Electroencephalography allows you to change the bioelectrical activity of nerve cells in the brain and record painful transformations caused by the appearance of foci of epileptic activity in the head. Today, EEG is the only effective way to accurately determine the state of neurons. Below is information about what an EEG shows in epilepsy.
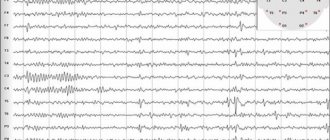
The exact signs of the disease are discharges and patterns of attack. The disorder is characterized by high-amplitude outbursts with varying activity. By themselves, they are not evidence of the development of epilepsy and are determined in the context of the clinical picture.
In addition to diagnosing epilepsy, EEG plays a significant role in identifying the form of the disease. This determines the prognosis for the development of the disorder and the choice of appropriate medications. EEG makes it possible to determine the required amount of drugs to assess the decrease in epileptic activity and to provide for side effects due to the occurrence of additional pathological activity.
To determine epileptoform activity on the EEG, rhythmic light stimulation, hyperventilation and other methods of influence are used, taking into account information about the factors that provoke seizures. Long-term recording during sleep allows the identification of epileptoform impulses and patterns related to seizures. The diagnosis is determined by the characteristic bioelectrical activity of neurons.
What is EEG: the essence of the method
An EEG or electroencephalogram is an effective diagnostic method for patients with signs of epilepsy and other various brain injuries. This method is often prescribed to patients who do not need it at all.
The essence of the technique is that it records electrical signals sent by neurons - nerve cells of the brain. In fact, many pathologies are manifested by severe disturbances in the electrical activity of the brain. Most often this is epilepsy, during which a group of neurons exhibits serious activity, and structural changes in the brain are detected: tumors, cysts, consequences of stroke and hemorrhages.
This technique is considered to be as accurate as possible, and all because it can fully show the entire clinical picture of the disease:
- how far the inflammation has spread and its level;
- what changes have occurred in the vessels;
- early signs of epilepsy;
- neoplasms and stages of their development;
- how much brain function is impaired due to an illness affecting the nervous system;
- what are the consequences of a stroke, hemorrhage or surgery.
According to ICD-10, epilepsy is assigned code G40; a detailed description of the EEG for this pathology allows you to track what changes have occurred in the brain, especially if this study was not carried out for the first time. Thus, the doctor has the opportunity to monitor brain activity during treatment and adjust it at any time. Almost always, after diagnosis, the doctor can accurately determine where exactly the source of excitation is localized.
Features of diagnosing chronic epilepsy using magnetic tomography
The peculiarities of diagnosing epilepsy using MRI are that the identified pathological formation of the brain itself cannot accurately indicate the presence of epilepsy, just as the absence of macrostructural pathology on MRI in standard mode cannot exclude the disease, since the cause of the disease may be microstructural brain changes.
Diagnosing chronic epilepsy (for a long time, starting in early childhood) and searching for a source of excitability is very difficult. The cause of the disease in children is congenital pathology of the cerebral cortex or past infectious diseases.
Difficulties in diagnosing microstructural pathology are due to the fact that identifying a focus of increased excitability in this case requires the use of special contrast and study modes (MP-RAGE, VIBE, FLAIR), which are not used in standard brain examinations.
For targeted diagnosis of the source of excitability, it is necessary to carry out thinner sections (two to three millimeters) and high power of the device.
As a rule, an MRI study is prescribed to a patient with chronic epilepsy purposefully to identify the focus of excitability. This is often necessary in cases of forms of the disease that are resistant to drug therapy, in order to resolve the issue of surgical treatment.
To increase the effectiveness of MRI, before it is performed, the patient undergoes electroencephalography, which is a clue to the radiologist in which part of the brain to look for the suspected lesion.
When should an EEG be performed?
This diagnostic method is used for various speech, mental and neurological disorders. As a preventive measure, EEG can be prescribed to people who are taking a driver's license exam, as well as to obtain permission to store and carry weapons. Positive results can exclude the presence of schizophrenia and other mental disorders. EEG shows epilepsy, and also provides other data, so this technique is used for medicinal purposes:
- after surgery that could affect the functioning of brain cells;
- when identifying and determining the location of tumor and cystic formations;
- with traumatic brain injuries obtained in various ways;
- to confirm or deny the presence of epilepsy;
- if the patient experiences convulsions, numbness of the limbs and fainting;
- with chronic hypertension and circadian rhythm disturbances;
- if the child has developmental delay.
An EEG of the brain can reveal not only disturbances in the functioning of brain tissue, but also the severity and depth of their damage, and the location of the source of the disease. In some cases, regular monitoring may be recommended, in other words, several studies at short intervals, which will help not only to identify signs of epilepsy on the EEG, but also to determine further treatment, which can be adjusted.
By studying the processes of activity of the nervous system, it is possible to prevent another attack. For patients in a coma or under long-term general anesthesia, this type of diagnosis is mandatory, because it will help determine the performance and vital activity of brain tissue.
Differential diagnosis of seizure
To clearly determine the presence of epilepsy, it is important to know its symptoms.
Signs of the disease:
- passing disorder of consciousness;
- significant changes in the emotional and mental sphere;
- convulsive syndrome;
- paroxysmal disturbances in the functioning of internal organs.
According to the classification developed and approved in 1989, there are only three types of seizures.
They are:
- Symptomatic – manifested due to brain damage or other serious pathology.
- Idiopathic - any syndrome caused by a hereditary predisposition.
- Cryptogenic – not detected during diagnostics.
But there are also a lot of other (non-epileptic) seizures that must be strictly differentiated. These include neurogenic, somatogenic and psychogenic.
Epileptic seizures can be major or minor. The first one is expressed very clearly and has several stages of development. Within 1-3 days, the patient develops a feeling of anxiety, aggression or depression is possible.
The attack itself begins with a fall, severe convulsions, screaming, foaming and respiratory arrest. It lasts about 5-7 minutes, and then gradually subsides.
The second (minor) is characterized by the absence of prolonged loss of consciousness. The person remains standing, but suddenly freezes in place for a few seconds, throwing his head back. This state quickly passes, and the person continues his activities.
Differential diagnosis of epilepsy:
Value of the study
Epilepsy code according to ICD-10 G40, EEG in this disease helps to identify and record foci of neuronal activity. The main aspects of the application of this technique are:
- determination of the form of the disease;
- opportunities to track development dynamics;
- monitor improvements in the patient's condition;
- selection of the correct therapy and dosage of drugs.
The main value of diagnosis is that all pathological changes can be detected between seizures.
If anomalies are present, then the equipment records peaks and waves, as well as graph elements specific to its definition. Therefore, as soon as bursts of activity, peaks and waves appear on the EEG, this already indicates the presence of a pathological condition, but this is not enough for an accurate diagnosis. Similar changes are often observed in cases of malignant neoplasm, after a stroke, sleep disorder, and encephalopathy. That is why additional studies are being carried out.
Each form of the disease has its own characteristic waves. With rolandic, their greater concentration is observed in the central temporal lobes, with nocturnal - in the frontal part.
The concept of “epileptic activity”
This term is used in two cases:
- Registration of epileptiform phenomena on the EEG during a seizure (psychomotor seizure pattern or ongoing polyspike). The activity may not contain epileptic seizure patterns.
- In the case of a clear activity schedule. Can be recorded outside of an attack .
Hereditary EEG patterns may be associated with epileptic seizures. Some specific combinations have different epileptic syndromes.
The presence of epileptiform activity and epileptic seizure patterns on the EEG, high-amplitude bursts of activity (more than 150 μV) are important signs of the presence of epilepsy.
EEG patterns
How to prepare for an EEG?
After 12 o'clock at night before the diagnosis, the patient should avoid drinking drinks containing caffeine. Hair should be washed and dried, and oils, lotions and aerosols should not be applied to it. There are no other requirements, but the child needs to be prepared more carefully to get the right results.
An epileptic attack in a child can begin at any moment and parents are not always prepared for it. Therefore, if even the slightest deviations are noticed, you need to seek help and undergo an examination. An EEG will help make an accurate diagnosis, but you should prepare for the study:
- Take a good look at the child's head. If wounds and scratches are found, they should be reported to the doctor. Electrodes should not be attached to damaged areas of the skin.
- Feed the baby. The study is carried out on a full stomach, this is the only way to get clear results. But you can’t give sweets with chocolate. Infants are fed before the procedure in a medical facility. In this case, the baby will fall asleep peacefully and sleep peacefully during the examination.
Stop taking medications, but if the child receives them on an ongoing basis, then doctors warn about this. Children of school and preschool age need to be explained what they will be doing; only the right psychological attitude will help to avoid excessive emotionality. The child can take toys with him, but not electronic ones.
Remove all foreign objects, such as elastic bands and hairpins, from the head; hair should be loose. If an EEG for epilepsy is not done for the first time, then be sure to take the previous transcript with you. If a child is sick, no diagnosis is carried out; a full recovery is expected.
Epilepsy, or a slightly different life
(Article by Elena Pilikina, AiF)
Neurologist, professor at the Moscow State Medical and Dental University, corresponding member of the Russian Academy of Medical Sciences, Doctor of Medical Sciences Vladimir Alekseevich KARLOV talks about this problem.
This disease bears the imprint of mysticism; epilepsy is often called “divine disease”, “sacred disease”, sometimes when talking about it they say the word “epileptic”. The sick were considered possessed by demons, evil spirits as punishment for sins. And only 400 BC. e. The outstanding ancient Greek philosopher and physician Hippocrates first introduced the term “epilepsy” (from “epileptos” - translated from Greek as “captured”) and associated it with brain disease. Neurologist, professor at the Moscow State Medical and Dental University, corresponding member of the Russian Academy of Medical Sciences, Doctor of Medical Sciences Vladimir Alekseevich KARLOV, who has been studying epilepsy since 1957, talks about this problem.
— Vladimir Alekseevich, it is known that epilepsy can manifest itself not only in childhood, but also in adulthood. What can cause the disease?
— Despite the fact that the disease most often debuts in childhood, genetic predisposition to it can play a fatal role at any time, usually under the influence of external unfavorable conditions. Other factors are well known: trauma, vascular diseases, brain tumors, etc.
— In the everyday understanding, an epileptic is a person who at any moment can go into convulsions, foaming at the mouth, bending in the most unexpected positions. How typical is this picture for a patient with epilepsy?
— The described picture is typical of a hysterical seizure, as it is now called - a demonstrative or pseudoepileptic seizure, which in form may even resemble a real epileptic attack, but most often it is not. Unfortunately, even among non-specialist doctors in this area, there is a misconception that epileptic seizures are convulsions, but this is not entirely true. There are many non-convulsive forms of epilepsy, especially in children, and only an electroencephalogram (EEG) of the brain can confirm the diagnosis. I am currently working on a book, “Epileptic Seizures in Children, Men and Women,” where this problem will be discussed in detail.
Neurologist or psychiatrist?
- The disease we are talking about is at the intersection of two medical specialties - neurology and psychiatry. Which doctor should care for the patient?
— Undoubtedly, the disease is neurological, because epilepsy is an organic disease of the brain. But the problem itself is interdisciplinary, that is, it is neurological, psychiatric, neurosurgical, pediatric and neurophysiological. It must be said that many people with epilepsy are undoubtedly very bright personalities, but one should not take comfort in the fact that Dostoevsky and other great people had a similar disease. The diagnosis of epilepsy is a tragedy for the patient, often a disaster, as a number of serious professional problems arise.
— And yet, what kind of specialist should take care of a patient with epilepsy?
- There is only one answer - a neurologist. It’s good that the stupidity that existed until recently and obligated a person with such a disease to register with a psychoneurological dispensary has ended. Although, of course, if the patient has predominant mental disorders, then he is a patient of a psychiatrist.
“But in some convulsive forms of the disease, when a person makes chaotic movements, loses consciousness and can fall and hit himself, he becomes dangerous both for himself and for others.
- This is a little exaggerated. There is an opinion that patients with epilepsy are very dangerous because they cannot control their actions during an attack. In reality, such cases are rare. We are talking about completely mentally retarded patients with epilepsy, and the progression of the underlying disease may be decisive. Rather, patients with epilepsy are characterized by excessive accuracy (pedantry), thoroughness of actions, polarity of moods (a very rapid transition from delight to depression). It is also characteristic that the usual good qualities of a person are exaggerated and develop into other forms. For example, affectionateness can become intrusiveness, flattery, and servility. But once again I want to say that such changes are extremely rare and are more typical for chronic, treatment-resistant patients. Famous people with this disease are bright personalities who have left a noticeable mark on the history of mankind.
— Among the methods of treating epilepsy, a special diet has recently been often mentioned. What can you say about this?
— The diet was developed back in the 20s, it was abandoned several times and returned to it again. The bottom line is that a high-fat diet is sometimes really effective for certain forms of epilepsy, mainly in children. The difficulty is that it is difficult to tolerate, you need to select products so that the body has ketosis (a certain change in metabolism), and for this the patient must be treated by a whole group of highly qualified specialists (dietitian, psychologist, neurologist and nurse). Such a team of 6-7 people carefully prepares the patient for the transition to a very specific diet, guides him during treatment, and upon discharge home, the patient is given specific recommendations on nutrition and monitoring the level of acidosis (ketosis) using a test strip that changes color upon contact with the patient's urine. In our conditions, this has not yet been worked out due to the complexity of organizing such treatment.
Spoons away
- But seizures are not only non-convulsive. What to do if a seizure occurs before your eyes, during which a person loses consciousness, falls, may suffocate, or get hurt? What can be done to help him?
- There is no need to be scared here. The first thing is to see if there is anything in the mouth that can cause respiratory arrest (removable dentures, etc.), this must be removed immediately. The patient should be placed on his side so that he does not choke on saliva or have a sunken tongue. Usually they try to put a spoon in the patient’s mouth, but this is not necessary, because the teeth break on something hard. It is best to roll up a soft cloth and insert it into your mouth; it will prevent you from biting your tongue.
— Tell us about the treatment methods that today help patients with epilepsy.
- First of all, you need to follow the regime. Avoid alcohol completely. In some forms of the disease, it is absolutely impossible to get enough sleep, although too much sleep can also be harmful. As for direct treatment, there are two approaches - medicinal and surgical. Today neurosurgery offers several types of operations. So, in case of temporal lobe epilepsy, a part of the temporal lobe is resected (removed), and it turned out that with unilateral removal, the second hemisphere of the brain takes over everything, that is, it compensates for the loss. For bilateral lesions, removal is performed in one lobe, and in the second, for example, spot electrolysis is performed, precisely plunging the needle into the affected area and coagulating (destroying) the affected tissue. In the temporal lobe, the location of epileptic foci is associated with parts of the brain that are responsible for memory, emotions and, of course, vital, that is, special care must be taken during treatment.
Medicines are used very widely today. Previously, doctors believed that the main thing was to eliminate the seizure and then the problem would disappear by itself, which is why patients were given Luminal (there were no other drugs then) in huge doses. Yes, seizures were eliminated in many cases, but after such treatment, not all patients could work, because their reaction speed and thinking slowed down, and in some professions these are necessary conditions. Later, psychotropic drugs appeared to correct mood. Today there is a completely different approach to the problem, the main thing is the quality of life. The “price” of medications should not be exorbitant, and one should not strive to eliminate the seizure at any cost. Often it is necessary to get rid of only convulsive seizures, and the patient sometimes copes with non-convulsive seizures himself. The quality of life is mainly affected not by the frequency of seizures, but by their nature. For the patient, it is the convulsive forms of paroxysms that are scary, they are unpredictable, and make a terrible impression on others. In addition, a person can fall, hit himself, get burned, etc. And those around him often mistake a “small” seizure for fainting - “well, it doesn’t happen to anyone.” Epilepsy must be treated correctly, and there is no life sentence in this diagnosis.
Dangerous sun
— After an incident in Japan, when showing a cartoon with rapidly flashing frames caused massive epileptic seizures in children, they started talking about photosensitive epilepsy.
- This is a similar problem. It seems to me that it is more correct to talk about stimulus-sensitive epilepsy, in which attacks occur in response to certain, and not only external, stimuli. For example, an attack can be caused by playing chess, cards, etc. Photosensitive epilepsy is the most striking example of reflex epilepsy, that is, stimulus-sensitive. One of the patients, a 20-year-old girl, felt her first attack after traveling on a train. She looked out the window, and the bright sun flashed through the foliage of the trees, and this is what stimulated the attack. In practice, when recording brain biocurrents (EEG), rhythmic light stimulation is mandatory, since light flickers of a certain frequency can cause an epileptic attack.
— A natural question is about light at discos, about laser beams, lighting techniques for theatrical events (New Year trees, children's matinees, etc.).
- If the diagnosis has already been made, then it is better to avoid such entertainment. But parents should be alarmed, for example, by the fact that the child often blinks involuntarily, because this may not be pampering, but “small” seizures. There is no need to be scared, you just need to urgently consult a doctor, since such forms have a benign (favorable) prognosis. With this form, the patient must avoid bright sun, walk on the shady side of the street, etc., and by these actions avoid attacks. Adults need to pay attention to computer games - flickering displays are also not helpful.
— And with these forms there is also no pain or suffering?
— This is actually a very interesting story, because most often patients do not remember anything, but there are also cases of self-inducing attacks. One of the patients, a doctor by profession who could objectively describe her feelings, said that on a bright, sunny day she had an irresistible desire to “meet the sun.” She interrupted the reception and went into the next room, where, with the help of her palm moving in front of her face, she reproduced the flickering of the sun's glare. This caused a non-convulsive attack of epilepsy, after which the tension immediately subsided, a collapse, a reset, occurred, the general condition returned to normal and the person could work calmly. The seizure also has a relieving value. I believe that this mobilizes reserves in the body that normally cannot be used.
— Vladimir Alekseevich, explain another unusual story, more like a myth. This concerns an absolutely incredible case when a patient with epilepsy during a seizure managed to buy a ticket and fly to another city, where he woke up, remembering absolutely nothing. But unlike the hero of “The Irony of Fate...” he was completely sober. Is this plausible?
— The story you told is completely real. A little clarification is necessary here, since in the new classification seizures are quite correctly divided into two groups. The first is self-limiting, when the seizure ends quickly, and the second is ongoing seizures, when they follow one after another and the patient, not yet having time to recover from one, is already “overwhelmed” by the next one. During prolonged nonconvulsive seizures, sometimes the patient subconsciously “holds” the program and implements it, as in your example. He automatically performs his usual actions, and then remembers absolutely nothing, because he was in the status (state) of a seizure for hours and even days.
Features of diagnostics
An EEG of the brain is a painless procedure that will not harm either an adult or a child. During diagnosis, the patient sits comfortably in a chair, electrodes are placed on his head, but initially measurements are taken in three positions: head circumference, the distance between the bridge of the nose and the protrusion of the occipital bone, from one ear to the other through the crown. Only after this can you determine exactly where to attach the electrodes. The attachment point is degreased with alcohol, after which a gel is applied and the sensor is installed. In some cases, special helmets or caps may be used.
What does an EEG look like for epilepsy? Yes, in different ways, even in a healthy person you can sometimes detect waves and peaks of activity, which is mainly due to his individual characteristics.
In children who suffer from neuroses and psychopathy, as well as those with an aggressive character, the study reveals activity, but there are no clinical signs. But most young patients with such data are eventually diagnosed with epilepsy.
With widespread seizures, activity is observed in all areas, and when it is a focal form, then only in certain areas. It is not always possible to detect signs of illness in people who abuse alcohol. The following may cause activity in such patients: eye movement, swallowing, touching sensors, contraction of head muscles, heartbeat, pulsation of blood vessels.
The patient's age, taking pills for epilepsy or other diseases, time of the last seizure, visual impairment, abnormal shape of the skull - all this can affect the EEG results. Therefore, the study is carried out taking into account all related factors.
How long does the study take?
A routine examination is a routine EEG or diagnosis of a paroxysmal state. The duration of the study depends on which area is being tested and what functional tests are used. On average, the procedure takes about half an hour. During this time, the specialist manages to:
- perform rhythmic photostimulation using different frequencies;
- check for hyperventilation;
- carry out a load in the form of blinking;
- detect hidden changes.
If the data obtained is not enough, then in addition to the EEG for epilepsy, the specialist can use a more in-depth and effective examination:
- EEG of night sleep.
- EEG with deprivation.
- Long-term EEG.
The duration of these techniques can take from 20 minutes to 15 hours.
EEG rhythms
During an EGG, the device detects four main types of rhythms:
- Alpha waves are the main element in the diagnosis of a healthy adult patient and are recorded in 90% of people. These waves have a frequency of around 13 hertz per second and are fundamental during wakefulness, when the patient simply lies with his eyes closed. The maximum activity of alpha waves is observed in the area of the back of the head and crown.
- Beta, like alpha waves, are considered normal manifestations in the body of a healthy adult. But the number of their oscillations reaches 35 hertz per second, they are recorded mainly over the frontal part. The beta rhythm appears if the sensory organs are irritated: by touching the patient, when stimulated by light or sound.
- Delta waves with a frequency of up to 3 hertz during decoding of an EEG for epilepsy can mean normal in a baby up to one year old. The indicator partially persists for up to 7 years. In adults, they are recorded during sleep.
- The theta rhythm with a frequency of up to 7 oscillations per second is normally found in children from one to 6 years of age, gradually being replaced by alpha waves as they grow older. In adults they are observed during sleep.
Analysis transcript
Before answering the question of what to do with epilepsy, you need to accurately decipher the EEG data. Research data is displayed on a monitor or on paper in the form of graphic curves that only an experienced specialist can decipher. The analysis and conclusion of an EEG for epilepsy is issued by a neurophysiologist, who, when decoding, takes into account the patient’s age, his complaints, the clinical picture of disorders in the body and many other factors, such as heredity.
Key points of decoding:
- It is determined which of the rhythms is the main one, predominant in the patient.
- The symmetry of the electrical potentials of nerve cells, which are recorded from the left and right hemispheres of the brain, is carefully studied.
- Pathological changes, such as delta and theta waves in an adult patient while awake, are carefully analyzed.
- The regularity and amplitude of the rhythms are checked.
- Paroxysmal activity is revealed when sharp waves, peaks and sky-waves are detected on the curve.
- If there are no pathological changes in the background EEG, then additional functional tests are performed, such as hyperventilation or photostimulation, repeated recording of electrical potentials and decoding.
History taking and examination
When collecting anamnesis, the following must be taken into account:
- patient complaints (it is necessary to find out the frequency and duration of attacks, whether an aura is noted before the attack, how the attack proceeds: with or without loss of consciousness, whether the patient remembers about the attack or friends and relatives tell him about it, the presence of epilepsy in close relatives);
- the age of the patient at which the epileptic attack was first recorded;
- the patient’s condition in the post-attack period (the presence of hallucinations, memories of the attack, the degree of fog of the patient’s consciousness after the attack);
- the presence of traumatic brain injuries, intoxications, neuroinfections, cerebrovascular accidents, episodes of drug use or alcohol abuse;
- data on intrauterine infections or intrauterine development disorders, congenital malformations;
- disturbances in sleep and rest patterns, the presence of concomitant diseases that could provoke an attack;
- the patient's use of drugs that could provoke an attack.
What changes are observed on the EEG in epilepsy?
During an epileptic seizure, EEG recording allows recording high-amplitude activity in the form of peaks and sharp waves. Outside of an attack, convulsive activity in the brain may not manifest itself in any way, therefore, to provoke epileptic activity, various tests are used. Patients often experience paroxysmal activity in the form of high-voltage theta and delta waves. For long-term EEG recording, it is allowed to use video monitoring, when the study is carried out over a long period of time, in some cases up to 8 hours, and subsequently a specialist deciphers it.
EEG allows not only to determine the location of the source of the disease, but also to recognize its type. If, nevertheless, the diagnosis is confirmed and bright and unlike anything else changes can be seen on the graph, then the description of the EEG for epilepsy will contain the following information:
- waves with sharp angles, rising and falling sharply;
- pronounced slow waves with sharp angles;
- a sharp increase in amplitude by several units;
- during testing for hyperventilation, narrowing and severe spasm of blood vessels appears;
- During photostimulation, an unusual reaction to the test is observed.
If there is a suspicion that this is indeed epilepsy, then during the control study the tests are carried out in a gentle mode, and all because the load can cause another epileptic attack in the patient.
When the diagnosis is definitely established, many people wonder what to do with epilepsy, how to help such a patient.
3.8. Epilepsy of the occipital lobe
general characteristics
Occipital epilepsy is a locally caused form of epilepsy, characterized predominantly by simple partial paroxysms not accompanied by impaired consciousness.
Early clinical symptoms of occipital epilepsies are caused by epileptic activity in the occipital lobe, and late ones are caused by the spread of epileptic activity to other areas of the brain.
The initial clinical symptoms of occipital paroxysms include: simple visual hallucinations, paroxysmal amaurosis and visual field disturbances, subjective sensations in the area of the eyeballs, blinking, deviation of the head and eyes to the side contralateral to the epileptic focus.
Simple visual hallucinations are represented by bright flashes of light before the eyes, glowing spots, circles, stars, squares, straight or zigzag lines, which can be single or multi-colored, stationary or moving in the field of vision.
Paroxysmal amaurosis manifests itself in the form of blurred or temporary loss of vision, feeling like “blackness before the eyes” or “a white veil before the eyes.”
Paroxysmal visual field disturbances manifest as paroxysmal hemianopsia or quadrant hemianopia within seconds or minutes.
Subjective sensations in the area of the eyeballs are expressed primarily by a feeling of eye movement in the absence of objective symptoms.
Blinking is observed at the very beginning of the attack, is of a violent nature and resembles the fluttering of a butterfly's wings.
Electroencephalographic patterns
Interictal EEG may not show pathological patterns or may be represented by epileptiform activity in the occipital or posterior temporal region, sometimes bilaterally. The main activity may not be changed or there may be disorganization and slowness. Epileptiform activity can often also be falsely represented in the temporal lobe of the same name (
)
During an attack, epileptiform activity may spread with the appearance of “mirror” discharges.
What other diagnoses does EEG reveal?
After undergoing an examination, neurologists often diagnose children and adults not only with epilepsy, but also with other ailments. Among the common diseases are the following:
- neoplasm in the brain of various etiologies, the cause of which is not clear;
- traumatic brain injury;
- an inflammatory process that simultaneously affects the membranes of the brain and the medulla; the cause of this condition can be an infection;
- abnormal accumulation of fluid in the structures of the brain, often this pathology is congenital, perhaps the pregnant woman did not undergo mandatory screenings, or this disease developed as a result of an injury that the baby received during childbirth;
- a chronic disease that affects the mental and nervous state with characteristic attacks - epilepsy, provoking factors can be heredity, birth injuries, infections, improper behavior of the mother during pregnancy;
- hemorrhage in the brain due to rupture of blood vessels, a condition that can be provoked by high blood pressure, head injuries, blockage of blood vessels with cholesterol plaques;
- cerebral palsy;
- sleepwalking, somnambulism.
Many diseases can be detected, therefore, if suddenly the EEG does not show epilepsy, but there are seizures, the doctor prescribes other types of studies. This is the only way to exclude other pathologies and make a more accurate diagnosis.
How accurate is imaging for epilepsy?
Single epileptic-like seizures may occur in 10% of the population, while true epilepsy is a chronic disease characterized by recurrent seizures that may occur in 2% of the population.
Current neuroimaging techniques are useful in diagnosing abnormalities underlying epilepsy. Information obtained from imaging techniques may also contribute to the correct classification of specific types of epileptic disorders and may delineate the underlying genetics of some syndromes.
Neuroimaging is even more important for those patients who have medically unexplained seizures. Advances in technology for localizing focal epileptogenic substrates, especially high-resolution structural images obtained after magnetic resonance imaging, have significantly improved the success of surgical treatment. This review compares available imaging modalities and the practical application of brain imaging in the treatment of patients with epilepsy.