage, the higher the regularity and rhythm of activity.
Damage to the medial structures of the hemispheres
rice.
1. EEG of a 39-year-old patient with a craniopharyngioma compressing the hypothalamic regions. Bilaterally synchronous generalized δ waves.
Bilateral or medially localized damage to the hypothalamic structures leads to the appearance of bilaterally synchronous bursts or constant bilaterally synchronous slow oscillations in the EEG. Most often these are δ-band waves (Fig. 1). Similar changes are observed with bilateral lesions of the thalamus (Szirmai I. et al., 1977).
Rice. 2. EEG of a 38-year-old patient with a tumor of the mediobasal regions of the left hemisphere of the brain involving the thalamic nuclei
Sopor. Generalized δ-waves (frequency 1-3 Hz, amplitude up to 200 μV), occasionally predominant in amplitude in the left hemisphere.
Lateralized lesions of the thalamus typically produce bilaterally synchronous widespread δ waves with amplitude predominance on the affected side (see Fig. 2). Sometimes gross destructive lateralized thalamic lesions give a picture of symmetrical bilaterally synchronous or even slow oscillations predominant on the intact side. This is due to the fact that due to powerful transverse adhesions that connect both thalami essentially into a single rhythmogenic structure, a single pathological pattern of activity is formed that unites both thalami. However, due to damage to one of the visual thalamus by a destructive process and disruption of its connection with the cortex of the corresponding hemisphere, pathological activity on the affected side turns out to be less regular and pronounced20. In such cases, a test with light rhythmic stimulation can provide significant assistance in determining the localization of the pathological focus. As already indicated, with this test, assimilation of the EEG rhythms of light flickers is observed. This effect occurs due to the functioning of thalamocortical relays. In case of disruption of thalamocortical connections and damage to the nuclei of the thalamus, the transmission of rhythmic impulses from the periphery to the cortex is disrupted, and on the affected side the rhythm assimilation reaction is either absent or poorly expressed, while on the side of the morphologically intact thalamus the disappearance of slow pathological activity and its replacement by rhythmic activity are observed. activity corresponding to the frequency of light flickers.
Rice. 3. EEG of a 43-year-old patient with glioma of the rostral part of the corpus callosum
Against the background of diffuse changes, there are flashes of asymmetrical δ-oscillations of irregular shape in the homotopic sections of both hemispheres, predominant in the anterior sections, respectively, the projections of the affected fibers.
In the absence of the possibility of presenting rhythmic light stimulation or in a severe comatose state, in which the reaction of rhythm assimilation may be absent, it is possible to use any other activating stimuli: sound, tactile, nociceptive. In this case, on the side of the morphologically intact hemisphere, an activation reaction occurs in the form of a restructuring of the rhythm (usually towards an increase in frequency and a decrease in amplitude), while on the affected side monotonous background activity remains without noticeable changes in response to stimulation. The described tests are effective for lateralized lesions of any midline structures, not just the thalamus, when the background EEG does not provide clarity regarding the side of the lesion. A severe destructive lesion of the corpus callosum causes the appearance of widespread slow oscillations in the symmetrical parts of the hemispheres, mainly in the areas of projection of the fibers of the corpus callosum corresponding to the lesion. Their peculiarity is that, arising simultaneously in homotopic sections of both hemispheres, they, however, as a rule, are asymmetrical and not strictly bilaterally synchronous. Violations of bilateral synchrony and symmetry are due to the fact that the corpus callosum is one of the most important mechanisms for bilateral synchronization of the activity of the hemispheres and, accordingly, the destruction of this structure by the pathological process causes a violation of the coherence of their activity2122 (Fig. 3).
Rice. 4. EEG of a 66-year-old patient with a tumor of the posterior cranial fossa
Bilaterally synchronous generalized bursts of a-waves with an amplitude of up to 200 µV in the occipital regions.
Pathological processes in the structures of the limbic system, depending on the nature and location, cause various EEG changes. Lesions of the nuclei of the septum, fornix, preoptic cortex, and cingulate gyrus, even with unilateral involvement, can produce nonlateralized slow bilaterally synchronous waves, mainly in the δ range, which is due to their midline localization and close bilateral functional connections. The amplitude of pathological fluctuations may predominate on the affected side. With bilateral lesions, stable amplitude asymmetries are not observed (see Fig. 4).
Footnotes
- Bremer E. Preoptic hypnogenic area and reticular activating system / Arch. Ital. biol., 1973, v. III, P-85-111.
- Bekhtereva N.P. Smirnov V.M., Bondarchuk A.N. Physiology and pathophysiology of deep structures of the human brain. L-M. Medicine. 1967.
- Wieser HG Spontane und evozierte Spitzentatigkeit im Tiefen- und Ober-flachen-EEG / EEG-Labor, 1988, Bd. 10, s. 8-30.
- Boldyreva G.N. Electroencephalography for tumors of basal localization // Clinical electroencephalography. - M: Medicine, 1973. - p. 147-172.
- Mayorchik V.E. EEG changes depending on the location of the brain tumor. Clinical electroencephalography. – M.: Medicine, 1973, p. 106-146.
- Grindel O.M. Electroencephalogram in traumatic brain injury. In the book: Clinical electroencephalography. M. Medicine. 1973, p. 213-259.
- Zenkov L.R., Kuuz R.A., Paramonov L.V. Electrical activity of the cerebrum and cerebellum in cranio-vertebral anomalies. In the book: Conference of young neurosurgeons. M., 1970.
- Grindel O.M. Electroencephalogram in traumatic brain injury. In the book: Clinical electroencephalography. M. Medicine. 1973, p. 213-259.
- Markand ON Electroencephalogram in “locked-in” syndrome / Electroenceph-alogr. Clin. Neurophysiol., 1976, v. 40, p. 529-534.
- Cummings JL, Greenberg R. Sleep patterns in the “locked-in syndrome.” Elec-troencephalogr. Clin. Neurophysiol. 1977, v. 43, p. 27—271.
- Patterson JR, Grabois M. Locked-in syndrome: A review of 139 patients / Stroke, 1996, v. 17, p. 758-764.
- Psatta DM, Matei M. Cerebral evoked potentials in the chronic vertebral insufficiency / J. Neurol, and psyciat., 1993, v. 31, No. 3-4, p. 221-238.
- Kamondi A., Szirmai I., Topographic EEG Analysis in two patients with basilar thrombosis / Clin, electroencephalogr., 1993, v. 24, p. 138-145.
- Markand ON, Dyken ML Sleep abnormalities in patients with brain stem lesions I Neurology, 1976, v. 26, p. 769-776.
- Fung PC, Tucker RP Alpha-rhythm and alpha-like activity in coma. Clin. Elec-troenceph. 1984, v. 15, No. 3, p. 167-172.
- Galkina N.S. Electroencephalograms of children in normal and pathological conditions. Clinical electroencephalography. - M.: Medicine, 1973. - p. 270-285.
- Blagosklonova N.K. Assessment of pathological signs on the EEG of children and adolescents. In the book: Blagosklonova N.K., Novikova L.A. Children's clinical electroencephalography. M., Medicine, 1994. p. 54-61.
- Zenkov L.R., Dikovskaya T.A. On the question of the influence of intracranial hypertension on the electrical activity of the brain. Ink.: Proceedings 1 MOLMI named after I.M. Sechenov, M., 1963.
- Eeg-Olofsson O. The development of the electroencephalogram in normal children and adolescents from the age of 1 through 21 years / Acta, pediat. scand. Suppl. 1970, v. 208, p. 1-47.
- Zenkov L.R. New directions in clinical neurology. Sov. honey. 1976, No. 11, p. 43-45.
- Montplaisir J., Nielson T., Cote J., Boivin D., Rouleau I., Lapierre G. Interhemispheric EEG coherence before and after partial callosotomy / Clin, electroencephalogr., 1990, v. 21, p. 42-47.
- Nagase Y., Terasaki O., Okubo Y., Matsuura M., Torn M. Lower interhemispheric coherence in a case of agenesis of corpus callosum / Clin, electroencephalogr., 1994, v. 25, p. 33-39.
Signs of disturbances in the development of brain blocks
At the beginning of the 20th century, A. R. Luria divided (conditionally) the human brain into 3 functional blocks, the interaction of which is necessary for any mental activity.
1 – energy block - is formed from the prenatal period to 2-3 years, is responsible for regulating the tone of the body and includes: the reticular formation of the brain stem, nonspecific structures of the midbrain, diencephalic sections, the limbic system, the mediobasal sections of the cortex of the frontal and temporal lobes of the brain.
The 1st block of the brain is primarily responsible for the emotional “reinforcement” of mental activity (the experience of success or failure).
This brain block is involved in organizing attention, memory, emotional state (especially fear, pain, pleasure, anger), processes a variety of information about the state of internal organs and regulates these states, and also maintains the general tone of the central nervous system.
Everything that happens to the mother during pregnancy (illness, psychological trauma, taking medications, etc.) leaves its mark on the formation of 1 brain block.
Block 2 - receiving, processing and storing information - is formed from 3 to 7 years and includes the main analytical systems: visual, auditory and cutaneous-kinesthetic, cortical zones which are located in the posterior parts of the cerebral hemispheres.
A special feature of this block is the six-layer structure of the cortex:
— primary zones (providing reception and analysis of information coming from outside). When damaged, a disturbance in the perception of individual signs of a perceived stimulus of one modality occurs (blind spot, hemeanopsia, tone scale disorder, anesthesia, etc.).
— secondary zones (performing the functions of synthesizing information from one analyzer). With a lesion, there is a violation of the synthesis of individual signs of a perceived stimulus into a holistic image of one modality (agnosia, aphasia).
— tertiary zones (the main task of which is a comprehensive synthesis of information). Damage to the tertiary zones leads to disruption of the complex synthesis of stimuli coming from different analyzers, which manifests itself in a violation of orientation in space. Moreover, according to the law of progressive lateralization, when the tertiary zones of the right hemisphere are damaged, object orientation in space is disrupted, and when similar zones of the left hemisphere are damaged, symbolic orientation in space suffers.
Block 3 - the block of programming, regulation and control over the course of mental activity - is formed from 7 to 15 years, includes the motor, premotor and prefrontal parts of the cortex of the frontal lobes of the brain. Full maturation of the frontal lobes occurs by age 20.
When the third functional block of the brain is damaged, the nature of the dysfunction is related to which particular apparatus is damaged. When the motor cortex is damaged, paresis and paralysis of individual muscle groups are observed. Damage to the premotor cortex leads to the disintegration of motor skills, damage to the prefrontal regions manifests itself in a violation of conscious goal-directed activity, and in this case, goal-directed behavior is replaced by “field” behavior
Anatomy
The red nucleus (nucleus ruber) is a large collection of neurons along almost the entire length of the midbrain.
Its color is explained by the large number of capillaries or the presence of iron-containing pigment in neurons. The structure is divided into an anterior small cell (parvocellular) and a posterior (magnocellular) large cell part.
| Part of the red core | Parvocellular nucleus ruber | Magnocellular nucleus ruber |
| Neurotransmitters | GABA, glutamate | Glutamate |
| Meaning | Connected to the cerebellum Gives rise to the red nuclear olivary tract | Gives rise to the rubrospinal tract |
| Evolution | Associated with motor learning processes, developed in humans | Ancient motor center |
There are several pathways connecting the structure with other parts of the brain. The main ones:
- The corticorubral tract (corticorubral tract, tractus corticorubralis) stretches from the cortex to the nucleus. It runs parallel to the corticospinal tract of the pyramidal system. This shows parallels between the pyramidal and extrapyramidal systems.
- The cerebellorubrospinalis tract (tractus cerebellorubrospinalis) follows the motor neurons of the spinal cord, but before that it passes through the red nucleus. Connections with the cerebellum provide correction of movements.
- The neurons of the magnocellular part give rise to the rubrospinal tract (red nuclear spinal tract, tractus rubrospinalis, rubrospinal tract). Its fibers immediately pass to the opposite side of the midbrain and then descend to the motor neurons of the spinal cord. In humans, the rubrospinal tract largely determines the movements of the limbs.
- Rubroolivary tract.
The structure also receives signals from the basal ganglia and sends impulses to the cortex.
The function of the red nuclei is to integrate information from the cortex and cerebellum and control underlying structures.
Red cores provide:
- Exit of the extrapyramidal system to the spinal cord.
- Determination of the tone of all skeletal muscles of the body.
- Coordination of posture together with the cerebellum.
- Regulation of unconscious automatic movements, such as changing body position.