Indications for use
According to the instructions for Diphenin, the drug is intended for the treatment of:
- Grand mal seizures;
- Status epilepticus, accompanied by tonic-clonic seizures;
- Myotonia, including congenital;
- Epileptic seizures in neurosurgery;
- Episodic behavioral disorders (anger, irritability, insomnia, anxiety, hyperexcitability);
- Paroxysmal choreoathetosis;
- Ventricular arrhythmias, including those caused by intoxication with tricyclic antidepressants and cardiac glycosides;
- Rhythm disturbances associated with organic damage to the central nervous system;
- Congenital long QT syndrome (with ineffectiveness of beta-blockers);
- Trigeminal neuralgia (in combination with carbamazepine or as a second-line agent).
Difenin is also prescribed for the prevention of:
- Post-neurosurgical and post-traumatic epilepsy;
- Ventricular arrhythmias after heart surgery.
Medicinal properties
If you have epilepsy and increased convulsive readiness, it is important to be able to block seizures in a timely manner, since the frequency and intensity of seizures negatively affect the centers of the brain and significantly reduce brain activity. The patient’s quality of life deteriorates significantly with each attack, and the recovery process is usually long and complex. Therefore, it is advisable to stop a convulsive attack in time by choosing the right drug, taking into account the nature and course of the disease. One of the most common anticonvulsant drugs is the drug “Difenin”. Its advantages are that it selectively inhibits the motor centers of the brain, while restoring and maintaining the functions of the vestibular apparatus. This is how the anticonvulsant effect is achieved, maintaining normal brain activity for a long time.
Contraindications
The use of Difenin is contraindicated in:
- Hypersensitivity to phenytoin or any auxiliary component;
- Morgagni-Adams-Stokes syndrome;
- Sinus bradycardia;
- AV block II-III degrees;
- Sinoauricular block;
- Porphyria;
- Cachexia;
- Heart failure;
- Impaired liver/kidney function;
- Pregnancy;
- Breastfeeding.
The drug should be used with caution in patients suffering from alcoholism, diabetes mellitus, as well as hyperthermia and systemic lupus erythematosus.
The drug is contraindicated...
When prescribing Diphenin as a medicine, doctors usually take into account the presence of liver and kidney pathologies and heart failure. The drug is not prescribed for peptic ulcers of the stomach and duodenum. The use of the drug "Difenin" by pregnant women and, naturally, nursing mothers is strictly contraindicated. In some cases, drug analogues act sparingly; this helps doctors choose the right treatment, taking into account the existing concomitant diseases in the patient’s medical history. Patients suffering from exhaustion of the body due to diets and malnutrition are categorically not recommended to use Diphenin as a medicine, since it has the function of suppressing appetite. The drug should not be used to treat patients with vitamin D deficiency in the body, since taking Diphenin will lead to a worsening of the condition.
Directions for use and dosage
According to the instructions for Diphenin, the tablets should be taken after meals.
When prescribing the drug as an anticonvulsant and sedative, the initial single dose is 100-300 mg, the frequency of administration is 1-3 times a day. If necessary, it is gradually increased to the optimal maintenance dosage (usually 200-500 mg per day).
As an antiarrhythmic drug, Difenin is usually taken 1 tablet four times a day. The effect of the drug appears on approximately 3-5 days, after which the frequency of administration is reduced to 3 times. To quickly achieve the required therapeutic concentration of phenytoin, the following regimen of use of Difenin can be prescribed: 2 tablets 5 times during the first day, the next 2 days - 1 tablet 5 times, from the 4th day of treatment - 1 tablet. 2-3 times a day. With this use of the drug, the antiarrhythmic effect is usually achieved within 1-2 days of treatment.
For children, at the beginning of therapy, the medicine is prescribed at the rate of 5 mg per kilogram of weight. If necessary, the dose is increased, but not more than 300 mg per day. The maintenance dosage is 4-8 mg/kg.
Patients with renal failure require a dose reduction of Diphenin, sometimes by 50%.
Analogs
Complete analogues containing phenytoin include Difantoin. At the moment it is temporarily out of stock. Among anticonvulsants, carbamazepine-based drugs are very popular.
Unlike Difenin, it has an effect in epilepsy with minor seizures, and is used to eliminate pain syndrome of neurogenic etiology (post-traumatic pain, spinal cord tuberculosis, neuralgia of various localizations). Carbamazepine is prescribed for acute manic syndrome and depression. List of drugs with carbamazepine:
- Zeptol, Sun Pharmaceutical, India. Price 350-469 rubles per 100 tablets.
- Tegretol, Novartis Pharma, Italy. The cost of package No. 50 is 480-520 rubles.
- Finlepsin, Teva, Poland. The price of a pack of 50 tablets is 580-650 rubles.
Preparations based on valproic acid can be used for various forms of epilepsy, normalize sleep, and produce a sedative effect. A special feature of this group is the variety of release forms, which allows you to individually select a treatment regimen taking into account the characteristics of the body. Approved for use during pregnancy and newborns. Commonly prescribed medications include:
- Konvulex, G.L. Pharma GmbH/GL, Austria. Release forms: capsules of 150, 300 and 500 mg of sodium valproate, 100 ml syrup in a bottle at a dosage of 50 mg/ml, ampoules with a ready-made solution for injection 100 mg/ml, 5 ml each.
Convulex - Depaquin, Uniter Liquid (Client Sanofi Aventis), France. Available in the form of syrup, solution for injection, tablets with prolonged action.
Side effects
When using Diphenin, according to the instructions, the following side effects may occur:
- Confusion, ataxia, mood changes, nystagmus, muscle weakness, dizziness, incoordination, transient nervousness, hand tremors, sleep disturbances, stuttering or slurred speech, in some cases peripheral neuropathy;
- Nausea and/or vomiting, toxic hepatitis, constipation, liver damage, gum hyperplasia, starting with gingivitis;
- Granulocytopenia, leukopenia, agranulocytosis, megaloblastic anemia, thrombocytopenia, pancytopenia;
- Hypertrichosis, widening of the tip of the nose, thickening of the lips, protrusion of the lower jaw;
- Dupuytren's contracture, in some cases - peripheral polyarthropathy;
- Impaired glucose absorption and vitamin D metabolism, development of hypocalcemia;
- Peyronie's disease.
In case of hypersensitivity or intolerance to the drug, allergic reactions may develop, including fever, eosinophilia, drug-induced lymphadenopathy and skin rash, which may be a prodromal symptom of more severe reactions, including toxic epidermal necrolysis and Stevens-Johnson syndrome.
With long-term use of Difenin and the absence of sufficient solar radiation or an adequate diet that would satisfy the need for vitamin D, the development of osteomalacia and rickets is possible.
Substance-powder Diphenine
Instructions for medical use of the drug
Description of pharmacological action
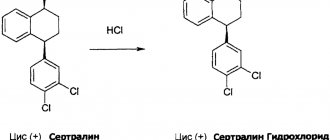
Anticonvulsant, hydantoin derivative. It has anticonvulsant, antiarrhythmic, analgesic, and muscle relaxant effects. It is believed that the anticonvulsant effect is due to the stabilization of the membranes of neurons, axons and synapses, as well as limiting the spread of excitation and seizure activity. Like other hydantoin anticonvulsants, phenytoin has an excitatory effect on the cerebellum, activating inhibitory pathways that extend to the cerebral cortex. This effect may also lead to a decrease in seizure activity, which is associated with increased discharges in the cerebellum. The antiarrhythmic effect is due to the membrane-stabilizing activity of phenytoin in Purkinje fiber cells. Blocks transmembrane sodium current, reduces the permeability of the cell membrane to calcium ions. Abnormal ventricular automaticity and membrane excitability are reduced. Phenytoin also shortens the refractory period and widens the QRS complex. Increases the pain threshold for trigeminal neuralgia and shortens the duration of the attack, reducing excitation and the formation of repeated discharges. The mechanism of muscle relaxant action is apparently similar to the mechanism of anticonvulsant action. Due to its membrane-stabilizing activity, in case of motor disorders, it weakens prolonged repeated discharges and potentiation in nerve and muscle cells. Hydantoin derivatives induce microsomal liver enzymes, thereby enhancing the metabolism of simultaneously used drugs.
Indications for use
Epilepsy (grand mal seizures); status epilepticus with tonic-clonic seizures; epileptic seizures in neurosurgery (prevention and treatment). Ventricular arrhythmias (including with glycoside intoxication or associated with intoxication with tricyclic antidepressants). Trigeminal neuralgia (as a second-line agent or in combination with carbamazepine).
Release form
powder substance; double-layer polyethylene bag (bag) 1 kg, paper bag (bag) 1; powder substance; double-layer polyethylene bag (bag) 5 kg, paper bag (bag) 1; powder substance; double-layer polyethylene bag (bag) 10 kg, paper bag (bag) 1; powder substance; double-layer polyethylene bag (bag) 15 kg, paper bag (bag) 1;
Pharmacodynamics
Anticonvulsant, hydantoin derivative. It has anticonvulsant, antiarrhythmic, analgesic, and muscle relaxant effects. It is believed that the anticonvulsant effect is due to the stabilization of the membranes of neurons, axons and synapses, as well as limiting the spread of excitation and seizure activity. Like other hydantoin anticonvulsants, phenytoin has an excitatory effect on the cerebellum, activating inhibitory pathways that extend to the cerebral cortex. This effect may also lead to a decrease in seizure activity, which is associated with increased discharges in the cerebellum. The antiarrhythmic effect is due to the membrane-stabilizing activity of phenytoin in Purkinje fiber cells. Blocks transmembrane sodium current, reduces the permeability of the cell membrane to calcium ions. Abnormal ventricular automaticity and membrane excitability are reduced. Phenytoin also shortens the refractory period and widens the QRS complex. Increases the pain threshold for trigeminal neuralgia and shortens the duration of the attack, reducing excitation and the formation of repeated discharges. The mechanism of muscle relaxant action is apparently similar to the mechanism of anticonvulsant action. Due to its membrane-stabilizing activity, in case of motor disorders, it weakens prolonged repeated discharges and potentiation in nerve and muscle cells. Hydantoin derivatives induce microsomal liver enzymes, thereby enhancing the metabolism of simultaneously used drugs.
Pharmacokinetics
When taken orally, absorption is slow and varies depending on the dosage form used. With intramuscular administration, absorption is also slow, but almost complete - 92%. Phenytoin penetrates into the cerebrospinal fluid, saliva, semen, gastric and intestinal juice, bile, and is excreted in breast milk. Penetrates through the placental barrier, concentrations in maternal blood plasma are equal to concentrations in fetal plasma. Protein binding 90% or more. Metabolized in the liver with the participation of isoenzymes CYP2C9, CYP2C19 with the formation of inactive metabolites. It has been established that a constant amount of the active substance is metabolized due to the saturation of the enzyme system responsible for the metabolism of phenytoin, which occurs when therapeutic concentrations are reached. Therefore, a small increase in dose may lead to a disproportionately significant increase in plasma concentrations of the active substance and T1/2. Phenytoin is an inducer of the isoenzymes CYP1A2, CYP3A4. T1/2 depends on the dose, the concentration of the active substance in plasma. It is excreted by the kidneys in the form of metabolites and through the intestines.
Use during pregnancy
Phenytoin should not be used during pregnancy unless the benefit to the mother outweighs the risk to the fetus. There is anecdotal evidence of tumor formation (including neuroblastoma), cleft lip and palate in children whose mothers received phenytoin during pregnancy. Phenytoin is excreted into breast milk in concentrations sufficient to cause side effects in a nursing infant. In this regard, the use of phenytoin during lactation is not recommended.
Contraindications for use
Morgagni-Adams-Stokes syndrome, AV block II and III degrees, sinoatrial block, sinus bradycardia, liver and kidney dysfunction, heart failure, cachexia, porphyria, hypersensitivity to phenytoin.
Side effects
From the central nervous system and peripheral nervous system: possible - nystagmus, ataxia, confusion, mood changes, muscle weakness, impaired coordination of movements, dizziness, sleep disturbances, slurred speech or stuttering, hand tremors, transient nervousness; rarely - peripheral neuropathy. From the digestive system: possible - nausea, vomiting, constipation, toxic hepatitis, liver damage. Gingival hyperplasia can occur during the first 6 months of therapy and begins with gingivitis, most often observed in patients under the age of 23 years. From the hematopoietic system: rarely - thrombocytopenia, leukopenia, granulocytopenia, agranulocytosis, pancytopenia, megaloblastic anemia. From the endocrine system: possible - hypertrichosis, enlargement of facial features, including thickening of the lips, widening of the tip of the nose and protrusion of the lower jaw. From the metabolic side: possible - impaired absorption of glucose due to inhibition of insulin release, impaired metabolism of vitamin D and the development of hypocalcemia. From the musculoskeletal system: possible - Dupuytren's contracture; rarely - peripheral polyarthropathy. With prolonged use, the absence of an adequate diet that satisfies the need for vitamin D, or sufficient solar radiation during the treatment period, osteomalacia and rickets may develop. Allergic reactions: rarely - skin rash, which may be a prodromal sign of more severe skin reactions (Stevens-Johnson syndrome, toxic epidermal necrolysis), eosinophilia, fever, drug-induced lymphadenopathy. Other: rarely - Peyronie's disease.
Directions for use and doses
For oral administration in adults, the initial dose is 3-4 mg/kg/day, followed by increasing the dose until the optimal therapeutic effect is achieved. In most cases, the maintenance dose is 200-500 mg/day in one or more doses. Children - 5 mg/kg/ in two doses, followed by increasing the dose to no more than 300 mg/ Maintenance doses - 4-8 mg/kg/ For intravenous administration to adults and children, the initial dose is 15-20 mg/kg. Depending on the clinical situation, a single dose may be 50-100 mg/kg. For newborns, the initial dose is also 15-20 mg/kg. Adults can be administered intramuscularly in a single dose of 100-300 mg.
Interactions with other drugs
When used simultaneously with drugs that have a depressant effect on the central nervous system, the depressant effect on the central nervous system may be enhanced. With the simultaneous use of amiodarone, antifungals (including amphotericin B, fluconazole, ketoconazole, miconazole, itraconazole), metronidazole, chloramphenicol, chlordiazepoxide, diazepam, dicumarol, histamine H1 receptor blockers, halothane, isoniazid, methylphenidate, omeprazole, fluoxet ina , estrogens, salicylates, succinimides, sulfinpyrazone, sulfonamides, tolbutamide, trazodone, it is possible to increase the concentration of phenytoin in the blood plasma, which leads to an increase in its therapeutic effect and increases the risk of side effects. The therapeutic effect of antifungals, clozapine, GCS, dicumarol, digitoxin, doxycycline, furosemide, estrogens, oral contraceptives, quinidine, rifampicin, vitamin D changes with the simultaneous use of phenytoin. When used simultaneously with phenothiazine derivatives (including chlorpromazine, prochlorperazine, thioridazine), phenobarbital, and antitumor agents, an increase or decrease in the concentration of phenytoin in the blood plasma is possible. The effect of phenytoin on plasma concentrations of phenobarbital is unpredictable. When used simultaneously with acetazolamide, osteomalacia and rickets are possible. When used simultaneously with acyclovir, it is possible to reduce the concentration of phenytoin in the blood plasma and reduce its effectiveness. With simultaneous use of valproic acid during the first few weeks, the total concentration of phenytoin in the blood plasma may decrease due to its displacement from sites of binding to plasma proteins by sodium valproate, induction of microsomal liver enzymes and acceleration of phenytoin metabolism. Next, the metabolism of phenytoin is inhibited by valproate and, as a result, the concentration of phenytoin in the blood plasma increases. Phenytoin reduces plasma concentrations of valproate, probably by increasing its metabolism in the liver. It is believed that phenytoin, as an inducer of liver enzymes, also increases the formation of a minor but hepatotoxic metabolite of valproic acid. With simultaneous use, the plasma concentrations of verapamil, nimodipine, and felodipine decrease. A case has been described of an increase in the concentration of phenytoin in the blood plasma and the development of toxic effects when used simultaneously with gabapentin. With simultaneous use, a decrease in the concentration of desipramine in the blood plasma is possible. When used simultaneously with diltiazem and nifedipine, it is possible to increase the concentration of phenytoin in the blood plasma and create a risk of developing toxic effects. When used simultaneously with disulfiram, it is possible to increase the concentration of phenytoin in the blood plasma with the development of toxic reactions; with imipramine, clarithromycin - it is possible to increase the concentration of phenytoin in the blood plasma. When used simultaneously with carbamazepine, folic acid, reserpine, sucralfate, vigabatrin, the concentration of phenytoin in the blood plasma may decrease and its therapeutic effect may decrease. In patients receiving phenytoin, the effectiveness of paracetamol may be reduced. When taking pyridoxine at a dose of 200 mg/day, a decrease in the concentration of phenytoin in the blood plasma is possible. When used simultaneously with ritonavir, there are reports of increased plasma concentrations of phenytoin. It is believed that interaction is possible, but its nature has not been definitively established. When used simultaneously with sucralfate, the absorption of phenytoin is reduced. When used simultaneously with theophylline, it is possible to reduce the plasma concentrations of phenytoin and theophylline and reduce their effectiveness. When used simultaneously with felbamate, it is possible to increase the concentration of phenytoin in the blood plasma. When used simultaneously with phenylbutazone, cases of increased concentrations of phenytoin in the blood plasma with the development of toxic reactions have been described. When treating folic acid deficiency, the use of folic acid preparations reduces the effectiveness of phenytoin. When used simultaneously with cimetidine, the concentration of phenytoin in the blood plasma increases, and there is a risk of developing toxic effects. When used simultaneously with ciprofloxacin, a decrease or increase in the concentration of phenytoin in the blood plasma is possible. The interaction is ambiguous.
Special instructions for use
If you are hypersensitive to one of the hydantoin anticonvulsants, hypersensitivity to other drugs in this group is also possible. Sudden cessation of phenytoin treatment in patients suffering from epilepsy may trigger the development of withdrawal syndrome. In patients with epilepsy, if abrupt discontinuation of phenytoin is necessary (for example, in the event of allergic or hypersensitivity reactions), anticonvulsants other than hydantoin derivatives should be used. Phenytoin undergoes intensive metabolism in the liver, so patients with impaired liver function, as well as the elderly, require dosage adjustment. During treatment, especially long-term treatment, a diet that satisfies the need for vitamin D and exposure to UV radiation is recommended. When using the drug in children during the growth period, the risk of developing side effects from connective tissue increases. In acute alcohol intoxication, the concentration of phenytoin in plasma may increase, and in chronic alcoholism, it may decrease. Effect on the ability to drive vehicles and operate machinery. During the treatment period, a slowdown in the speed of psychomotor reactions is observed. This must be taken into account by persons engaged in potentially hazardous activities that require increased attention and speed of psychomotor reactions.
Storage conditions
List B: In a dry place, protected from light, at a temperature not exceeding 25 °C.
Best before date
60 months
ATX classification:
N Nervous system
N03 Antiepileptic drugs
N03A Antiepileptic drugs
N03AB Hydantoin derivatives
N03AB02 Phenytoin
special instructions
Patients with epilepsy during the period of Difenin withdrawal are prescribed anticonvulsants that do not belong to the group of hydantoin derivatives, since abrupt cessation of treatment can cause the development of withdrawal syndrome.
During the period of use of Diphenin, especially long-term, it is recommended to adhere to a diet that satisfies the body’s need for vitamin D.
The concentration of phenytoin in the blood can be increased by phenylbutazone, felbamate, diltiazem, gabapentin and cimetidine, in some cases this is accompanied by the development of toxic effects. A decrease in the concentration of the active substance and, as a result, a decrease in the effectiveness of Diphenin, is possible when it is used simultaneously with folic acid, vigabatrin, reserpine, carbamazepine and sucralfate.
It should be borne in mind that when using the medicine during the growth period of children, the risk of developing side effects from connective tissue increases.
Phenytoin may negatively affect the speed of psychomotor reactions. This must be taken into account by people driving vehicles and working in potentially hazardous industries.
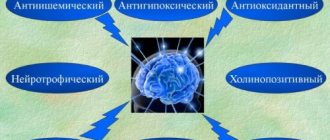
Properties and mechanism of action
The peculiarity of Diphenin is that it has an anticonvulsant effect, but without a pronounced hypnotic effect. The mechanism of this action has not been fully established, but it is believed that this is achieved by reducing the excitability of neurons in the epileptic focus, as well as by influencing neurotransmitters.
Other actions provided include:
- blocking sodium channels and prolonging their inactivation time;
- the formation and propagation of high-frequency discharges is not allowed;
- providing an antiarrhythmic effect, which most likely occurs due to the normalization of the entry of calcium and sodium ions into the cells of the cardiac Purkinje fibers;
- suppression of abnormal automatism;
- increasing the duration of the work potential in the His-Purkinje system due to a reduction in the duration of repolarization;
- reduction of the refractory effective period.
As for pharmacokinetics, there is a “first pass” effect through the liver. Then the active substance penetrates into saliva, cerebrospinal fluid, intestinal and gastric juice, sperm, bile or breast milk through the placenta. Almost completely binds to plasma proteins. The period for reaching the maximum concentration of the drug in the blood serum ranges from one and a half to three hours. A stable concentration is mainly achieved on days 5-10, provided that the daily recommended dosage is used.
The concentration of Diphenin in the serum, which will be optimal to obtain a therapeutic effect, depends on the type of epileptic seizures in the patient.
Therefore, doctors monitor the effectiveness of the drug not by its concentration in the serum, but by how the disease clinically manifests itself.
Principles of drug substitution
Recently, some difficulties have arisen with the supply of the drug “Difenin” to pharmacy chains. The manufacturer of this anticonvulsant is Lugansk Chemical Pharmaceutical Plant (Ukraine), Usolye-Sibirsky Chemical Pharmaceutical Plant OJSC and Pharmstandard LLC. Some difficulties with the political situation in Ukraine have led to a reduction in the supply of this medicine to the network of Russian pharmacies. There are more than ten names of analogue drugs on the modern pharmaceutical market. The attending physician must decide what can replace Diphenin, and he will also adjust the treatment regimen according to the rules for taking the new drug. When replacing a drug, it is important to select an adequate replacement; only a qualified specialist can do this, based on the patient’s individual indicators.
Main principles of treatment with anticonvulsants
The main treatment for epilepsy is drug therapy. The basic principles of such therapy are:
- Early start of treatment.
- Preference for monotherapy.
- The correct choice of drug for the treatment of convulsive syndrome.
- Using rational combinations of drugs if necessary.
- Abrupt discontinuation of medications is inadmissible.
- Duration and continuity of therapy with gradual withdrawal of the drug upon the onset of stable remission.
If the patient feels well while taking this medicine, the doctor can adjust the treatment using a drug with a completely identical effect to the drug “Difenin”. Synonyms of this drug are known under the names “Dilantin”, “Phenytoin”.