Due to various diseases of the brain, the electrical activity of its cells changes.
The patient develops an epileptic syndrome, characterized by recurrence of convulsive attacks.
In most cases, attacks disappear after the underlying disease is eliminated.
Of course, there is a risk of developing true epilepsy, but with appropriate treatment it does not exceed 10%. Patients with ES do not experience mental disorders or decreased intelligence characteristic of epileptics.
What it is
Epileptic syndrome is repeated convulsive seizures that develop against the background of a brain disease. In other words, it is not an independent disease, but the result of other brain pathologies.
Causes of ES in children:
- Birth injury.
- Intrauterine hypoxia.
- Hereditary metabolic disorder.
- Infectious diseases.
The most common causes of the disease in adults:
- Head injuries.
- A brain tumor.
- Hypoxia.
- Infections (meningitis, encephalitis).
- Stroke.
- Multiple sclerosis.
Another name for epileptic syndrome is symptomatic epilepsy, that is, seizures are a symptom of a serious brain disease.
Hereditary predisposition to the occurrence of ES is of great importance. If close relatives have epilepsy, the likelihood of developing epilepsy increases to 30%.
Diagnostics
It should also be noted that the diagnosis of episyndrome is not final. This is a part of the general diagnosis, a complex of symptoms. So the problem can only be dealt with if the root cause is eliminated. How can episyndrome be diagnosed? For this today there are two main and most informative methods:
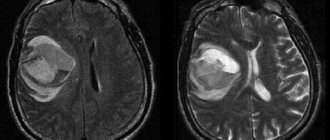
- CT. It is based on the use of x-rays. However, it differs from x-rays in the higher quality of the resulting image.
- MRI. In this case, the human body is not exposed to radiation. There is a strong magnetic field at work here.
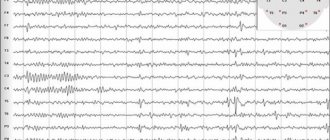
These methods help the doctor make a diagnosis and rule out other brain lesions. But an electroencephalogram can not only record the seizures themselves, but also determine their location.
Symptoms in children and adults
Symptomatic epilepsy manifests itself differently, depending on the location of the brain lesion. In medicine, the following types of disease are distinguished: frontal, parietal, temporal.
When the frontal lobe is damaged, the following symptoms occur:
- olfactory hallucinations;
- convulsive clenching of hands, pressing of legs to the stomach;
- rolling eyes, drooling.
Parietal ES is manifested by the following signs:
- loss of orientation in space;
- fainting;
- numbness of the limbs, face.
Symptoms of the temporal type of pathology:
- sleepwalking;
- confusion;
- bouts of euphoria;
- visual hallucinations;
- feeling of heat in the stomach, nausea.
In children, the nervous system is not yet strong, so ES has more pronounced symptoms:
- rhythmic spasms throughout the body;
- intermittent breathing;
- pale skin;
- flexion of limbs;
- disturbance of consciousness;
- foaming from the mouth.
The average duration of a seizure is 3-4 minutes.
After it, the patient feels lethargic, drowsy, and does not remember what happened to him. Along with long-term ones, short-term attacks appear, during which the patient momentarily loses consciousness, looks at one point, and makes chaotic movements with his hands. Then he comes to his senses as if nothing happened.
Episyndrome symptoms
How does episyndrome manifest? Symptoms for this problem are focal. That is, the manifestations of the disease depend on where exactly the affected area is located.
Episyndrome frontal. In this case, attacks will be accompanied by the following conditions:
- The patient's limbs may suddenly tense and stretch.
- The patient may involuntarily smack his lips, chew, and roll his eyes. Salivation may occur involuntarily.
- There may be a painful and sharp contraction of the muscles of the limbs or face.
- Sometimes there are aromatic hallucinations.
Temporal episyndrome. In this case, the disease manifests itself as follows:
- Hallucinations of vision, smell, and hearing may occur.
- There are mood swings from euphoric feelings to dysphoria.
- Patients may be tormented by obsessive thoughts, sleepwalking, and a feeling of deja vu.
Parietal episyndrome is characterized by the following conditions:
- Patients often complain of numbness in certain areas of the body.
- There is a disturbance of consciousness, freezing of the gaze.
- Sometimes there is disorientation and dizziness.
Episyndrome and epilepsy - what is the difference
It is necessary to differentiate true epilepsy from epileptic syndrome.
The main difference is in the origin of the pathology . Episyndrome always develops against the background of another brain disease.
Epilepsy is an independent disease that often occurs for unknown reasons.
With epilepsy, the patient experiences progressive mental disorders: psychosis, amnesia. Such patients are characterized by personality changes, expressed in decreased intelligence, impaired thinking, and changes in mood. With ES this practically does not happen.
Children with epilepsy experience hyperactivity or lethargy, increased aggression, and sadistic manifestations. These children cannot study in a regular school.
With episyndrome, the above manifestations are absent, children can attend educational institutions along with healthy peers.
If the underlying brain disease, which is the root cause of the development of ES, is eliminated, all signs will disappear. In other words, SE does not mean that the patient has epilepsy.
Find out more about epilepsy:
- forms and stages of the disease, its symptoms and signs, diagnostic methods;
- the patient’s lifestyle and menu, the ability to become pregnant and give birth if this disease is present;
- common consequences of the disease, preventive measures.
About children
It is very important to promptly diagnose epilepsy or episyndrome in children. This is why children need to be closely monitored not only at home, but also in educational institutions. So, at the first symptoms, the child should be sent for examination. And if seizures (convulsions, fainting) “tell” about the episyndrome, then epilepsy is a more dangerous and serious disease when changes in personal characteristics and mental processes occur. Thus, the first alarming indicators of epilepsy in children are as follows:
- There can be either restlessness and increased activity, or a completely opposite state - inertia and lethargy.
- Children may be characterized by negativism and stubbornness.
- Often guys become cruel, their behavior borders on sadistic.
- Children's actions are destructive and aggressive. They can be directed not only at others, but also at themselves (auto-aggression).
It is also important to note that while children with epilepsy can be educated in general educational institutions, in most cases with epilepsy, children require home schooling.
Treatment
Treatment of epileptic syndrome begins with identifying and eliminating the cause. Basic principles of therapy:
- Treatment of infectious pathogens (meningitis, encephalitis).
- Surgical removal of a brain tumor.
- Prescription of drugs that improve cerebral circulation (after a stroke).
- The use of antipyretics (if attacks occur due to high temperature).
In cases where it is impossible to completely eliminate the cause of the attacks (TBI, intrauterine hypoxia, birth trauma, multiple sclerosis), the patient is prescribed anticonvulsants (Carbamazepine, Konvulex, Phenobarbital).
A special diet with a high fat content is also indicated.
The body uses fats as its main source of energy, which reduces the frequency of seizures.
The duration of treatment depends on the patient's condition. If attacks do not occur within a year, then the dosage of medications is gradually reduced, then the drugs are stopped completely.
Sometimes they resort to surgery, during which they act on the excitation center in the brain. Most often, surgical treatment is indicated for the temporal type of ES.
Prevention
Prevention of the disease includes a whole range of therapeutic and preventive measures that have the greatest effect in the earliest possible time after the occurrence of a traumatic brain injury. Prevention is more focused on disrupting the chain of epilepsy pathogenesis.
Previous use of carbamazepine or valproic acid in small doses significantly reduces the risk of attacks accompanied by convulsions.
An elementary preventative method for preventing post-traumatic epilepsy is to avoid traumatic brain injury and use personal protective equipment during a dangerous work process, for example, at a construction site or in production.
How to live with a disease
Patients with ES can easily live a normal life without feeling inferior. To prevent an attack, you must follow some recommendations:
- Beware of overheating and strong temperature increases.
- Stick to a low-carb diet.
- Eat less spicy and salty foods.
- Do not drink tonic drinks (tea, coffee, energy drinks).
- Quit alcohol and smoking.
- Avoid stressful situations.
With frequent convulsive seizures, patients cannot perform their work duties and receive a disability group.
If attacks occur rarely, the patient can work, but there are a number of activities that are contraindicated for this disease.
Living with epilepsy
Contrary to popular belief that a person with epilepsy will have to limit himself in many ways, that many roads in front of him are closed, life with epilepsy is not so strict. The patient himself, his loved ones and those around him need to remember that in most cases they do not even need to register a disability. The key to a full life without restrictions is the regular, uninterrupted use of medications selected by a doctor. The brain, protected by drugs, becomes less susceptible to provoking influences. Therefore, the patient can lead an active lifestyle, work (including on the computer), do fitness, watch TV, fly airplanes and much more.
But there are a number of activities that are essentially a “red rag” for the brain of a patient with epilepsy. Such actions should be limited:
- Car driving;
- Working with automated mechanisms;
- Swimming in open water, swimming in a pool without supervision;
- Self-cancellation or skipping pills.
There are also factors that can cause an epileptic attack even in a healthy person, and they should also be wary of:
- Lack of sleep, night shift work, 24-hour work schedule.
- Chronic use or abuse of alcohol and drugs
What is positron emission tomography (PET)?
PET is based on the phenomenon of recording two oppositely directed gamma rays of identical energies resulting from annihilation. The process of annihilation occurs in cases where, with the introduction of metabolites labeled with a short-lived radioisotope, a positron emitted by the nucleus of the radioisotope meets an electron in the patient’s tissues. To conduct research in the interictal period, 2-deoxy-2-(18F)fluoro-D-glucose is used. In case of temporal lobe epilepsy in the interictal period, identification of foci of hypometabolism in the area of epileptogenic foci is indicated. These foci are detected in approximately 80% of patients with temporal lobe epilepsy. However, foci of hypometabolism detected on PET are more extensive than structural changes on MRI and focal changes on EEG and may involve ipsilateral regions of the Sylvian fissure and ipsilateral regions of the parietal lobe.
Functional neuroimaging
Designed to assess the functional state of the cerebral cortex in epilepsy, i.e. assessing the intensity of cerebral blood flow and the nature of metabolic changes in areas of the cortex suspected of epileptogenesis.
Why is it necessary to use neuroimaging methods in epilepsy?
The morphological state of the brain in epilepsy has always been an area of intense interest for neurologists, epileptologists and the object of diverse research.
Currently, the generally accepted opinion is that cranial radiography, used as a method of studying patients with epilepsy, is extremely low in information content. Almost all radiographs are normal, with the exception of traces of previous skull fractures or areas of calcification of the brain substance (for example, with toxoplasmosis, tuberous sclerosis). Neuroradiological research in epilepsy has given a powerful impetus to a new round of research devoted to the etiopathogenesis of epileptic seizures and optimization of syndromic classification.
What are the indications for neuroimaging in epilepsy?
To date, according to the recommendations of the Commission on Neuroimaging of the International League Against Epilepsy (1996), the absolute indication for neuroimaging methods are any epileptic seizures, with the exception of those that are obviously idiopathic (genetically determined) forms (in the absence of special indications), including: childhood absence epilepsy, benign myoclonic epilepsy of early age, juvenile absence epilepsy, childhood benign epilepsy with centrotemporal spikes (rolandic epilepsy). “Special” cases mean cases with atypical forms of these syndromes associated with neuropsychic deficits, the taxonomic position of which is not defined in the Classification of Epilepsy.
Which neuroimaging method is the most informative for epilepsy?
Speaking about the comparative information content of neuroradiological diagnostic methods, it should be noted that the vast majority of authors rely on magnetic resonance imaging (MRI) of the brain to identify structural changes in the brain. S. Garcia-Assensio et al. (1995) showed that various structural changes in the brain are detected in 36% of patients with epilepsy with normal parameters of the initial CT study.
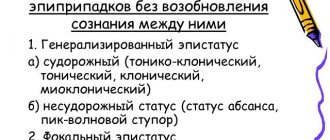
Epileptic seizure
The occurrence of an epileptic attack depends on a combination of two factors in the brain itself: the activity of the seizure focus (sometimes also called epileptic) and the general convulsive readiness of the brain. Sometimes an epileptic attack is preceded by an aura (a Greek word meaning “breeze” or “breeze”). The manifestations of the aura are very diverse and depend on the location of the part of the brain whose function is impaired (that is, on the localization of the epileptic focus). Also, certain conditions of the body can be a provoking factor for an epileptic attack (epileptic attacks associated with the onset of menstruation; epileptic attacks that occur only during sleep). In addition, an epileptic seizure can be triggered by a number of environmental factors (for example, flickering light). There are a number of classifications of characteristic epileptic seizures. From a treatment point of view, the most convenient classification is based on the symptoms of attacks. It also helps to distinguish epilepsy from other paroxysmal conditions.
International Classification of Epileptic Seizures (ILAE, 1981)
- Partial (focal, local) seizures. Simple partial seizures occurring without impairment of consciousness. Motor seizures:
- focal motor without march;
- focal motor with march (Jacksonian);
- adversive;
- postural;
- phonatory (vocalization or stopping speech).
- Somatosensory seizures or seizures with special sensory symptoms (simple hallucinations, eg flashes of flame, ringing):
- somatosensory;
- visual;
- auditory;
- olfactory;
- taste;
- with dizziness.
- Attacks with vegetative-visceral manifestations (accompanied by epigastric sensations, sweating, redness of the face, constriction and dilation of the pupils).
- Seizures with mental dysfunction (changes in higher nervous activity); rarely occur without impairment of consciousness, more often they manifest themselves as complex partial seizures:
- dysphasic;
- dysmnestic (for example, a feeling of “already seen”);
- with impaired thinking (for example, daydreaming, impaired sense of time);
- affective (fear, anger, etc.);
- illusory (for example, macropsia);
- complex hallucinatory (for example, music, scenes, etc.).
- Simple partial seizure followed by loss of consciousness:
- begins with a simple partial seizure (A.1 - A.4) followed by impaired consciousness;
- only with impaired consciousness;
- Simple partial seizures (A), turning into complex and then generalized.
- Absence seizures Typical absence seizures
- only with impaired consciousness;
- changes in tone are more pronounced than with typical absence seizures;
- random attacks that occur unexpectedly and for no apparent reason;
International Classification of Epilepsies and Epileptic Syndromes (1989)
- LOCALIZATION-DETERMINED (FOCAL, PARTIAL) EPILEPSY AND SYNDROMES Idiopathic (with age-dependent onset) Benign epilepsy of childhood with central temporal peaks
- Epilepsy of childhood with occipital paroxysms
- Primary reading epilepsy
- Chronic progressive permanent epilepsy of childhood (Kozhevnikov syndrome)
- Idiopathic (with age-dependent onset) Benign familial neonatal seizures
- Nonspecific etiology Early myoclonic encephalopathy
- With generalized and focal seizures Neonatal seizures
- Situation-related seizures Febrile seizures
How to distinguish epilepsy in a newborn from physiological changes
A child under one year of age is seriously different in behavior from older children - 2-3 years old. He often makes unconscious movements with his arms and legs. And distinguishing normal development from an epileptic seizure can be difficult. But there are universal signs indicating the onset of a seizure.
| Main features | Additional signs |
| Sudden immobilization - the child seems to freeze. | Problems with breathing, until it stops. |
| The gaze is focused in one direction. | Temperature increase |
| The eyes begin to roll behind the upper eyelids. | Frequent urination and defecation. |
| There is no reaction to stimuli - light, sound, movement. | Convulsions |
| Loss of consciousness |
After the attack, the child’s normal functioning resumes.
What is magnetic resonance angiography (MRA)?
MRA is a method for visualizing vascular (vascular) structures of the brain, based on recording an MRI signal from moving hydrogen nuclei (protons), followed by computer processing and constructing a three-dimensional model. This produces an image of the blood flow itself, and not the vascular wall. This method is not associated with intravenous administration of a contrast agent.
Important!
Thanks to neuroimaging methods, the ability to diagnose the causes of epilepsy is significantly increased, and it becomes possible to obtain a completely different quality of information about the state of the brain, which makes it possible to optimize the tactics and strategy for managing such patients, including the identification of clear and timely indications for surgical treatment of epilepsy. Since 2012, patients seeking consultative and diagnostic help from neurologists-epileptologists at the Neurological Center for Epileptology, Neurogenetics and Brain Research at the University Clinic have received the unique opportunity to conduct an MRI study of the brain on the basis of the Professor’s Clinic of our university (Krasnoyarsk, Prospekt Mira, 5, tel. 8(391) 271-21-36). The choice of the MRI method, the area of maximum diagnostic search, the need for additional contrast enhancement methods is carried out by qualified neurologists-epileptologists at the University Clinic (Krasnoyarsk, Karl Marx St., 124, tel.). Author: Natalya Alekseevna Schneider, MD, Professor, Head of the Department of Medical Genetics and Clinical Neurophysiology of the Institute of Postgraduate Education, Head of the Neurological Center for Epileptology, Neurogenetics and Brain Research at the University Clinic of Krasnoyarsk State Medical University named after. prof. V.F. Voino-Yasenetsky Source: Schneider, N.A., Dmitrenko, D.V., Batukhtin, E.N., Molgachev, A.A. Modern methods of neuroimaging for epilepsy. A textbook for the system of postgraduate education of doctors. – Krasnoyarsk, 2007. – 102 p.