5.1. ARC OF AUTONOMOUS REFLEX
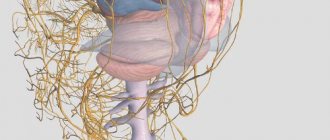
Like the somatic reflex arc, the autonomic reflex arc
consists of three links: sensitive (sensory, afferent), associative intercalary) and effector. For example, in the autonomous reflex arc of the spinal level (Fig. 5.1), the sensitive link is formed by cells of the spinal or peripheral ganglia. It can be common to the autonomic and somatic reflex arcs.
The peripheral processes of sensitive cells branch in internal organs, skin, vessel walls, etc., while the central ones synaptically contact the interneurons of certain segments. The second link of the same arch can be simplistically represented as a cluster of neurons in the lateral horns of the spinal cord. Their processes leave the spinal cord as part of the ventral roots, enter the somatic nerve trunks and from here, in the form of white connecting branches, are directed to the nodes of the sympathetic trunk. Here some of them are switched to effectors
| Rice. 5.1 Schematic diagram of the arc of autonomous (right) and somatic (left) reflexes 1 - spinal cord, 2 - sensory neuron, 3 - spinal ganglion (spinal ganglion), 4 - dorsal root, 5 - intercalary (preganglionic) neuron of the arc of the autonomic reflex, 6 - ventral root, 7 - preganglionic (prenodal) nerve fiber, 8 - sympathetic paravertebral ganglion (sympathetic trunk node), 9 - white connective branch, 10 - motor (postganglionic) neuron of the arc of the autonomic reflex, 11 - somatic nerve, 12 - postganglionic (post-nodal) nerve fiber, 13 - gray connecting branch, 14 - visceral branch, 15 - sympathetic prevertebral ganglion (mesenteric plexus node), 16 - intestine, 17 - effector neuron of the functional module of the metasympathetic nervous system, 18 - functional module of the metasympathetic nervous system, 19 - interneuron of the functional module, 20 - sensitive neuron of the functional module, 21 - motor somatic fiber, 22 - motor neuron of the somatic reflex arc, 23 - interneuron of the somatic reflex arc . |
cells. The third link is a nerve cell that has migrated from the spinal cord to one of the peripheral nodes.
The nodes can be located either near the spine (paravertebral),
either in the nerve plexuses near the internal organs
(prevertebral),
or, finally, in the walls of the internal organs
(intramural).
The arcs of local reflexes at the ganglionic level can close in the prevertebral and intramural ganglia, so that in this case all the components of the reflex arc are located on the periphery near or directly in the wall of the executive organ. In this case, sensory and efferent fibers can pass through the same nerve trunk.
5.1.1. Division of the autonomic nervous system
The autonomic nervous system is divided into sympathetic, parasympathetic
and
metasympathetic
parts, or divisions (Fig. 5.2). This division has certain functional and structural bases. They relate to all three main parts of the reflex arc. According to A. A. Zavarzin, in the process of development, with the appearance of bilateral symmetry and differentiation of the head and tail ends, the division of the nervous system into somatic and autonomic began. From this system a part of the main three-member apparatus emerged, retaining its connection with the somatic system. Due to the more uniform and less complex organization of the visceral organs than the organs of movement, special properties appeared that developed from the general properties of the unified nervous system. In this way the sympathetic, parasympathetic and metasympathetic nervous systems arose.
In turn, the development of parts of the autonomic nervous system probably proceeded in parallel, which explains the presence of a single principle in each of them - a parallel apparatus. In the process of evolution, this apparatus developed special properties that were characteristic of each of the parts, but developed from a single nervous system. Thus, in the metasympathetic part, the sensory apparatus became isolated, its own pacemaker, an interneuron processing network and an effector neuron with its own mediator appeared.
| 1 - sacral spinal cord (S), 2 - thoracolumbar spinal cord (T-L) 3 - cervical spinal cord (C), 4 - medulla oblongata, 5 - midbrain, 6 - sympathetic trunk (paravertebral ganglia ), 7— parasympathetic nodes of the head, 8— postganglionic fibers, 9— (celiac) solar plexus and its nodes, 10— caudal mesenteric plexus and its nodes, preganglionic nerve fibers, 12— pelvic nerve, 13— salivary glands, 14— internal muscles of the eye, 15— vessels of the brain and its membranes, 16— trachea, bronchi, lung, 17— functional modules of the metasympathetic nervous system, 18— stomach, 19— heart, 20— skeletal muscle, 21— duodenum, 22— pancreas , 23— vessels of internal organs, 24— liver, 25— adrenal gland, 26— colon, 27— kidney, 28— bladder, 29— testes, 30— uterus, 31— skin |
provision. In other words, lower reflex centers appeared, located directly in the walls of the executive organs. The sympathetic and parasympathetic departments have arcs with the participation of the spinal cord and the formation of their own centers - the nuclei of the spinal cord and brain, as well as a higher center - the hypothalamic region.
Embryonic source
The cells of the autonomic nervous system in mammals serve as a ganglion plate, which is divided into somites, which subsequently give rise to the sympathetic and parasympathetic nervous system. Their peripheral part, as well as the metasympathetic nervous system, are formed as a result of further migration of neuroblasts into the walls of internal organs.
Histology.RU
Material taken from the site www.hystology.ru
The autonomic part of the nervous system includes higher autonomic centers localized in the diencephalon in the region of the third ventricle, autonomic nuclei of the gray matter of the trunk and spinal cord, as well as peripheral nerve ganglia.
In contrast to the reflex arcs of the somatic nervous system, the motor neuron of the reflex arcs of the autonomic department is not part of the gray matter of the central nervous system, but in one of the peripheral ganglia.
The autonomic nervous system is represented by the parasympathetic and sympathetic systems. The parasympathetic nervous system includes neurons of the cranial and sacral regions of the brain and the ganglia associated with them. The sympathetic nervous system unites the neurons of the thoracolumbar region of the brain and the associated prevertebral and paravertebral ganglia. Sympathetic nerve fibers innervate all organs, while the parasympathetic nervous system innervates only organs that have developed from the embryonic gut or in connection with it.
Most internal organs receive both sympathetic and parasympathetic nerve fibers.
The efferent link of autonomic reflex arcs is two-membered. The central neuron is always located in the brain or spinal cord. The second neuron (peripheral) in the sympathetic nervous system lies in the prevertebral or paravertebral nodes, and in the parasympathetic nervous system - in or near the organ (Fig. 180).
In the parasympathetic nervous system, both neurons are cholinergic. The presynaptic pole of both the first and second neurons contains small, light synaptic vesicles (40 - 60 nm) and single large electron-dense vesicles.
In the sympathetic nervous system, the first neuron is cholinergic, the second is adrenergic (transmitter - norepinephrine). Morphologically, adrenergic synaptic vesicles (30 - 50 nm in diameter) are characterized by an electron-dense core (granular synaptic vesicles). In addition to the granular vesicles characteristic of adrenergic synapses, large granular vesicles are also detected in their composition, as in cholinergic synapses.
Rice. 180. Simple autonomic reflex arc:
1 - spinal cord; 2 - spinal node; 3 - anterior root; 4 - posterior horn; 5 - lateral horn; 6 - anterior horn; 7 - sensitive (afferent) neuron of the somatic and sympathetic nervous system; 8 - central (efferent) neuron of the autonomic nervous system; 9 - motor (efferent) neuron of the anterior horns; 10 - node of the sympathetic trunk; 11 - solar plexus node; 12 - intramural node (nerve plexus node of the esophagus); 13, 14, 15 - peripheral (efferent) neurons of the autonomic nervous system; 16 - preganglionic fibers of the efferent pathway of the autonomic nervous system; 17 - postganglionic fibers of the efferent pathway of the autonomic nervous system; 18 - efferent pathway of the somatic nervous system; 19 — wall of the esophagus; 20 - striated muscles; 21 - microscopic structure of the peripheral nodes of the autonomic nervous system; 22 - multipolar nerve cell; 23 - glial cells; 24 - nerve fiber.
Rice. 181. Nerve cells of the autonomic ganglion:
1 - long-axon nerve cell; 2 - axon; 3 - equilateral nerve cell; 4 - nuclei of glial cells.
vesicles with a diameter of 60 - 120 nm (1 - 5% of the total).
In the sympathetic nerve ganglia, in addition to the multipolar neurons characteristic of them, there are groups of small granule-containing intensely fluorescent cells (MYF cells). They are characterized by short processes and the presence of granular vesicles in the cytoplasm. By fluorescence and submicroscopic structure, their vesicles correspond to the vesicles of the cytoplasm of adrenal medulla cells. It is assumed that they participate in the conduction of nerve impulses from preganglionic fibers to ganglion neurons (the role of interneurons). MIF cells are considered as an intraganglionic inhibitory system. Excited by preganglionic synapses, they release catecholamines, which inhibit the transmission of nerve impulses from preganglionic fibers to the sympathetic neurons of the ganglion.
Intramural nerve plexuses . A significant number of neurocytes of the autonomic nervous system are concentrated in the nerve plexuses of hollow organs: the digestive tract, heart, bladder, etc. The nerve ganglia of the plexuses contain efferent, receptor and associative neurons. Morphologically, three types of nerve cells are distinguished in the intramural nerve ganglia (Fig. 181).
Cells of the first type of Dogel (long-axonal neurocytes) are characterized by a long axon and many branching dendrites. Cells of the second Dogel type (equal-processed neurocytes) contain several processes, among which the axon cannot be morphologically identified. It was experimentally established that it ends with a synapse on cells of the first type. Cells of the third type form synaptic connections with the dendrites of neurons in neighboring ganglia. In the wall of the gastrointestinal tract there are three nerve plexuses: subserosal, intermuscular and submucosal, containing ganglia of nerve cells.
The most massive intermuscular nerve plexus is located in the muscular layer of the organ between the longitudinal and circular layers. Neurohistologically, electron microscopically, histochemically and neurophysiologically, the specificity of this plexus has been revealed, making it possible to compare it with the central nervous system in a number of ways. In particular, the intermuscular nerve plexus of the intestine is also covered with a connective tissue membrane, delimited from the nervous tissue by a basal membrane. The nervous plexus has its own blood supply system in the form of its own capillary network, localized outside the capsule. Capillaries and connective tissue do not penetrate into the ganglion parenchyma.
The plexus capsule contains 2–3 layers of collagen fibers, separated from each other by flat cells. Within each layer, the fibers are oriented parallel, without forming bundles. In the cytoplasm of capsule cells, free ribosomes, mitochondria and pinocytotic vesicles are distinguished. The latter indicate the participation of these cells in the processes of transport of substances.
Experiments have shown that the endothelium of the capillaries and the plexus capsule are involved in the formation of the blood-nerve plexus barrier, which prevents the penetration of marker molecules into the latter.
Neuroglia of the ganglia of the intermuscular nerve plexus are not differentiated (unlike the extramural nodes) into satellite capsules of neurocytes and lemmocytes of fibers. Gliocytes simultaneously border the pericarpones of neurons, cover groups of axial cylinders and synaptic formations. The cytoplasm of gliocytes is poor in organelles. They contain small cisterns of granular endoplasmic reticulum, single mitochondria and free polyribosomes.
The neurocytes of the ganglia of the intermuscular nerve plexus are characterized by an abundance of organelles. Large Golgi complexes and endoplasmic reticulum cisterns together form a dense network of membranes in cells. Numerous ribosomes are localized both freely and on the membranes of the endoplasmic reticulum. The granular endoplasmic reticulum is evenly distributed and does not form chromatophilic clumps.
The ganglia of the intestinal myenteric nerve plexus contain efferent and afferent neurons (Fig. 182). Using fluorescence and electron microscopy, excitatory cholinergic and inhibitory adrenergic synapses are detected on cells of the first Dogel type.
With few exceptions, intramural neurons of the intestine are non-adrenergic, but they are supplied with adrenergic synapses mainly on the axons of nerve cells of the prevertebral ganglia. Electron microscopically, these synapses are characterized by granular synaptic vesicles (30 - 60 nm) typical of adrenergic elements.
Using fluorescence microscopy, it was established that most neurons in the plexus have adrenergic synapses. The absence of fluorescent fibers during transection of the mesenteric nerves indicates that adrenergic synapses in the intramural plexuses are formed by the endings
Rice. 182. Diagram of the intramural plexuses of the digestive tract:
1 - submucosal plexus; 2 - myenteric plexus; 3 - postganglionic sympathetic fibers; 4 - spinal afferent fibers; 5 - sympathetic preganglionic fibers; 6 - vagal afferent fibers; 7 - afferent fibers of local reflex pathways; 8 - annular muscle layer; 9 - longitudinal muscle layer; 10 - serous layer; 11 - mucous membrane (according to Nozdrachev, 1978).
axons of neurocytes of pre- or paravertebral ganglia.
In the intestine, in addition to cholinergic neurocytes, there are inhibitory purinergic neurons that secrete purine compounds as a mediator. Perikaryons and their processes contain characteristic electron-dense vesicles 100 nm in diameter. Purinergic neurons cause descending inhibition of the digestive tract, which is part of the peristaltic reflex. Unlike purinergic adrenergic nerves, they cause reflex inhibition of peristalsis by inhibiting intramural cholinergic excitatory neurons (Burstock and Costa, 1979).
Reviews (0)
Add a review
Features of the structure of the autonomic reflex arc
The path that nervous excitation passes from interoceptors to the central nervous system, and from it to the viscera, is called the autonomic reflex arc
(rice.). Sensory neurons that receive information from internal organs are located in the spinal ganglia or sensory ganglia of the cranial nerves. In contrast to a similar somatic reflex arc (for example, the musculocutaneous reflex), in the autonomic nervous system the efferent link always consists of two neurons. The peripheral processes of sensory neurons have sensitive nerve endings - interoreceptors - in all internal and other organs, skin, and vessel walls. The anatomical features of the structure allow the receptors to selectively respond to only one specific type of energy, which is converted into a nerve impulse. The central processes of sensory neurons enter the brain and reach the vegetative nuclei, where they form synapses (contacts) with intercalary (switching) neurons.
Intercalated autonomic neurons located in the nuclei of the brainstem or spinal cord are preganglionic (prenodal)
neurons.
Efferent neurons that conduct impulses to internal organs and are located in the autonomic ganglia are ganglionic
neurons; their processes are called
postganglionic
nerve fibers. The bodies of effector (motor, secretory and other) neurons form nodes lying near the spine (perivertebral) as part of the right and left sympathetic trunks, in the walls of internal organs (intraorgan nodes), as well as near the internal organs (periorgan nodes). The axons of effector (third) neurons have effector nerve endings in organs.
Rice. . Neuronal composition of the reflex arc of the autonomic (vegetative) nervous system.
As noted above, in the autonomic nervous system local
reflex arcs formed by sensory neurons in the intraorgan plexuses (type P Dogel cells). The implementation of local visceral reflexes can occur without the direct participation of the central nervous system, i.e. autonomously. In these cases, the closure of the reflex arcs occurs at the level of the visceral plexuses or autonomic ganglia.
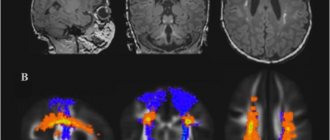
Along with the autonomic neurons located in the nuclei of the brainstem and spinal cord, there are also other autonomic nerve centers in the brain that occupy a higher hierarchical position. These are numerous nuclei in the hypothalamus
, exerting descending regulatory influences (neurogenic regulation) on the stem and spinal vegetative centers, or - through
the pituitary gland and other endocrine glands
- directly on the functioning of internal organs (humoral regulation).
The higher centers that control autonomic functions are located in cortex
, namely in
the frontal, parietal and temporal regions
. Here there is a synthesis of the vegetative and animal functions of the entire human body, as well as their coordination with its psycho-emotional activity.
By controlling the work of internal organs and regulating metabolism, the autonomic nervous system has different, sometimes opposite, effects on them. Under its influence, it is possible to both narrow and expand the lumen of blood vessels, increase or decrease the frequency of heart contractions, increase or decrease the secretory activity of various glands, increase or decrease the level of metabolism in organs and tissues, etc. According to the nature of the effect on the innervated organs various parts of the ANS, the peculiarities of their anatomical structure, as well as the different sensitivity of autonomic ganglia neurons to certain biologically active substances, the autonomic nervous system is divided into sympathetic and parasympathetic
parts.
Functional manifestations of vital activity of internal organs under the influence of sympathetic
nervous system are characteristic of conditions
increased activity of the body (physical and mental stress), and parasympathetic
- for its relative peace. For example, irritation of sympathetic nerve elements causes an increase in heart rate, narrowing of blood vessels and increased blood pressure, increased respiratory movements, weakened intestinal motility, and dilated pupils. Excitation
parasympathetic nerves; elements, on the contrary, leads to a decrease in heart rate, lower blood pressure, increased intestinal motility, etc. However, these functional differences cannot be considered as direct antagonism. Both parts of the autonomic nervous system work in concert, functionally complementing each other.
Sympathetic part of the ANS
the nuclei belong to its central section
, located in the lateral horns of the spinal cord from the VIII cervical (I thoracic) to the II lumbar segment.
The peripheral part of the sympathetic part includes the paired sympathetic trunk
, located on the sides of the spinal column (right and left) with its
connecting branches (white and gray)
,
nerves
going from the sympathetic trunk to the internal organs and vessels, to the large sympathetic plexuses located in the abdominal cavity and pelvic cavity,
nerve endings
sympathetic nature.
The sympathetic trunk (trancus simpatihicus) is a paired formation; it consists of a chain of nerve ganglia located on the sides of the spinal column along its entire length (Fig.). All nodes of the sympathetic trunk are interconnected by internodal branches. The nodes of the sympathetic trunk retain some signs of metamerism, but complete correspondence between the vegetative nodes and body segments is not observed. The sympathetic trunk is divided into: the cervical region, represented by the cervical nodes, the thoracic, lumbar, sacral and coccygeal regions, also represented by the corresponding vegetative nodes.
In the sympathetic part of the autonomic nervous system, preganglionic neurons arise from the spinal cord only in its thoracic and partially lumbar regions. The bodies of preganglionic neurons lie in the intermediolateral nuclei of the lateral horns of the spinal cord. These nuclei can be traced at the level of all thoracic (Th1-12) and upper two lumbar (L1-2) segments of the spinal cord.
Preganglionic sympathetic fibers exit the spinal cord as part of the anterior roots of the spinal nerves. Their axons are covered with a myelin sheath and therefore form white connecting branches extending from the spinal nerve. Each such branch connects
Rice. The structure and areas of innervation of the sympathetic part of the autonomic nervous system
spinal nerve with one of the nodes of the sympathetic trunk on its side (Fig.). These sympathetic nodes are called paravertebral nodes
or
paravertebral
ganglia.
Some of the axons of preganglionic neurons end with synapses on the bodies of ganglionic neurons of the corresponding sympathetic nodes. The rest follow in transit through the node and continue to other nodes more distant from the spine, located in the visceral plexuses ( prevertebral
or
prevertebral
nodes), where they switch to efferent neurons.
Neurons located in the nodes of the sympathetic trunk give rise to postganglionic unmyelinated nerve fibers, which, as part of the gray connecting branches, are sent to each spinal nerve. Some postganglionic nerve fibers in the form of independent nerves or branches go either to the visceral plexuses or directly to the organs. As part of the spinal nerves, postganglionic autonomic fibers are directed to the vessels and glands of the skin, to skeletal muscles, and as part of the autonomic nerves, directly to the glands of the skin or blood vessels, ending mainly on their smooth muscle cells. Postganglionic fibers go to the innervated organs in three ways: as part of the spinal nerves, into which they enter along the gray connecting branches, along the blood vessels, or as separate nerves extending from the sympathetic trunk.
The sympathetic nerve plexuses are located on the abdominal aorta, on the anterior surface of the sacrum and consist of groups of nerve nodes,
nerves approaching them and departing from them. Among the largest plexuses is the celiac (solar) plexus, located around the celiac trunk. Sympathetic fibers depart from the nodes of this plexus, innervating almost all organs of the abdominal cavity. Due to its important role in the innervation of internal organs, this plexus was even called the brain of the abdominal cavity. Sympathetic fibers extending from the sympathetic trunk also form part of all spinal and cranial nerves. There are also independent sympathetic nerves - cardiac, carotid, esophageal, pulmonary and others, which carry out sympathetic innervation of the heart, organs of the head, neck, chest and abdominal cavities. The sympathetic nervous system innervates all tissues and all organs of the human body. The mediator (chemical mediator of excitation transmission) of the endings of sympathetic nerve fibers is norepinephrine. Under its influence, the rhythm and strength of heart contractions increases, vasoconstriction occurs, the pupil dilates, the secretion of gastric and intestinal glands decreases, intestinal smooth muscles relax, and salivation increases.
Parasympathetic part of the ANS
As noted above, in the parasympathetic part of the autonomic nervous system there are two main foci for the exit of parasympathetic nerve fibers from the central nervous system: cranial
(in the area of the brain stem) and
pelvic
(in the area of the sacral spinal cord).
The cranial part includes the parasympathetic nuclei located in the midbrain
(mesencephalic part), as well as in the area
of the pons and medulla oblongata
(bulbar part).
Parasympathetic ganglia, unlike sympathetic ones, are located in close proximity to innervated organs or in these organs themselves, which is why they are called terminal or terminal ganglia
.
In the cranial part of the parasympathetic nervous system there are: ciliary, pterygopalatine, submandibular, sublingual and auricular nodes (Fig.).
The ciliary node is located in the orbit and is connected by connecting branches to the optic nerve (I branch of the trigeminal nerve). Preganglionic fibers come to it from the accessory nucleus (Yakubovich's nucleus) of the oculomotor nerve (III pair). As part of the oculomotor nerve, parasympathetic preganglionic fibers reach the ciliary ganglion, where they switch to efferent neurons. The postganglionic fibers of these neurons, as part of the ciliary nerves, go to the muscle that constricts the pupil and the ciliary muscle, which tunes the eye to examine nearby or distant objects.
The pterygopalatine ganglion is located in the fossa of the same name and is closely connected by connecting branches with the maxillary nerve (II branch of the trigeminal nerve). However, preganglionic fibers are sent to it as part of the facial nerve (VII pair); they originate from neurons of the superior salivary nucleus
located in the bridge tire.
Having separated from the facial nerve in the form of the greater petrosal nerve
, part of the preganglionic parasympathetic fibers continues to the pterygopalatine ganglion, where synaptic contacts with its neurons are formed. Postganglionic parasympathetic fibers emerge from the pterygopalatine ganglion, join the maxillary nerve and are sent to innervate the glands of the mucous membrane of the nasal cavity, palate and pharynx.
Another part of the preganglionic parasympathetic fibers is separated from the facial nerve as part of a branch called the chorda tympani
, which joins one of the branches of the trigeminal nerve (
lingual
nerve), which continues to the submandibular and hypoglossal nodes. In these nodes, located near the glands of the same name, there are ganglion neurons, the fibers of which, as part of the glandular branches, go to the submandibular and sublingual salivary glands.
Rice. The structure and areas of innervation of the parasympathetic part of the autonomic nervous system. Roman numerals indicate cranial nerves
The ear node is located in the area of the outer base of the skull near the foramen ovale. Preganglionic fibers enter it from the inferior salivary nucleus
as part of the glossopharyngeal nerve (IX pair).
Preganglionic parasympathetic fibers are separated from the glossopharyngeal nerve as the tympanic nerve
, penetrating into the tympanic cavity of the middle ear, where they form a plexus.
Next, the fibers of the plexus in the form of the lesser petrosal nerve
reach the ear ganglion and end on its neurons.
Postganglionic fibers from the ear ganglion are directed to the parotid gland as part of the auriculotemporal nerve
(III branch of the trigeminal nerve).
The vagus nerve (nervus vagus) is the main collector of the parasympathetic nerve pathways. The parasympathetic fibers in its composition begin from the dorsal nucleus of the vagus nerve, located in the medulla oblongata. A distinctive feature of this nerve is the presence of clusters of nerve cells inside its trunk almost throughout its entire length. These nerve cells serve as the site for the switching of preganglionic fibers to postganglionic fibers. Part of the preganglionic nerve fibers as part of the nerve branches reaches numerous terminal nodes located in the area of periorgan or intraorgan (intramural)
visceral plexuses of the organs of the thoracic and abdominal cavities of the body. Postganglionic fibers of the neurons of the parasympathetic nodes, in which the fibers of the vagus nerve switch, innervate the thyroid gland, heart, lungs, esophagus, organs of the gastrointestinal tract to the left flexure of the colon, liver, pancreas, spleen, kidneys. Special small branches extend to all these organs.
The pelvic part of the parasympathetic nervous system consists of the pelvic nodes, scattered throughout the visceral plexuses of the pelvic region. Preganglionic fibers originate from the sacral parasympathetic nuclei located at the level of the II-IV sacral segments of the spinal cord, emerge from them as part of the anterior roots of the sacral spinal nerves, and then branch from them in the form of the pelvic splanchnic nerves. These nerves form the genital and pelvic plexuses. Preganglionic parasympathetic fibers switch in the parasympathetic ganglia of these plexuses, after which postganglionic parasympathetic fibers innervate the internal genital organs, bladder, urethra, as well as the muscles and glands of the terminal part of the colon after the left flexure, including the rectum.
The parasympathetic part innervates only the internal organs, which thus have double autonomic innervation - both sympathetic and parasympathetic. All other organs and tissues receive only sympathetic autonomic innervation. The parasympathetic part of the nervous system innervates non-organs and tissues. Most of the blood vessels, the uterus, the adrenal medulla, the pituitary gland, skeletal muscles, and receptors are deprived of this innervation.
The mediator produced at the endings of parasympathetic nerve fibers is acetylcholine
. This chemical mediator reduces the rhythm and force of heart contractions, narrows the lumen of the bronchi, enhances pulmonary ventilation, enhances gastrointestinal peristalsis, activates the secretion of the glands of the stomach, intestines, pancreas, and constricts the pupil.
Thus, unlike other organs and parts of the body, internal organs receive double autonomic innervation: both sympathetic and parasympathetic. Both of these parts of the autonomic nervous system act on the same internal organs, not opposing, but creating a more optimal mode of their operation. Depending on life circumstances and the magnitude of functional loads, the autonomic nervous system either strengthens the functions of certain internal organs, including the work of the heart, or weakens them. Moreover, at each moment, in accordance with the needs of the body, either the sympathetic or parasympathetic parts of the autonomic nervous system show greater activity in relation to the internal organs.
As for other organs and tissues (musculoskeletal system, skin with their structural elements, vascular walls and some others), all metabolic processes in them are regulated by the sympathetic part of the autonomic nervous system.
The work of all parts of the autonomic nervous system is coordinated by the hypothalamus of the diencephalon and the cerebral cortex.
The table provides a comparative description of the effects of sympathetic and parasympathetic nerves on organ functions.
Table
Comparative characteristics of the influences of sympathetic and parasympathetic nerves on organ functions.
| Organ | Nervous system | |
| sympathetic | parasympathetic | |
| Pupil | Expands | Narrows |
| Glands (except sweat glands) | Reduces secretion | Enhances secretion |
| Sweat glands | Enhances secretion | Not innervated |
| Heart | Increases heart rate and speeds up | Reduces and weakens heartbeat |
| Non-striated muscles of internal organs (bronchi, gastrointestinal tract, bladder) | Relaxes | Reduces |
| Vessels (except coronary) | Narrows | Not innervated |
| Coronary vessels | Expands | Narrows |
| Sphincters | Enhances tone | Relaxes |
Development in embryogenesis
- Development of the peripheral (somatic) and autonomic nervous system.
The peripheral (somatic) and autonomic nervous system develops from the outer germ layer - the ectoderm. Cranial and spinal nerves in the fetus are formed very early (5-6 weeks). Myelination of nerve fibers occurs later (for the vestibular nerve - 4 months; for most nerves - at 6-7 months).
Spinal and peripheral autonomic ganglia are formed simultaneously with the development of the spinal cord. The starting material for them is the cellular elements of the ganglion plate, its neuroblasts and glioblasts, from which the cellular elements of the spinal ganglia are formed. Some of them are shifted to the periphery to the localization of the autonomic nerve ganglia
| This section of the article has not been written. According to the plan of one or more Wikipedia contributors, a special section should be located in this place. You can help by writing this section. This mark was set on October 31, 2021 . |
Autonomic nervous system
All functions of the body are divided into somatic (animal) and vegetative (autonomous). Somatic functions include the perception of external stimuli and motor reactions of skeletal muscles. These reactions can be voluntarily evoked, enhanced or inhibited and are under the control of consciousness. Vegetative functions ensure metabolism, thermoregulation, the functioning of the cardiovascular, respiratory, digestive, excretory and other systems, growth and reproduction. Autonomic reactions, as a rule, are not controlled by consciousness.
The autonomic nervous system (ANS) is a complex of central and peripheral nervous structures that regulate the activity of internal organs and the necessary functional level of all body systems. More than 80% of diseases are associated with a disorder of this system.
Physiological significance:
1. Maintaining homeostasis - the constancy of the internal environment of the body.
2. Participation in the vegetative support of various forms of mental and physical activity.
Morphological and functional features of the ANS.
General properties of the somatic and autonomic nervous system.
1. Reflex arcs are built according to the same plan - they have afferent, central and efferent links.
2. The reflex arc of somatic and autonomic reflexes may have a common afferent link.
1 - receptor
2 - afferent nerve and afferent neuron
3 - interneuron in the spinal cord
4 - efferent nerve, which leaves the efferent neuron
5 - effector organ
The structure of the reflex arc of somatic and autonomic reflexes
Structure of the ANS.
The ANS consists of central and peripheral sections.
The central section is represented by segmental and suprasegmental centers. Segmental centers are the spinal cord, medulla oblongata and midbrain. Suprasegmental centers - hypothalamus, cerebellum, basal ganglia, cerebral cortex, limbic system. Suprasegmental centers exert their influence only through underlying segmental centers.
The peripheral section includes microganglia of the metasympathetic nervous system, para- and prevertebral ganglia, preganglionic and postganglionic fibers of the ANS.
Central nervous control of autonomic activity
The activity of the autonomic nervous system varies depending on the information it receives from visceral and somatic afferent fibers. Regulation also depends on information coming from higher centers of the brain, in particular from the hypothalamus.
Internal organs are innervated by afferent fibers that respond to mechanical and chemical stimuli. Some visceral afferent fibers reach the spinal cord through the dorsal roots along with somatic afferents. These fibers form synapses at the segmental level and transmit information through second-order ascending fibers within the spinothalamic tract of the spinal cord. They project to the nuclei of the solitary tract, various motor nuclei in the brain stem, the thalamus and hypothalamus. Other visceral afferents, such as those from arterial baroreceptors, reach the brainstem via vagal afferents.
Information from visceral afferents causes certain visceral reflexes, which, like reflexes of the somatic motor system, can be either segmental or can be associated with the participation of neurons in the brain. Examples of autonomic reflexes are the baroreceptor reflex, pulmonary respiratory reflexes, and the micturition reflex.
In response to perceived danger and damage, there is a behavioral warning response that can lead to aggressive or defensive behavior. This is known as the defense response, which originates in the hypothalamus. During a defensive reaction, there are noticeable changes in the activity of the autonomic nerves, in which the normal control of reflexes is altered.
The hypothalamus regulates the homeostatic activity of the autonomic nervous system and is the highest central organ for the regulation of the sympathetic and parasympathetic systems. The activity of the autonomic nervous system and the functions of the endocrine system are under the control of the hypothalamus, which is part of the brain and regulates mainly those
functions that are associated with maintaining homeostasis of the body. If the hypothalamus is destroyed, homeostatic mechanisms do not work. The hypothalamus receives afferents from the retina, sensory organs, somatic organs, and afferents from internal organs. It also receives a lot of information from other parts of the brain, including the limbic system and cerebral cortex, which can influence the functioning of the autonomic nervous system indirectly through changes in the functioning of the hypothalamus. Neurons of the hypothalamus play an important role in thermoregulation, in the regulation of tissue osmolarity and water-salt balance, in the control of food and drink intake, and in reproductive activity.