An arachnoid cyst is a relatively common benign formation of the central nervous system, localized both intracranially and in the spinal canal and located between the surface of the brain and the arachnoid (arachnoid) membrane.
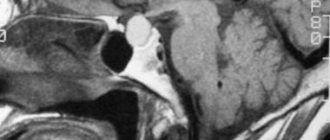
On images, they are visualized as a clearly demarcated cavity with invisible walls, pushing aside adjacent structures, with contents characterized by a pattern similar to that of cerebrosynnal fluid (hypodense on computed tomography, hyperintense on T2-weighted images, and hypointense on T1WI magnetic resonance imaging). They can also cause remodeling of the adjacent bone.
What causes a cyst in the head?
A benign spherical formation - a cyst in the brain - is filled with cerebrospinal fluid inside. The severity of symptoms depends on the size of the tumor, but it is detected during a random medical examination or when any other disease is diagnosed. Arachnoid cysts of the brain are asymptomatic in most cases. Vivid neurological symptoms are present in only 20% of patients. Factors influencing the appearance and growth of cysts:
- any brain injury;
- increase in fluid pressure inside the cystic formation;
- inflammatory process in the brain (infection, virus).
Causes
Most often, a sphenoid sinus cyst is formed against the background of:
- Acute and chronic infection.
- Pathologies of inflammatory etiology.
Also, the occurrence of cystic formation is possible in the presence of:
Allergic rhinitis, flu.
- allergic rhinitis;
- influenza, acute respiratory diseases;
- nasal and cranial trauma;
- autoimmune pathologies, during which the immune system as a whole weakens;
- anatomical disorders in the structure of the nasal passages, septum;
- congenital curvature of the nasal septum;
- narrow passages in the nose;
- nasal polyps;
- foreign object in the nasal cavity.
The disease can develop in any part of the sinus, as well as against the background of an incompletely cured cold:
- if the pathology was suffered “on the legs”;
- with inadequate self-treatment;
- if medical prescriptions were not followed.
The formation of a cyst on the main sinus of the nose occurs with a prolonged course of cold symptoms, which were not treated in time. Occasionally, the presence of some homogeneous pathologies can trigger the development of the problem.
Types of arachnoid cyst
Leading experts in the field of medicine today identify two types of neoplasms, which differ from each other in the cause of their occurrence. The first is primary, which develops in the baby while still in the womb. Secondary manifests itself in the process of the above pathologies. Also, a cyst can be simple, formed from the cerebrospinal fluid, or complex, containing various types of tissue. Based on their location, tumors in the brain are divided into:
- left or right temporal lobe;
- parietal or frontal part of the head;
- cerebellum;
- spinal canal;
- posterior cranial fossa;
- spine (perineural);
- lumbar region.
It can form as a result of inflammatory processes that developed during the prenatal period. The cause of the appearance of a neoplasm is sometimes birth trauma or meningitis in a newborn. There are often numerous developmental disorders of the fetus due to smoking, taking medications, and drinking alcohol by a pregnant woman. If the primary cyst progresses rapidly, then with severe symptoms it can be removed at any age of the child.
This type of arachnoid cyst of the brain develops after illnesses, injuries, and surgical interventions. The occurrence can be triggered by a strong blow to the head, concussion after an accident, subarachnoid hemorrhage or mechanical damage. When a secondary cyst begins to form as a result of some pathology, its walls consist of scar tissue. If a cyst in the brain of an adult has developed for another reason, then its walls contain tissue of the arachnoid membrane.
Pilonidal cyst of the coccyx: postoperative period
Patients who have undergone radical surgery to remove a pilonidal cyst of the coccyx must follow a number of the following recommendations in the postoperative period:
- For three weeks after surgery, you should not take a sitting position; prolonged lying on your back and lifting heavy objects are also prohibited;
- after the stitches are removed, you need to take a shower, wash the intergluteal fold, wear clean underwear made from natural materials;
- avoid overheating and severe cooling;
- Six months after the operation, the patient should undergo hair removal in the coccyx area;
- Two to three months after surgery, it is recommended to stop wearing tight, tight clothing.
It is necessary to understand that early contact with a proctologist increases the likelihood of maintaining health and reducing the risk of developing unwanted complications.
The proctology department of the Yusupov Hospital provides high-quality services for the diagnosis and treatment of pilonidal cysts of the coccyx using the latest medical equipment from the world's leading manufacturers. High efficiency of treatment of pathology is ensured by the use of innovative technologies, as well as the extensive practical experience of proctologists at the Yusupov Hospital. Qualified rehabilitation specialists at the clinic develop an individual set of rehabilitation measures during the rehabilitation period after surgery for each patient. The Yusupov Hospital has created all the conditions necessary for a comfortable stay for patients within the hospital walls, and provides round-the-clock, high-quality care from medical personnel.
Why is a retrocerebellar arachnoid cyst dangerous?
This type of tumor is located between the soft and hard membranes of the brain. A risk factor is that a retrocerebellar arachnoid cyst may subsequently promote cell death, a condition that leads to the development of a malignant tumor. In children, the neoplasm leads to developmental delay or hypermobility syndrome. In adults, a growing cyst increases pressure on the gray matter and brain tissue.
Main signs and symptoms of formation
Signs of a cyst appear as it grows. Headaches begin, tinnitus and skin sensitivity are disrupted. If an arachnoid cyst of the brain is not treated, paralysis of the limbs may occur, epileptic seizures may appear, deafness may increase, and vision may be lost. Symptoms of the disease are characteristic of a specific affected area.
In adults
Small bubbles with liquid contents in the brain tissue do not pose a threat to humans, and he can easily live with them throughout his life. Large formations of a progressive type have clear signs of pathology. This:
- loss of orientation;
- regular migraine;
- loss of sleep;
- violation of muscle tone;
- lameness;
- nausea, vomiting;
- twitching of limbs (involuntary);
- dizziness.
In children
When a cyst forms in newborns as a result of inflammation, damage or other pathology of the brain, it is a ramification formation that manifests itself anywhere. If the baby has parasites, for example, tapeworm, then a parasitic cyst may develop. Brain tumors are a consequence of impaired circulation of interstitial fluid. Symptoms depend on the location and type of cyst, and there is no universal list of them. The following conditions may indicate brain pathology in a child:
- pulsating fontanel;
- lethargy of the limbs;
- disoriented look;
- spitting up like a fountain after feeding.
Set of measures
If the lacunar cyst is a small cyst and the patient is not bothered by the clinical manifestations of brain dysfunction, then treatment, as a rule, is not prescribed, but it is recommended to carry out regular monitoring of the growth of the formation.
There is an opinion that asymptomatic cysts should not be considered diseases, but rather anomalies. Other experts, on the contrary, are convinced that even small formations accelerate the onset of senile dementia and contribute to the development of neurological diseases.
It is necessary to treat the pathologies that caused the cyst. For this, antibiotics, antiviral drugs, and antihypertensive drugs can be used, depending on the etiology of the disease.
In cases where formations arise as a result of hemorrhage in the brain or symptoms develop that reduce the patient’s quality of life, surgical intervention is indicated. Today this is the only way to get rid of lacunar cysts.
Methods used to remove formation:
- Bypass surgery - the patient is given a drainage tube through which the fluid filling the cavity drains out. The walls of the cyst fall and grow together. The disadvantage of this method is the high risk of infection when using the shunt for a long time.
- Endoscopy – removal of a cyst through a puncture in the skull using an endoscope equipped with a video camera. The safest and non-traumatic method. However, there are contraindications for its use.
- Craniotomy is a highly effective operation that allows you to remove cysts of any location, but with a high risk of brain damage.
At the moment, shunting and trepanation are used extremely rarely.
Diagnostic methods
The optimal diagnostic method for pathology is MRI of the brain. If there is a cyst, the final description of the tomography results will indicate: “arachnoid changes of a liquor cystic nature.” The location of the formation is revealed by the use of contrast agents. The main property of a neoplasm, unlike a tumor, is the ability to accumulate contrast. If necessary, laboratory tests and studies are carried out:
- blood for cholesterol;
- to detect infections;
- Dopplerography of blood vessels;
- measuring blood pressure (detects its surges).
Treatment methods
Treatment methods for the disease will depend on the diagnostic results. If the arachnoid cyst of the brain is small, it does not pose a health hazard. The patient will be observed by a doctor and undergo periodic examinations. During this period, it is important to eliminate the cause of the pathology and minimize the influence of negative factors. If the tumor grows rapidly, drug therapy or surgery will be used.
Drug therapy
Medium-sized cysts can be eliminated with medications. The course of treatment is prescribed individually and is carried out under the supervision of a doctor until the patient’s condition improves. Names of medications that can stop the growth of tumors:
- absorbable adhesions: Longidaz, Karipatin;
- activating metabolic processes in tissues: Actovegin, Gliatilin;
- immunomodulators: Viferon, Timogen;
- antiviral: Pyrogenal, Amiksin.
Folk remedies and herbs
With an asymptomatic brain cyst, it is possible to support the body with folk recipes:
- Tincture of hemlock herb. Eliminates headaches. The duration of treatment is 79 days. If necessary, the course can be repeated. You can prepare the tincture as follows: 100 g of seeds or crushed stems are poured with olive oil (0.5 l). The solution should be left in a dark place for three weeks. Afterwards the oil is passed through cheesecloth several times. The infusion is taken through the nose 3 times a day, 2 drops.
- Infusion from the root of Caucasian dioscorea. It has a beneficial effect on brain function: it cleanses and dilates blood vessels. The course of treatment is 2-3 months. The root (200 g) is crushed, the jar is filled, and 700 ml of vodka is poured. The composition is infused in a cool place for 5 days. Afterwards, the infusion is drained and another 700 ml of vodka is poured. After 5 days, both compositions are mixed, filtered and consumed 2 tsp. three times/day before meals.
- Yeast elixir. Helps reduce inflammation and normalize intracranial pressure. The course of treatment is three weeks. Yeast (1 tablespoon) is mixed with dried elecampane grass (40 g) and three liters of boiled water. Leave for 2 days, then take half a glass 4 times a day.
Complications
The optic nerves and brain are located near the sphenoidal cavity, which can cause additional problems if inflammation develops in it. In the process of enlargement, the cystic formation can fester or transform into a mucocele - a formation that occupies the entire space of the sphenoid sinus. Sometimes infection and suppuration (pyocele) develop against the background of a mucocele.
As a result, cystic formation of the sphenoidal sinus can cause:
- severe impairment of visual function due to compression of the optic nerve;
- periosteal abscess - suppuration and softening in the tissues of the eye orbits;
- formation of osteomyelitis (infection in bone tissue);
- the formation of an abscess in the brain tissue (infection) or meningitis (inflammation in the brain).
Less obvious consequences associated with a cystic formation in the sphenoidal sinus include:
- impaired nasal respiratory function - due to poor ventilation, the brain suffers from hypoxia, which causes the development of headaches, memory loss or developmental delays (in childhood);
- decreased functionality in the kidneys, myocardium, brain, liver, changes in bone and joint structure. The reason is a regular lack of oxygen.
The disease can be cured if the pathology is identified in time and therapy is started, and also if the infection has not had time to spread to the membranes of the brain and bone structure.
Prevention
A change in the size of an arachnoid cyst should not be taken as an oncological disease, but preventive measures should be taken to maintain brain health. These include: physical activity, proper nutrition, and giving up bad habits. For people over 40 years of age, it is advisable to visit a cardiologist and neurologist for examination every six months.
Definition
Neuroepithelial cysts (NCs) , also called neuroglial or glioependymal cysts, are developmental anomalies resulting from the absorption of part of the developing neuroectoderm, from leptomeningeal neuroglial heterotopia, or from folds of the choroidal pia mater in the case of choroidal sulcal cysts. NCs can be classified according to location into intraventricular, choroidal sulcus, and intraparenchymal cysts.
Morphology
Intraventricular neuroepithelial cyst
Intraventricular neuroepithelial cysts arise from the choroid plexus, usually at the level of the glomerulus in the triangle of the lateral ventricle. In such a location, they are often bilateral, and usually do not require any treatment. However, they can increase due to the secretive activity of the hair epithelium.
Bichat's fissure cyst (choroidal fissure cyst)
Due to the relationship between the choroidal fissure and the choroid plexus, cysts associated with the choroidal fissure are considered to be of neuroepithelial origin, although they have also been classified among arachnoid cysts. Because they are located close to the hippocampus, which is often compressed, they can cause complex partial seizures.
Intraparenchymal NC
Intraparenchymal neuroepithelial cysts are very rare. Differentiation from dilated perivascular spaces (see below) may not be possible on imaging, although location in the pericommissural or periventricular regions and multiplicity strongly favor dilated perivascular spaces. Sometimes, high-resolution MRI can detect a tiny band corresponding to the vessel's entry space. In the absence of such functions, they may be considered intraparenchymal NCs. Several histologically proven cases showed glio-ependymal elements along the cyst wall
Liquid collectors for anatomical variants
Fluid reservoirs, sometimes cystic in appearance, may result from accumulation of CSF in non-arachnoid cavities, which represent paraphysiologic developmental variations. These volumes usually cause slight deformation of adjacent structures, and, as a rule, are found in oligosymptomatic or completely asymptomatic children. These conditions include pseudocystic dilatation of the perivascular (ie, Virchow-Robin) spaces, cavities of the septum pellucida, cavities of Verges, and the spaces of the velum intermedius.
Expansion of perivascular spaces (PVS or Virchow-Robin spaces)
Perivascular spaces are tiny spaces that surround the arteries, arterioles, veins and venules that penetrate the brain parenchyma. Contrary to what was commonly thought, the SVCs are not continuous with the subarachnoid space. Rather, they are separated by a single (cortex) or double (basal ganglia) layer of pia mater that invaginates with penetrating arteries. Thus, the pia mater separates the PVC from the subarachnoid space, and the PVC is not filled with CSF, but rather with interstitial fluid, with the pia mater acting as a regulatory interface between the two compartments. PVAs are also functionally important in the elimination of high molecular weight substances from the brain. Thus, blocking such pathways can lead to the accumulation of these substances in the extracellular spaces of the brain. On imaging, PVP appears as smoothly demarcated, circular, linear parallel areas that are similar in signal intensity to CSF. So they are ↓ on CT, ↓ on T1, ↑ on T2, and ↓ on FLAIR. There is no perifocal gliosis. They tend to cluster around the anterior commissure and inferior parts of the basal ganglia, as well as in the external capsule.
Fig. 58 Periventricular regions, especially posteriorly around the triangles, are another typical location of prominent VVP. Unlike other regions, the periventricular VVP may be surrounded by a hyperintense rim on FLAIR in the pediatric age group. This may reflect incomplete myelination of the white matter (ie, terminal zones) or possibly spongy changes. In white matter, their orientation is typically radial, reflecting the course of penetrating arteries within the brain parenchyma. The normal diameter of PVP does not exceed 5 mm under normal conditions. However, there are known cases of frank dilatation of the RVP, which can occur in the absence of any pathological condition as an anatomical variant. “Giant” PVS can be up to 3 cm in diameter and may be difficult to distinguish from neuroepithelial cysts on imaging. Recognition of radial orientation or direct central visualization on high-resolution MRI is helpful for correct diagnosis. Occasionally, expansion of the PVP may be widespread and involve both hemispheres of the brain. Several pathological conditions can be characterized by dilatation of the PVP. In the pediatric age group, this includes storage diseases such as mucopolysaccharidoses (ie types I and II). In these disorders, blockage of the PVP is thought to result in the accumulation of abnormal materials in the PVP. In such cases, the PVP expansion noticeably includes, in addition to the periventricular white matter, the corpus callosum. Thus, the discovery of several callosal PVAs should prompt metabolic studies. In addition, VVP can provide a route for the spread of a number of diseases, including infections, inflammation, demyelination and tumors.
Cavity of the septum pellucida and Verge's cavity
The septum pellucidum is a thin two-layer curtain located between the anterior parts of the corpus callosum above, and the anterior columns of the fornix and anterior commissure below.
News
Mechanisms of growth of arachnoid cysts.
In some patients, the treatment strategy changes as the cyst grows. The growth of the cyst can lead to neurological symptoms. In 1964, it was reported that the contents of the cyst differed in consistency from normal cerebrospinal fluid. The intracystic fluid was analyzed and different levels of phosphate, protein, ferritin and lactate dehydrogenase were found compared to normal cerebrospinal fluid. Possible mechanisms of cyst growth must therefore be reconciled with these findings. Various mechanisms of cyst growth have been proposed. Active secretion by cyst wall cells, differences in osmotic pressure gradient, or unidirectional valve mechanism are possible mechanisms.
Active secretion of fluid by the cyst.
Ultrastructural and cytochemical studies analyzed the resected wall of the arachnoid cyst. They observed similarities between the neuroepithelial lining of the cyst wall and arachnoid granulations, such as intercellular clefts and sinusoidal extensions of desmosomes at intercellular junctions, pinocytotic vesicles, lysosomal structures and the basal lamina. On the luminal surface, the cyst is densely covered with microvilli, thus suggesting active secretion. Enzyme immunoassay cytochemistry demonstrated the presence of Na-K-ATPase in the luminal membrane and alkaline phosphatase on the opposite side of the membrane. This architecture may indicate fluid transfer to the cyst lumen. The different chemical composition compared to cerebrospinal fluid can be explained by this theory.
Osmotic gradient.
The hypothesis that the arachnoid cyst grows beyond osmotic gradients has been proposed due to the slight differences in the concentration of substances compared to the cerebrospinal fluid. The thin arachnoid cyst wall with loose connective tissue may allow water penetration. However, the movement of water along the osmotic gradient must be started. Hemorrhages into the cyst with blood degradation products and inflammatory reactions can act as osmotic triggers. In primary arachnoid cysts, there is no evidence that such mechanisms predominate.
Valve mechanism.
It was found that small and medium cysts remain constant in size and easily communicate with the normal subarachnoid space. In large cysts or in growing cysts, unidirectional fluid transport may develop. In conditions with positive extra-intracystic pressure, the cyst may increase in volume. In fact, the valve, like the transfer of fluid into the cyst, is observed during endoscopic or open surgical interventions.
Other mechanisms leading to symptoms
In addition to symptoms due to cyst enlargement, several other mechanisms such as spontaneous intracystic hemorrhage due to aneurysm rupture or brain injury may cause symptoms. Patients with arachnoid cysts appear to be prone to developing chronic subdural hematomas, even after minor head trauma, which may render a previously asymptomatic cyst clinically apparent. Clinical symptoms caused by spontaneous or traumatic rupture of a cyst with subsequent formation of a subdural hygroma have also been described.
Clinical symptoms.
Clinical symptoms are determined by the location of the cyst. An arachnoid cyst can occur anywhere in the skull and spine where the arachnoid membrane is present. Additionally, they can be found in the ventricular system. In this case, it should be noted that there is a strong attachment to the choroid plexus. It has been proposed that intraventricular cysts arise from arachnoid tissue that remains in the ventricles and grows from vascular mesenchyme at the time of formation of the choroid plexus. The prevalence of arachnoid cysts in a group of healthy adults is 1.1-1.5%. The presence of a cyst in the temporal region is typical for males, and in the cerebellopontine angle for women. To date, there are no theories to explain the gender difference.
Cysts in the temporal region and Sylvian fissure.
The middle fossa is the most common location of the cyst. In a large series of pediatric and adult patients, approximately two-thirds of the cysts were located in the middle cranial fossa or Sylvian fissure. Rarely, cysts are found on both sides. Such patients may suffer from glutaric aciduria. In general, however, there is a tendency towards a location in the left hemisphere. Symptoms are either the result of a mass effect causing increased intracranial pressure or irritation of the temporal or frontal cortex. Most often, such patients suffer from headaches or seizures, as well as contralateral motor deficits. Developmental delays are more common in children with cysts. Skull asymmetry, facial asymmetry, or proptosis may also develop due to underdevelopment of the sphenoid bone.
Discussions also continue about cysts in the temporal region as a cause of mental disorders and mental deficits. It includes attention deficit disorder, hyperactivity disorder, depression, hallucinations, dementia, schizophrenia, anorexia, insomnia and other psychotic disorders.
Intraventricular arachnoid cysts.
Intraventricularly located cysts are rare. They are found in the lateral, third and fourth ventricles. Classically, these cysts become clinically evident with the development of acute or chronic hydrocephalus if the size of the cyst increases. Symptoms associated with compression of surrounding structures also occur. Cysts in the fourth ventricle, for example, can lead to cerebellar dysfunction or depression-like symptoms.
Retrocelebellar arachnoid cysts and cysts of the cerebellar-pontine angle.
The subtentorial location accounts for approximately 10% of all arachnoid cysts. Most of them are located in the cerebellopontine angle or in the retrocelebellar. Symptoms of a retrocelebellar cyst include hydrocephalus and compression of the cerebellum and brainstem. Patients mainly present with headaches or gait disturbances. A cyst of the cerebellopontine angle can block the circulation of cerebrospinal fluid in the posterior fossa and cause occlusive hydrocephalus. Compression of structures at the cerebellopontine angle can lead to symptoms of neurovascular conflict and cranial nerve dysfunction, including hearing loss, trigeminal neuralgia, hemifacial spasm, diplopia, hoarseness, dysphagia, or double vision.
Supra- and intrasellar arachnoid cysts.
Cysts located above or below the sella turcica arise in the basic subarachnoid space, in close proximity to the optic nerve, the pituitary gland and its stalk, the hypothalamus and the midbrain. In the case of a massive cyst located above the sella turcica, it can interfere with the physiological drainage of cerebrospinal fluid at the level of the third ventricle or foramen of Monro, thereby causing obstructive hydrocephalus. Visual impairment can be caused by compression of the optic nerve, and endocrine disorders by compression of the pituitary gland or its stalk. Compression of the hypothalamic structures can cause developmental abnormalities, such as premature puberty.
Spinal arachnoid cysts.
Like a cranial cyst, a spinal cyst usually causes symptoms of compression of the spinal cord and nerve roots. Symptoms of myelopathy such as ataxia, progressive paralysis can occur due to compression of the spinal cord. Radicular symptoms are due to compression of the nerve roots and include pain, sensory deficits, or weakness of innervated muscles.
Similar articles:
Articles → Quality of life of patients with spastic and pain syndromes during epidural stimulation of the spinal cord
News → The history of the profession of a neurosurgeon, or how to become a good doctor
News → A modernized Republican Vascular Center opens in Kazan
News → Savant syndrome, abbreviated as savantism (from the French savant - “scientist”).
News → 3D model of the skull for preparation for reconstructive surgery
Discuss on the forum
What is the difference between a cyst and a pseudocyst?
Domestic doctors use these concepts as synonyms. In fact, there are differences, but they are morphological, related to structure and have little effect on the outcome.
Cysts and pseudocysts are cavities filled with fluid, in the brain - with cerebrospinal fluid. Inside the cyst there is a lining of epithelium, but inside the pseudocyst there is no lining. This difference can only be detected with high-precision equipment with very high resolution, which is equipped in large medical centers. When doctors mention a cyst or pseudocyst, they mean that there are cavity formations in the brain.
Thus, a cerebral pseudocyst in newborns does not require separate treatment - it is a small bubble with fluid inside. Such children should be monitored over time by a neurologist.
What is a subependymal pseudocyst?
There are several ventricles in the brain. These are cavities for the circulation of cerebrospinal fluid. The liquor collects in them and washes the brain. Ependyma is a thin membrane that lines the inside of the ventricles and spinal canal. The cells that form ependyma belong to neuroglia or auxiliary nerve cells that perform a supporting and trophic function for nervous tissue.
Signal to parents
Statistics say that choroid plexus cysts are formed in 1-2% of cases. Their spontaneous resorption occurs by the 24th week in 90% of cases. Their size is considered small up to 5 mm.
Geneticists classify these formations as “soft” markers of chromosome abnormalities. This means that the child may have an inherited chromosomal abnormality, but does not have to. A more careful and thorough study is needed, using genetic molecular diagnostic methods.
If other developmental abnormalities are detected, it is advisable to perform amniocentesis - puncture of amniotic fluid with subsequent study of the chromosome set. The consequences of chromosomal abnormalities are incurable hereditary diseases, and parents should be aware of this.
Cyst of the right maxillary sinus or left: what is it?
A cyst is a benign neoplasm, which is a cavity with fluid inside. The contents may be mucous, purulent or serous.
A cyst can occur in any paranasal sinus, including the maxillary sinus. The maxillary sinus is a paired formation that is located in the area of the body of the upper jaw. The nasal cavity has a natural opening through which it communicates with the nasal cavity. Its lower wall is thin, which contributes to the rapid transition of the pathological process from the roots of the teeth. The mucous membrane of the upper jaw contains a small number of vessels and nerves, and therefore the disease is often asymptomatic. Both sinuses (right or left) can be affected, but bilateral involvement is extremely rare.
The disease most often develops at the age of 14–22 years. It practically does not occur in the elderly and children.
What to do if a cyst is discovered in infancy?
Basically, to ensure that the pathology does not interfere with the child’s development. A damaged subependymal area indicates that the child suffered several episodes of hypoxia in utero, or was infected.
The cyst can also replace the site of hemorrhage in the wall of the ventricle. A fairly common cause is the herpes virus; it is considered one of the causes of the formation of brain cysts. Brain damage is caused by difficult childbirth. The main thing is that the size of the cyst should not increase in the baby and development should be disrupted.
The size of the cyst is monitored using ultrasound, which is done at 3, 6, 9 and 12 months. Usually by a year, often earlier, the cyst disappears. It is also necessary to monitor the timing of development and the general condition of the child. The slightest delay requires help and correction.
The following complaints indicating increased intracranial pressure should cause alarm, especially if they appear for the first time:
- constant crying and screaming;
- general increased irritability;
- vomit;
- refusal to eat;
- convulsive attacks.
Such conditions are rare, but parental awareness is the key to ensuring that the baby grows up healthy. An enlarged cyst immediately changes the child’s behavior.
Does it matter whether the side is right or left?
Hardly ever. A cyst of the right choroid plexus is as little dangerous as a formation on the left. In half of all cases of diagnosis, the cysts turned out to be bilateral. This is especially true for formations found in the fetus. There are times when cerebrospinal fluid is already being produced, and the growth of the ventricle simply “does not have time.” Then the cerebrospinal fluid becomes blocked in the middle of the vessels, which can represent a cyst. Such cavities sometimes persist until adulthood, without revealing themselves in any way. Liquor, in contact with the villi of the plexus, has the ability to exchange substances.
Asymptomatic cysts, especially those discovered by chance, do not require treatment. They do not have any effect on the functioning of the nervous system, motor or mental function.