The ventricles of the brain (ventriculi cerebri) are cavities located in the brain, lined with ependyma and filled with cerebrospinal fluid, and play an important role - the secretion of cerebrospinal fluid. Cerebrospinal fluid circulates continuously, the whole process consists of three main stages. When one of the links in the cerebrospinal fluid circulation fails, neuralgic symptoms appear.
Ventricular system of the brain
What is a cerebral ventricle
The ventricular system of the brain is presented in the form of reservoirs in which the secreted secretion - cerebrospinal fluid - accumulates. Continuous circulation of fluid in the subarachnoid space, ventricles and spinal canal is achieved through openings (anastomosis), which are necessary for the process of cerebrospinal fluid circulation.
The choroid plexuses of the ventricles, namely glandular cells, produce cerebrospinal fluid, the amount of which is determined by a person’s age. The size of the ventricles also increases as the central nervous system matures; normally, the lateral cisterns are larger.
Type of ventricles GM
In a newborn child, the total volume of fluid is about 10 milliliters, and in an adult it is from 150 to 250. But regardless of age, the cerebrospinal fluid is renewed up to 6 times per day. How much secretion glandular cells produce per day depends on the size of the ventricles and the influence of various factors (psycho-emotional background, blood pressure, central nervous system diseases).
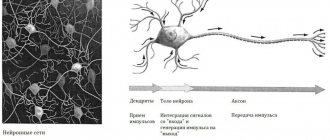
The cerebral ventricles are lined with a layer of epithelium, each cell in it has cilia that move the accumulated fluid. Thus, the cerebrospinal fluid moves passively through an open system with the help of vibration from large cerebral vessels and the villous layer. These cells (tanycytes) have processes that penetrate into the diencephalon.
Their anatomical structure is very similar to nerve fibers, so ependyma is involved in the transmission of nerve signals, but there are also unique features in the structure that affect the overall functionality of the cells.
Summarizing all of the above, we can answer the question - what are the ventricles responsible for? The main task of the cavities is the production of secretion, which in turn is an important shock-absorbing system and supports the trophism of brain tissue.
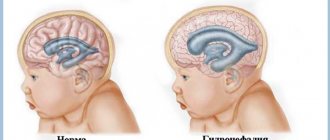
The ventricles increase in proportion to the growth of the skull. But there are deviations in which the cavities are significantly expanded and this leads to neuralgic symptoms. It is possible to assess the liquor flow and the size of cavities using non-invasive research methods.
In children under 1 - 1.5 years of age, diagnosis is carried out through the central, non-overgrown fontanel using ultrasound (neurosonography). This method is not suitable for adults, since the ossified areas of the arch do not conduct the ultrasonic wave. MRI or CT is used for diagnosis.
The table shows the normative values of the structures of the ventricular system in an adult:
| Structural unit | Average standard values in millimeters |
| Anterior horns of large cavities (lateral). | From 2 to 5 |
| Sylvian fissure. | From 3 to 5 |
| 3 cerebral ventricle | From 2.2 to 4.7 |
| 4 cerebral ventricle | From 12 to 14 |
The side tanks normally have no asymmetry and are identical in size.
For a general assessment of the ventricular system, the index is also calculated:
- Evans - the distance between the anterior horns of the lateral ventricles and the largest bitemporal diameter of the skull (from 24 to 30%);
- Schlatenbrandt-Nurenberger – width of the 3rd ventricle and transverse diameter of the skull (from 30 to 50 mm);
- Akimova-Komissarenko - the width of the 4th ventricle in relation to the diameter of the cranial fossa (from 11.5 to 14 mm.). The overall coefficient is calculated, where a value of 5.1 is the norm.
With significant asymmetry of the lateral cisterns, the reason always lies in organic pathology (inflammatory processes, neoplasms).
How many ventricles does a person have, their structure and functions
The ventricular system in the brain includes 4 tanks for storing cerebrospinal fluid. The choroid plexuses inside the cavities form a secretion, which flows through special openings inside the ventricles to the final reservoir.
Liquor circulates in an open circle; physiological fluid accumulates not only in the cavities of the brain, since the whole process goes on continuously:
- Brain connecting canal;
- Subarachnoid space between the membranes;
- Free space in the brain and spinal cord.
The size of the lateral ventricles is larger in relation to the other cisterns, so the bulk of the secretion accumulates in them. Thus, the process of liquor circulation begins from the side tanks, which includes 3 stages:
- Secretion of fluid in the ventricles;
- Movement of cerebrospinal fluid;
- Outflow.
Structure of the ventricular system
Despite the fact that after birth the child’s brain continues to develop, the basic structures and ventricular system are already formed for the functioning of the central nervous system.
Already at the end of the 4th week of intrauterine life of the fetus, the central nervous system begins to form. From the neural tube, the brain vesicles are formed, which are transformed into various structures, as well as the ventricular system.
The canal of the neural tube expands, forming two hemispheres in which large cisterns are located. From small plexuses of capillaries that pass through the walls of the anterior and posterior sections, vascular tangles are formed in the cavities.
During ultrasound screenings, the size of the large cisterns is assessed by week of intrauterine development. By the time of birth, their size should not exceed 10 mm. Exceeding the parameters of the ventricular system during embryogenesis is considered a deviation, and the diagnosis of ventriculomegaly is called into question.
Anatomical structure of the ventricular system:
- The lateral C-shaped cisterns are located in the right and left hemispheres, lined with ependyma. They do not have canals between themselves, but horns extend from each. They are a channel for moving cerebrospinal fluid into the 3rd ventricle;
- The annular cistern (3rd ventricle) is located between the optic projections, their intermediate mass grows inside the cavity. The walls of the cavity are lined with the bodies of neurons (gray mass). Through the openings it communicates with the lateral stores, the Sylvian canal serves as a connection with the 4th ventricle;
- Rhomboid storage (4th ventricle) - located in the back of the brain, the walls have several layers. The cistern has the smallest dimensions and is the connection of two sections (the spinal canal).
The functionality of the ventricles is determined by the 3 stages of the liquor circulation process, which were described earlier. Additional functions are more related to the allocated secret:
- Protective function – prevents friction of structures and prevents damage when exposed to external negative factors;
- Controls internal pressure in the skull;
- Maintains homeostasis;
- Participates in metabolic processes - delivers nutrients to brain tissue and removes decay products.
The ventricles of the brain are often subject to various pathologies, and the volume of cerebrospinal fluid is directly related to the functioning of the autonomic nervous system.
Lateral ventricles 1 and 2
The right and left hemispheres of the brain have connections, the largest of which is an interweaving of nerve fibers that runs along its entire length. Inside each hemisphere there are symmetrical cavities. Asymmetry of the cisterns in relation to the callosal groove or excess size indicates the presence of a pathological process, which led to structural changes.
Each lateral ventricle has an identical structure. On the left side of the brain is the first lateral ventricle. On the right side is the second side storage.
Tank parts:
- Center (body);
- Frontal horn (anterior);
- Occipital horn (posterior);
- Temporal horn (lower).
The anterior, inferior and posterior horns are peculiar channels that are necessary for the outflow of cerebrospinal fluid. The body in the storage visually resembles a small gap, which is surrounded by: nerve fibers on top (upper wall), a component of the striatum, visual hillocks (lower wall).
First and second ventricles
Inside the cavity there is a vascular tangle, which produces secretion. In addition to the horns, the cisterns have openings (Monroy's) that allow cerebrospinal fluid to flow into the 3rd ventricle.
The volume of the lateral ventricles and structural units must correspond to average indicators; according to the standards, each tank should not be more than 24 - 25 mm.
Based on the enlargement of the lateral ventricles of the embryo, it is possible to suspect congenital anomalies. But to make a diagnosis during embryogenesis or in an infant, the size of the structural units of each ventricle is also taken into account.
The lateral ventricles of the brain are normal for infants:
- The central part - from birth to 3 months the norm is no more than 4 mm;
- Frontal canals - from birth to 3 months, the norm is from 2 to 4 mm;
- Occipital canals - from birth to 3 months, the norm is from 10, but not more than 15 mm.
Timely diagnosis allows you to begin emergency measures immediately after the birth of the child, if the pathology is diagnosed in utero.
3rd ventricle of the brain
The third ventricle of the brain is located below the lateral cisterns at the level of the intermediate structure. The cistern is located between the visual tuberosities, but since the intermediate mass penetrates the cavity, a kind of circle is obtained.
Cerebrospinal fluid accumulates in the cavity; it differs anatomically in the number of walls:
- Lateral vaults are formed by visual tuberosities, where their intermediate mass is the internal component of the storage. The surface inside the cistern is lined with a layer of ependyma;
- Superior fornix – located under the nerve fiber line (corpus callosum);
- The lower arch is a gray plate between the arches;
- The roof of the ventricle is represented by a small part of connective tissue and vessels that come from the soft shell. The vessels penetrate through anatomical communications into the lateral stores;
- The posterior arch consists of two parts. The upper part is represented by a pineal-shaped depression, and the lower part by a commissure;
- The bottom of the storage is represented by the base of the brain.
The ventricle is responsible for the outflow of fluid through the Sylvian canal to the 4th cistern. Through the Monroe anastomosis, the 3rd ventricle communicates with the lateral cisterns. Normally, based on the results of NSG, the tank should not be more than 3.3 mm. A significant excess of the normative values indicates that the 3rd ventricle of the brain is enlarged.
This affects the functioning of the autonomic nervous system, that is, signals of excitation and inhibition for vital systems (respiratory, cardiovascular) are sent untimely. Thus, the process of self-regulation in the event of failures is disrupted.
4th ventricle of the brain
The fourth ventricle is formed from the posterior wall of the third medullary vesicle and serves as a common cavity for all posterior cerebral structures. Just like other tanks, it participates in the accumulation and transport of cerebrospinal fluid. Inside, the cavity is formed by cells similar in structure to the epidermis of all internal organs.
Inside the epidermis there are chemoreceptors that perceive chemical stimuli and reproduce them into nerve impulses. The storage is involved in immune defense; sensitive cells prevent the introduction of infectious and other health-threatening agents.
The cavity has the shape of a curved parallelepiped, but in the base area it visually looks like a rhombus, which is why the name can be found - diamond-shaped fossa.
The lower wall is formed by nerve fibers that connect the small brain to the large brain. The worm and brain sails form the roof, and the bottom is formed by an oblong structure and a bridge.
Liquor from the cavity flows into the subarachnoid space through the foramen of Luschka (two) and Magendie (one). The spinal canal enters the posteroinferior corner, and the anterosuperior corner has a connection with the aqueduct. The lateral angles form blind recesses that go around the inferior cerebellar peduncles.
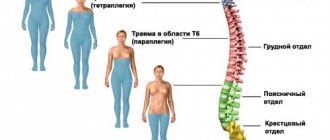
The ventricle regulates the uniform distribution of fluid between the subarachnoid space and the spinal canal. The presence of nuclei of cranial nerves (from 5 to 12 pairs) complements the overall functionality of the cavity:
- Innervation of the muscles of the face and neck;
- Sensitivity of the skin on the face;
- Performing swallowing and chewing movements;
- Taste recognition;
- Rhythm of heart contractions;
- Regulation of digestive processes and enzyme production;
- Control of extraocular muscles;
- Auditory perception;
- Coordination of movements.
The ventricle also has a connection with the arachnoid membrane, which completely covers the central nervous system. Infections that enter the cavity through a vascular connection spread and can enter any structure.
5th ventricle of the brain
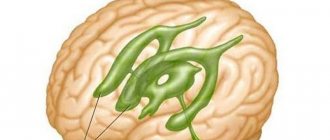
Brain diagnostics during embryogenesis is aimed at identifying various anomalies in the fetus. The fifth ventricle is considered normal during the development of the central nervous system and is a longitudinal slit-like expansion in the anterior midline of the brain (below the corpus callosum).
By the sixth month of gestation, the gap merges into one septum, and by 3–6 months of the child’s life it is completely closed. If this process does not occur, then we are talking about an anomaly in the structure and an additional ventricle is fixed - the fifth.
The ventricle can be connected to the rest of the system, but a closed version is more common. That is, the fluid does not enter through messages in the cavity, but by absorption by the pores, since the abnormal ventricle does not have its own vessels for the production of cerebrospinal fluid.
The size of the additional cavity is individual in each case, the prognosis is usually favorable. But, despite the fact that this refers to a structural feature, doctors believe that the failure occurred during embryogenesis. Quite often, the anomaly is detected due to chromosomal mutations or intrauterine infection of the fetus.
Functional impairment
Age-related changes such as cerebral atherosclerosis; vascular lesions caused by toxic causes or diseases such as diabetes mellitus, dysfunction of the thyroid gland, can lead to the death of a large number of capillaries of the choroid and their replacement by growing connective tissue. Such growths are scars, which are always larger than the original area before the lesion. As a result, large areas of the brain will suffer from deterioration in blood supply and nutrition.
The surface area of affected vessels is always less than that of normally functioning vessels. In this regard, the speed and quality of metabolic processes between blood and cerebrospinal fluid decrease. Because of this, the properties of the cerebrospinal fluid change, its chemical composition and viscosity change. It becomes thicker, disrupting the activity of nerve pathways, and even puts pressure on the areas of the brain bordering the 4th ventricle. One type of such condition is hydrocephalus, or dropsy. It spreads to all areas of the liquor supply, thereby affecting the cortex, expanding the gap between the grooves, exerting a pressing effect on them. At the same time, the volume of gray matter is significantly reduced, and a person’s thinking abilities are impaired. Dropsy, affecting the structures of the midbrain, cerebellum and medulla oblongata, can affect vital centers of the nervous system, such as the respiratory, vascular and other zones of regulation of biological processes in the body, which causes an immediate threat to life.
First of all, disorders manifest themselves at the local level, as indicated by the symptoms of damage to those same pairs of cranial nerves from the fifth to the twelfth. Which, accordingly, is manifested by local neurological symptoms: changes in facial expressions, impaired peripheral vision, hearing impairment, impaired coordination of movements, speech defects, taste abnormalities, problems with spoken language, secretion and swallowing of saliva. There may be disturbances in the activity of the muscles of the upper shoulder girdle.
The causes of dropsy may lie not only at the cellular level. There are tumor diseases (primary from nervous or vascular tissue, secondary - metastasis). If the tumor occurs near the boundaries of the 4th ventricle, then the result of an increase in size will be a change in its shape, which again will lead to hydrocephalus.
What diseases can affect the ventricles
Despite the small size of the ventricular system, the process of liquor circulation is extremely important for the functioning of the central nervous system and the whole organism. Like any organ, the cavities in the brain are often susceptible to various diseases. Hydrocephalus of the brain is considered the most common disease that has no age restrictions.
The lateral cisterns are characterized by asymmetry, which means that the cause of the anomaly lies in the malfunction of the choroid plexuses. The accumulation of cerebrospinal fluid in the cavities is not always caused by increased secretion production; blockage of the conductor channels often leads to a pathological condition.
Hydrocephalus syndrome
The expansion of the ventricles of the brain manifests itself in a bright clinic, since the central nervous system ceases to receive balanced nutrition and oxygen. Neurological symptoms appear when the brain is unable to perform its functions productively.
Pathologies in the ventricular system have primary or secondary causes and treatment is aimed at restoring all stages of liquor circulation. Diseases of the ventricles require immediate treatment, since delays threaten degenerative changes in the brain matter.
Enlargement of the ventricles of the brain in the fetus is considered a congenital disorder; early diagnosis helps to carry out emergency neurosurgical intervention immediately after the birth of the child.
Suspicion of enlargement of the lateral ventricles of the brain is always subject to a thorough diagnostic examination. Visualization of brain structures allows you to evaluate the entire ventricular system and identify the cause of the failure.
Diagnostic methods:
- Physical examination by a neurologist - neurological status is assessed;
- Consultation with an ophthalmologist – examination of the fundus;
- Neurosonography - the study is carried out through the central fontanelle for children under 1 - 1.5 years old;
- MRI or CT with contrast – layer-by-layer visualization of structures, performed on adults and children from 2 years of age;
- Doppler ultrasound – evaluates the vessels of the head and neck.
Highly accurate methods allow the assessment of all parameters in the ventricular system. An index is calculated for each cavity; if the percentage values are higher than normal, then a diagnosis of hydrocele is made. The degree of pathology is determined by the compliance of the ventricles with age criteria and the individual index.
The absorption of cerebrospinal fluid in the subarachnoid space into the vascular network directly depends on the constancy of intracranial pressure. Failure of the cerebrospinal fluid circulation leads to unstable pressure; when it decreases, fluid absorption is impossible.
Liquid is continuously produced and if there is no free outflow, then the cisterns grow, increasing in volume and width; the pressure on nearby structures depends on how enlarged the ventricles of the brain are.
Thus, during diagnosis it is revealed at what stage in the cerebrospinal fluid circulation the failure occurred and what was the cause. The primary causes always relate to congenital anomalies.
Ventricular dilatation (MRI image)
Secondary disorders in the ventricular system are a consequence of the influence of various negative factors and associated pathologies:
- Traumatic brain injuries (including birth injuries);
- Cystic formations;
- Intracranial neoplasms - tumors inside the cavity can be of intraventricular origin, that is, the primary focus, and the origin of cancer cells occurs precisely in the storage area. When atypical cells grow through the walls of the ventricle, we are talking about a secondary focus (metastasis). Ependymoma and choroidpapilloma are formed by abnormal cell division in the choroid plexus;
- Penetration of viruses and bacteria - the entry of pathogenic agents causes inflammation of the meninges and a suppurative process, as a result of which a structural change in blood vessels occurs;
- Vascular thrombosis;
- Cerebral hemorrhage – more common in older people.
Bleeding in the ventricles is a life-threatening condition. The pathology has a high mortality rate, since the clinical picture develops rapidly and the patient cannot always be transported to the hospital on time.
The disease more often affects older people (atraumatic hemorrhage), as age-related changes occur in the structure of blood vessels.
In the presence of concomitant diseases (atherosclerosis, cardiovascular pathology, blood diseases), this leads to various internal damage to the blood vessels, resulting in rupture and effusion of blood into the cavity. Intraventricular hemorrhage can also be traumatic.
A burst vessel leads to acute cerebrovascular accident. If the hemorrhage occurs in the lateral cisterns, then the blood flows through the channels to the lower ventricles. Blood clots form in the cavities, thus causing ventricular tamponade and rapidly increasing cerebral edema.
Blockage of the rhomboid cistern quickly leads to death, since the work of the vegetative centers that control vital mechanisms is disrupted.
With a timely neurosurgical operation, a drainage system is installed, with the help of which it is possible to remove intracerebral hematomas.
Poor circulation of the cerebrospinal fluid causes the accumulation of fluid in the cavities, as a result of which the ventricles enlarge and put pressure on neighboring structures. An increase in the total volume of fluid in the brain leads to an increase in ICP and the development of intracranial hypertension.
As a result of increased pressure, nerve cells die, which is dangerous for the development of encephalopathy - dystrophic damage to brain tissue is irreversible.
In children, there are cases where the lateral ventricles are dilated, but parents do not notice changes in behavior or other pathological symptoms. Perhaps this will be a variant of the norm (individual) and we are not talking about a congenital disease (ventriculomegaly), but provided that the CMD is also normal.
To do this, ICP is measured; there are several methods - non-invasive measurements using CT or MRI diagnostics, a minimally invasive technique in the form of a puncture in the lumbar spinal canal.
But neurosurgeons more often resort to the technique of puncturing cavities; when puncturing the brain, a special needle is inserted and the anterior horns of the lateral ventricles are punctured. Direct collection of cerebrospinal fluid from cavities is considered a highly informative technique.
If the ICP exceeds the indicators, then in all cases of failure of the cerebrospinal fluid circulation, emergency surgery is indicated. Installation of shunt systems allows you to restore fluid circulation, which leads to stabilization of cerebral pressure and relief of pathological symptoms.
A shunt in the brain is a silicone conductor - a tube. Through the drainage system, cerebrospinal fluid from the ventricles flows into the abdominal (or thoracic) cavity; the pump in the system takes on the function of regulating drainage and CMD.
How not to miss ventricular diseases? The causes of CNS pathologies are different, but all of them are manifested by general cerebral symptoms, which should be paid special attention to and promptly seek medical help.
In infants, liquorodynamic disturbances are often visible visually. Unossified vaults in the skull provide additional space for the accumulation of excess fluid, thus making the skull voluminous and asymmetrical. There is a delay in psychomotor development and a number of neuralgic syndromes.
But quite often hydrocephalus occurs in a compensatory manner and does not have pronounced symptoms; the signs appear gradually as fluid accumulates.
General cerebral symptoms in cases of impaired cerebrospinal fluid circulation in children and adults:
- Severe headaches. In children they manifest themselves in the form of incessant crying and anxiety, the baby refuses to eat;
- Vomiting that does not bring relief. Infants experience excessive regurgitation after feeding;
- Dizziness, nausea;
- Decreased performance. Children are characterized by lethargy or, conversely, hyperactivity;
- Loss of coordination - unsteadiness of gait;
- Decreased vision;
- Constant feeling of fatigue, drowsiness;
- Sleep disturbance;
- Violations in the psycho-emotional sphere – mood swings, up to the development of mental illness.
When a certain brain structure is compressed, additional symptoms appear - focal ones. With timely diagnosis of the pathology, hydrocephalus can be successfully treated with conservative methods (except for congenital forms).
Severe forms of dropsy or advanced cases are accompanied by convulsions and seizures. Pressure on the brain stem causes paralysis.
In case of chronic disturbance of liquor circulation, the prognosis for life is often unfavorable. Installing a shunt may be ineffective because the brain tissue already has degenerative changes.
Since various pathologies of the central nervous system have similar symptoms, a comprehensive diagnosis is important to differentiate diseases of the ventricular system.
Tumors of the fourth ventricle
Treatment of cancer >> Books on oncology >> N. A. Popov, “Intracranial tumors” Len. dept. Medgiz Publishing House, Leningrad, 1961 OCR Wincancer.Ru Given with some abbreviations
Among tumors related to the posterior cranial fossa, this localization is not uncommon. We mean primary tumors of the fourth ventricle, i.e., growing from its inherent tissue elements (ependyma, choroid plexuses). Cysticercus of the fourth ventricle (the favorite localization of a single parasite) can be completely identified with a primary tumor of the ventricle based on the clinical picture.
From a clinical diagnostic point of view, the mentioned tumors are combined with neoplasms emanating from the cerebellar vermis and spreading into the ventricular cavity - the so-called “subtentorial tumors of the midline” (N. N. Burdenko, I. Ya. Razdolsky).
A characteristic feature of tumors of this localization is the poverty or even absence at first of focal symptoms in the presence of already pronounced cerebral (hydrocephalic-hypertensive) symptoms, caused by early-occurring occlusion of the cerebrospinal fluid pathways at the level of the fourth ventricle (blockage of the Sylvian aqueduct, foramen of Magendie). Hypertensive symptoms are often remitting in nature, and the general development and course of the disease differ in some special features.
However, there is one early and even pathognomonic symptom - isolated vomiting. Its distinctive feature in tumors of the fourth ventricle is that it can occur independently of headache, not as a result of increased intracranial pressure, but be a purely local, primarily focal symptom. Its occurrence is explained by irritation of the vomiting center at the bottom of the fourth ventricle as a result of tumor pressure on the region of the vagus nerve nucleus. This symptom acquires great topical and diagnostic value when it is the only, and sometimes the first, sign of the disease; then it should suggest a tumor associated with the bottom of the fourth ventricle (the rhomboid fossa).
This circumstance is important to keep in mind, because vomiting is one of the common cerebral symptoms in brain tumors, along with other manifestations of intracranial hypertension. On the other hand, it is possible to mistakenly take this symptom (if it has been isolated for a long time) as an expression of a gastrointestinal disease, which is sometimes observed in practice and even leads to appropriate surgical interventions. In one of the observations by I. Ya. Razdolsky, vomiting, as the only symptom of a tumor of the fourth ventricle, was observed for almost 2 years.
Another clinical feature of tumors of the IV ventricle (usually with cysticercus) is Bruns syndrome, i.e. attacks that suddenly occur with sudden movements of the head, accompanied by attacks of dizziness, headache and vomiting, often with impaired consciousness, due to a temporary blockage of the liquor pathways. The appearance of this syndrome during movements (displacement of the tumor mass, especially free cysticercus), naturally forces patients to a fixed position of the head - also one of the characteristic symptoms of the localization in question.
Vestibular disorders are often observed (the position of the nucleus of the vestibular nerve at the bottom of the rhomboid fossa) and damage to the nuclei of neighboring cranial nerves. The pressure exerted by the tumor on the cerebellar vermis, especially in cases where it grows from the roof of the IV ventricle (ventral surface of the vermis), leads to disruption of statokinetics, especially gait, and general muscle hypotonia. In the later stages, the appearance of so-called cerebellar Jacksonian seizures is possible - tonic seizures with opisthotonus, autonomic disorders and which are essentially brain stem (see: Cerebellar tumors).
Vestibular disorders, especially dizziness, can be pronounced and be one of the first and even initially the only focal symptom; therefore, the possibility of mixing them with Meniere's syndrome cannot be ruled out. Their correct assessment has important topical and diagnostic significance. Unlike tumors of the temporal lobes, dizziness is not accompanied by optical and psycho-sensory disturbances. The presence of pronounced cerebral symptoms in these cases should direct thought primarily to a tumor of the fourth ventricle.
Patient G., 33 years old, was admitted to the Oktyabrskaya Railway Hospital for the second time on June 24, 1959, with complaints of headache, vomiting, diplopia, and decreased vision. Since November last year, vomiting in the morning and sometimes hiccups began to appear periodically, especially in connection with a change in position with good general health, as well as a sensation of a metallic taste in the mouth. There were no other complaints. This was associated with an alleged pregnancy. On XII/26 the patient was first admitted to the hospital for examination due to incessant vomiting. On January 2, 1959, a test curettage was performed, but no pregnancy was detected. On 14/1, the patient was transferred for treatment to the therapeutic department and from there, due to the absence of diseases of the internal organs, to the nervous department with a presumed diagnosis of obsessional neurosis (the patient, a paramedic by profession, believed that she had an unrecognized ectopic pregnancy).
Psychotherapy (hypnosis) was used, the patient's condition improved, but vomiting continued to be observed periodically as before. The patient did not experience any hypertensive symptoms, either subjective or objective, during this period; in particular, there were no headaches, the fundus was unchanged. In February, the patient was discharged and began her work.
In March, headaches began to appear for the first time, then profuse drooling. In June, the condition noticeably worsened, vision began to weaken, and diplopia appeared. Vomiting in the morning, according to the patient, was associated with head movement: while she remained in bed, they did not occur. She was sent to the hospital for the second time with a diagnosis of Bruns syndrome.
Objectively: The patient is somewhat euphoric, pulse is 70 beats per minute. Sharp attacks of headache. Bruns syndrome, but no forced head position. Fundus: pronounced congestive papillae of the optic nerves with hemorrhages. Visual acuity in both eyes is 1.0. Field of vision: for white color - no changes, for red color - limitation along all meridians, but mainly on the temporal sides, more pronounced in the right eye. Decreased corneal reflexes. Mild paresis of the abducens and facial nerves on the right. Large-amplitude horizontal nystagmus (I degree). Slight predominance of tendon reflexes and decreased abdominal reflexes on the right. Slight hypotonia in the left arm and leg, intention tremor on the left during the finger-nose test.
Craniogram: increased vascular pattern in the posterior cranial fossa, destruction of the dorsum sella. Cerebrospinal fluid (ventricular): pressure is sharply increased, protein - 0 66%o, cytosis - 3/3, blood unchanged. The patient was transferred to LIHI. Clinical diagnosis: Tumor of the midline of the posterior cranial fossa (IV ventricle). Ventriculography: Severe occlusive hydrocephalus.
10/VII 1959 operation: Trepanation of the posterior cranial fossa with laminectomy of the C1-C2 vertebrae. When opening the sharply tense dura mater, a tumor is identified on the posterior surface of the medulla oblongata. It is located in the cavity of the IV ventricle and descends to the level of the C3 vertebra, covering the brain from the sides and back. The tumor (evudymoma) is removed radically. No respiratory or cardiac disturbances were observed. The patient tolerated the operation well, and the postoperative course was without complications. X-ray therapy was performed. On 1/IX the phenomena of congestion in the fundus passed, all clinical phenomena disappeared, and on 5/IX the patient was discharged in good condition (follow-up for more than a year).
Although in this observation there were no symptoms characteristic of tumors of the fourth ventricle (forced position of the head, dizziness, static disorders, etc.), however, a history of vomiting as an isolated (focal) symptom, pathognomonic for tumors of this localization, and Bruns syndrome in combination with other manifestations of pronounced intracranial hypertension with the participation of the VI, VII, VIII cranial nerves spoke quite convincingly in favor of a tumor of the IV ventricle. With such a pronounced Bruns symptom complex, of course, cysticercus could not be excluded.
The observation is an example of the difficulties that can be encountered in assessing vomiting as the first and for a long time the only symptom of a tumor of the fourth ventricle. And this symptom occurs quite often: according to G.P. Kornyansky (on a large material) in 50%! It often misleads therapists and surgeons, who mistake it for an expression of gastrointestinal pathology, and serves as a source of serious difficulties for the neurologist in the early recognition of tumors of this localization. Thus, from a clinical point of view, the observation is a fairly typical example of tumors of the fourth ventricle.
As features, two symptoms attract attention: taste paresthesia from the very beginning of the disease and drooling that appeared later. Both of these phenomena are not usually observed with tumors of the fourth ventricle. But there is one distinctive feature of the tumor in this case - its penetration into the spinal canal, which makes the tumor cranio-vertebral in localization. It is ependymomas emanating from the bottom of the IV ventricle that tend to penetrate through the foramen of Magendie into the cistern magna and then descend to the upper cervical vertebrae (C2-C3), which also occurred in the described observation. Since the first symptom, long preceding others, in particular the general cerebral one, was signs of irritation of the vomiting center, one can think that the tumor grew from the lower corner of the bottom of the fourth ventricle.
It is also worthy of attention that an ependymoma of such a large size, enveloping the medulla oblongata on three sides and penetrating into the foramen magnum, did not manifest itself with any bulbar (as well as conduction) symptoms. In full accordance with this is the fact that the removal of the tumor was not accompanied by any respiratory or cardiac disorders: the patient tolerated the entire operation well and was discharged almost completely healthy.
However, there is also an atypical course of tumors of the fourth ventricle, which sometimes creates great difficulties in their topical diagnosis.
Patient M., 32 years old, was admitted to the hospital on August 15, 1956 with complaints of headache, noise in the head, and blurred vision. The pain has existed for about 5 years, but has intensified in the last two months. In July, congestive nipples were discovered.
Objectively: The left palpebral fissure is wider than the right, sluggish reaction of the pupils to light, with convergence the left eyeball moves outward. Congestive nipples with hemorrhages; visual acuity of the right eye - 0.5, left - 0.1 (with correction). Narrowing of the field of view along all meridians. Slight intentional trembling in the left hand, uncertainty during the heel-knee test on the left. Craniogram without changes.
Cerebrospinal fluid: increased pressure, protein - 1.65%o, cytosis - 4/3. Ventriculography through the anterior horn of the right lateral ventricle: Significant internal hydrocephalus. In the coming days, the patient's general condition worsened. Clinical diagnosis: Tumor of the midline of the posterior cranial fossa or arachnoiditis of the cisterna magna.
Operation 11/IX 1956: When the large tank was opened, the release of liquid quickly stopped. The cerebellar tonsils are strongly descended. A tumor the size of a walnut, freely located in the cavity of the fourth ventricle, was bluntly isolated. Histologically - papilloma of the choroid plexus of the fourth ventricle. After the operation, the patient's condition improved significantly; After a course of radiotherapy she was discharged in satisfactory condition. On January 18, 1957, 4 months after the operation, the patient was again admitted to the hospital due to hypertensive crises and tabloid symptoms. Suddenly, on March 10, 1957, she died from respiratory paralysis.
Section: Tumor of the choroid plexus of the fourth ventricle (papillary cancer) with invasion into the medulla oblongata. Significant hydrocephalus.
This patient did not have any symptoms characteristic of a tumor of the fourth ventricle. Signs of a significant increase in intracranial pressure, together with cerebellar symptoms, although mild, and pain in the occipital region made the most likely assumption of a postcranial localization of the process. A comparison of clinical data, ventriculography results and changes in cerebrospinal fluid confirmed the blockade of the liquor-conducting system at the level of the fourth ventricle. These facts gave reason to speak under these conditions about a subtentorial neoplasm of the midline or to assume chronic arachnoiditis of the cisterna magna. The latter was supported by the absence of any distinct cerebellar symptoms with significantly pronounced cerebral symptoms and the presence of a history of trauma. The tumor was largely caused by the severity of the course, rapidly growing congestive nipples with decreased vision, and protein-cell dissociation in the cerebrospinal fluid.
The clinical features and course of the disease in this case can be explained to a certain extent by the nature of the neoplasm itself, namely papilloma, emanating from the plexus of the fourth ventricle and undergoing malignant degeneration into choroid carcinoma. This type of tumor belongs to the most rare neoplasms of the ventricular system; in addition, they usually develop in childhood. In relation to the walls of the ventricles, papilloma is considered a primary ventricular tumor.
Being completely isolated at first, it grows freely in the cavity of the ventricle, reaching a significant size and thereby disrupting the circulation of liquor, but without having a significant effect on the adjacent brain formations. When the tumor reaches a large size, it completely blocks the liquor-conducting system (foramen of Magendie). This stage of papilloma development corresponded to a period of sharp deterioration in the patient’s condition. It is clear that the surgical intervention, by eliminating the blockade, directly eliminated almost all painful symptoms. However, later malignant degeneration of the tumor remnants led to its rapid growth with infiltration of surrounding tissues, including the medulla oblongata.
Patient D., 52 years old, was admitted to the hospital on 23/V 1958. She fell ill about three weeks ago, acutely, feeling a “blow” to the head, followed by a sharp headache; the next day, repeated vomiting. Moderate pain has been observed over the past 3 years.
Objectively: Blood pressure 150/90 mm Hg. Pulse 64 per minute. The patient tries to lie down all the time; when she tries to get up, the headache intensifies, dizziness occurs, and her general condition worsens. Moderate neck stiffness. Slight anisocoria, sluggish reaction of the pupils to light. Mild nystagmus of the eyeballs. The fundus is unchanged; sometimes notes blurred vision. Decreased hearing in both ears (otiatrician's conclusion - auditory neuritis). There are no motor, sensory or cerebellar disorders. Later, left-sided hemihypesthesia of skin sensitivity was observed, with the exception of the facial area. Tendon reflexes are uniformly animated. Cerebrospinal fluid: protein - 0.66°/oo, cytosis -2/3. Craniogram without changes.
Due to frequent vomiting of bile and suspicion of gastrointestinal disease, gastric juice was examined, which turned out to be normal. During the three-week observation (before surgery), the patient's condition was characterized mainly by forced position in bed, remitting course; Once there was a hypertensive crisis with confusion and bradycardia. Two weeks after admission, initial symptoms of congestion in the fundus of the right eye, foot clonus, hypotonia, increased tendon reflexes on the left, and Oppenheim's sign on the right were discovered.
Ventriculography through the posterior horn of the left lateral ventricle: about 50 ml of cerebrospinal fluid under high pressure is released and the same amount of gas is introduced. Intratriculograms revealed a sharp symmetrical expansion of the lateral ventricles of the brain. Clinical diagnosis: Tumor in the posterior cranial fossa.
Operation I4/VI 1958: Arachnoiditis of the posterior cranial fossa. Between the tonsils of the cerebellum on the medulla oblongata, a patch of brown tissue is visible, spreading into the cavity of the fourth ventricle and filling it. Its removal is impossible due to its close connection with the bottom of the diamond-shaped fossa. The patient died on 10/VII.
Section: Tumor of the IV ventricle, arising from the anterior surface of the cerebellar vermis and spreading to the medulla oblongata. Severe internal hydrocephalus. Histologically - polar spongioblastoma.
In this observation, the tumor originated from the ventral surface of the cerebellar vermis, filling the cavity of the fourth ventricle and spreading to the brain stem. From a clinical point of view, this type of tumor is combined with primary tumors of the fourth ventricle under the name of subtentorial midline tumors. Difficulties in diagnosis in this case were determined by the acute onset, rapid course of the disease and increased blood pressure, which gave reason to think at first even about a vascular disease.
This was aggravated by the absence of congestive nipples and radiological changes in the skull bones. The patient's gait, an important symptom of damage to the cerebellar vermis, could not be examined due to the patient's forced position in bed. However, sharp paroxysmal headaches, frequent vomiting (raising even suspicion of a gastrointestinal disease), dizziness, intensifying due to changes in body (head) position, made one think about a tumor of the posterior cranial fossa, which was confirmed by ventriculography. There was no sufficient evidence for a tumor of the fourth ventricle; The patient’s age (52 years) and the very rapid course of the disease also spoke against this, which at one time gave reason to suspect a cerebellar tumor of a metastatic nature.
Thus, the neoplasm was asymptomatic for a long time, which is generally typical for intraventricular brain tumors. Some mild changes in the cranial nerves, especially decreased hearing (auditory neuritis), nystagmus, as well as conduction disorders of skin sensitivity, are explained by the close relationship of the neoplasm to the brain stem and can occur at any localization within the posterior cranial fossa. For intraventricular tumors, stem symptoms are more typical in the terminal stages.
It should be emphasized the importance in this case of the forced position of the body, caused by a sharp deterioration in the patient’s condition with any change in body position. This symptom acquires the same importance here as the forced posture of the head in an upright position of the patient - a characteristic symptom of tumors of the fourth ventricle.
Patient Sh., 57 years old, was admitted to the hospital on 9/V 1956 with complaints of a sharp headache, accompanied by noise, sometimes with vomiting; at times dizziness and unsteadiness of gait. The pain began to appear in March last year, and soon the patient noticed decreased vision. From 4/V 1956, congestive nipples and bitemporal narrowing of the visual field were detected.
Objectively: Pronounced congestion of the nipple of the left eye, initial symptoms of congestion in the right eye. Visual acuity of the right eye - 0.6, left - 0.1 (with correction). The field of vision of both eyes is somewhat limited on the temporal side. The pupils are slightly uneven and their reaction to light is sluggish. Minor paresis of the lower branch of the right facial nerve. No motor, sensory or cerebellar disorders are observed.
Cerebrospinal fluid flowed out in frequent drops, after puncture the patient's condition improved; the amount of protein is 0.5%o, cytosis is 724/3 (lymphocytes). Repeated studies of the fluid revealed a significant increase in the number of cells, reaching 920/3 (once 1212/3) with a relatively moderate amount of protein, not exceeding 1.3%, and a decrease in sugar content to 25 mg%. Examination of the cerebrospinal fluid for parasites is negative. The number of eosinophils in the blood did not exceed 3%. Craniogram without changes.
During long-term observation, the patient's condition was characterized by repeated remissions (due to punctures) against the background of a slowly progressive deterioration - an increase in hypertension and the appearance of psychotic symptoms. Paresis of the facial nerve became more obvious, corneal reflexes faded, and deep reflexes gradually decreased. At the same time, congestion at the bottom of the eye increased and vision decreased. Headaches at night, occasionally accompanied by vomiting.
Changes in the psyche were expressed mainly in visual (sometimes very complex) hallucinations and photopsia; By the end of the observation, delusional states and at times disorientation in the environment arose, the state of stupefaction increased, and criticism noticeably weakened. Sometimes there was an imbalance when walking, and in the terminal period - a forced position of the head. Cerebellar tests remained negative. Only once was there a severe hypertensive cerebral crisis with clonic convulsions in the right arm.
Ventriculography revealed symmetrical dilatation of the entire ventricular system. In the ventricular cerebrospinal fluid, protein is 0.82%o, cytosis is 920/3. The craniograms showed signs of destruction of the back of the sella turcica. Clinical diagnosis: Neoplasm (arachnoiditis) in the posterior cranial fossa. Operation 18/IX: A parasitic cyst (cysticercus) the size of a hazelnut was discovered in the IV ventricle; it is removed, after which cerebrospinal fluid appears. The patient's condition initially began to improve, but then deteriorated again. He died on 20/X.
Section: Cysticercosis of the brain; parasitic cyst in the insula of the left hemisphere; moderate hydrocephalus; purulent meningitis.
Only a month before admission, the patient’s general cerebral symptoms began to develop quite quickly, and soon congestive nipples were discovered. The erasure of focal symptoms, their remitting course, and enormous cytosis in the cerebrospinal fluid characterized basically the entire clinical picture of the disease. It should be emphasized the height of lymphocytic pleocytosis, in the cerebrospinal fluid reaching 900 and 1200/3. Such an increase in the number of cells is not at all characteristic of brain cysticercosis. Thus, according to A. Ts. Vozna, cytosis most often ranges from 50 to 150 per 3 ml; according to I. Ya. Razdolsky - from several tens to several hundred.
These changes in the cerebrospinal fluid, together with the hypertension syndrome, made it possible for a long time to admit (by exclusion) the possibility of serous meningitis, although this was contradicted by other signs of the disease. The thought of cystcercosis did not arise: the anamnestic information in this regard was negative, there was no eosinophilia in the blood. The absence of Bruns syndrome and severe hypertensive-hydrocephalic crises, as well as local symptoms (especially vomiting, dizziness, etc.), inevitable when the bottom of the rhomboid fossa is involved in the process, spoke against the localization of the process in the fourth ventricle. Later psychotic symptoms that appeared, pronounced in the patient, are characteristic of cerebral cysticercus, but mainly with multiple localization of the parasite in the cerebral cortex. The described observation makes it possible to explain the origin of mental disorders by the intoxicating effect of the cysticercus on the vital activity of the brain as a whole, as evidenced by the very nature of these disorders, which is usually not characteristic of even significant intracranial hypertension.
Very poorly presented and unstable local symptoms could not contribute to either topical diagnosis or recognition of the nature of the process. The forced position of the head appeared only in the terminal period of the disease, when the postcranial localization became obvious. Episodically observed vestibular disorders were the only thing that could indicate the localization of the process, close to the bottom of the fourth ventricle. Ventriculography, which revealed internal hydrocephalus, allowed us to finally lean in favor of localizing the lesion in the posterior cranial fossa and made its revision necessary.
All of the above makes quite obvious the difficulties that may arise when recognizing the cysticercus of the fourth ventricle - its favorite location. Diagnosis in these cases is based on the presence from the very beginning of a remitting hypertensive-hydrocephalic syndrome in combination with the Bruns symptom complex (but possibly without it), episodic balance disorders and vestibular dizziness, and significant pleocytosis in the cerebrospinal fluid, which cannot find any other explanation. Mental disorders, including hallucinations, can also contribute to this. The presence of eosinophilia in the cerebrospinal fluid and the reaction of complement fixation with cysticercus antigen in the blood and cerebrospinal fluid make the diagnosis undoubted.
The described observations show that the source of difficulties and diagnostic errors in the accurate recognition of primary tumors of the fourth ventricle may be the absence of sufficiently pronounced symptoms characteristic of a given location.
The same applies to the diagnosis of a single cysticercus of the fourth ventricle in the presence of only general cerebral - hypertensive-hydrocephalic symptoms, the absence of general signs of a parasitic disease and negative medical history. Very high pleocytosis in the cerebrospinal fluid and significant changes in the psyche under these conditions further complicate topical diagnosis. See further: Tumors of the medulla oblongata and pons >>
Features of the third ventricle
The 3rd ventricle of the brain is part of the cerebrospinal fluid circulation system and is the connecting link between the lateral cisterns and the rhomboid fossa. In a frontal section of the brain, the cistern looks like a narrow slit, which communicates with the 4th cavity through the Sylvian aqueduct.
A feature of the cavity is the dense surrounding of various structures, as well as the presence of vegetative centers. Excessive accumulation of cerebrospinal fluid or obstructed outflow from the cavity leads to pressure on the nerve nodes that maintain internal homeostasis.
The width of the tank in an adult should not exceed 6 mm; for children under one year of age, the norm is 3–4 mm. The severity of the process is determined by the presence and severity of neurological symptoms. Diagnostic measurement of ventricular parameters allows emergency measures to be taken and, if necessary, surgical intervention.
Disturbances in liquorodynamics always require emergency treatment, which is aimed at restoring the functionality of the central nervous system and eliminating the cause of the disturbance. Degenerative changes in brain tissue cannot be restored, but installing a shunt helps improve the patient’s quality of life.