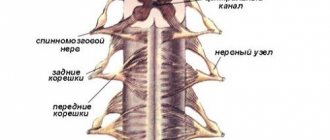
The spinal cord is located in the spinal canal and is a cylindrical cord flattened from front to back, which passes upward into the medulla oblongata, and below ends in a conical point at the level of the 2nd lumbar vertebra. The anterior and posterior roots of the spinal cord emerge from the spinal cord on both sides in longitudinal rows. At some distance from the spinal cord, the motor root merges with the sensory root, and together they form the trunk of the spinal nerve. In the intervertebral foramina, the dorsal root has a thickening - the spinal ganglion, containing sensory neurons with one process, which is then divided into two branches: one of them is central, goes as part of the dorsal root, the other, peripheral, continues into the spinal nerve. The lower lumbar and sacral roots form a complex of nerve roots called the cauda equina.
Structure of the spinal cord
Definition 1
The spinal cord (SC) is phylogenetically the oldest section of the central nervous system of vertebrates, located in the bony vertebral (spinal) canal from the first cervical vertebra to the first - second lumbar vertebrae and ends in a medullary cone, from which a thin thread stretches down, surrounded by long roots of the lower segments brain (the so-called “horse tail” is formed).
Finished works on a similar topic
- Course work Spinal cord 430 rub.
- Abstract Spinal cord 250 rub.
- Test work Spinal cord 190 rub.
Receive completed work or specialist advice on your educational project Find out the cost
The spinal cord is a cylindrical cord of segmental structure, 40-45 cm long, 1-1.5 cm in diameter and weighing about 30 g. It is slightly compressed in the anterior-posterior direction.
In the center of the spinal cord there is a reduced canal, inside of which there is cerebrospinal fluid.
In the central part of the spinal cord there is gray matter, in a cross section resembling butterfly wings or the letter H. It consists of the bodies of neurons united by processes and glia.
The gray matter of the spinal cord forms paired anterior and posterior horns. There are lateral horns in the thoracic region and upper segments of the lumbar region.
Note 1
Functionally, the anterior horns are motor, the lateral are vegetative, and the posterior are sensitive.
Have questions about this topic? Ask a question to the teacher and get an answer in 15 minutes! Ask a Question
In humans, the spinal cord consists of the following segments:
- 8 cervical C (I – VIII);
- 12 thoracic Th (I – XII);
- 5 lumbar L (I – V);
- 5 pelvic S (I – V);
- 1 - 3 coccygeal Co (I - III).
Note 2
According to the Bell-Magendie law, the posterior (dorsal) roots of the spinal cord are responsible for sensory function, and the ventral (anterior) roots are responsible for motor function.
The ratio of fibers that enter through the dorsal and exit through the ventral roots is also characteristic (for mammals - about 2: 1). It is known that the common final path for impulses coming from different receptors and competing for the common final path is the same motor neuron.
Lecture No. 15. "Functional anatomy of the spinal cord."
The spinal cord (medulla spinalis) is the initial part of the central nervous system.
It is located in the spinal canal and is a cylindrical cord flattened from front to back, 40–45 cm long and weighing 34–38 grams. From above it passes into the medulla oblongata, and from below it ends with a point - the conus medullaris at the level of 1-2 lumbar vertebrae. Here a thin terminal filament departs from it - this is a rudiment of the caudal (caudal) end of the spinal cord. The diameter of the spinal cord varies in different areas. In the cervical and lumbar regions it has thickenings (accumulations of gray matter) due to the innervation of the upper and lower extremities. On the anterior surface of the spinal cord there is an anterior median fissure, on the posterior surface there is a posterior median sulcus. They divide the spinal cord into right and left halves, which are interconnected. On each half, anterior lateral and posterior lateral grooves are distinguished. The anterior one is the place where the anterior motor roots exit the spinal cord, the posterior one is the place where the posterior sensory roots of the spinal nerves enter. These lateral grooves are the boundary between the anterior, lateral and posterior cords of the spinal cord. Inside the spinal cord there is a gap filled with cerebrospinal fluid (CSF) - the central canal. From above it passes into the 4th ventricle, and from below it ends blindly (terminal ventricle). In an adult, it partially or completely heals. Parts of the spinal cord:
- Cervical
- Chest
- Lumbar
- Sacral
- Coccygeal
Each part has segments - a section of the spinal cord corresponding to 2 pairs of roots (2 anterior and 2 posterior).
Along its entire length, 31 pairs of roots arise from the spinal cord. Accordingly, 31 pairs of spinal nerves in the spinal cord are divided into 31 segments:
- 8 – cervical
- 12 – chest
- 5 – lumbar
- 5 – sacral
- 1-3 – coccygeal
The lower spinal nerves descend down to form the cauda equina.
As the body grows, the spinal cord cannot keep up with the length of the spinal canal, and therefore the nerves are forced to descend, exiting the corresponding foramina. Newborns do not have this formation.
Inside the spinal cord there is gray and white matter. Gray - neurons that form 3 gray columns in each half of the spinal cord: anterior, posterior and lateral. In cross section, the pillars look like gray horns. There are wide anterior and narrow posterior horns. The lateral horn corresponds to the intermediate vegetative column of gray matter. The gray matter of the anterior horns contains motor neurons, the posterior horns contain sensory neurons, and the lateral horns contain intercalary autonomic neurons. There are also intercalary inhibitory neurons - Renshaw cells, which inhibit the motor neurons of the anterior horns. The white matter surrounds the gray matter and forms the cords of the spinal cord. There are anterior, posterior and lateral cords in each half of the spinal cord. They consist of longitudinally running nerve fibers collected in bundles - pathways. The white matter of the anterior cords contains descending pathways (pyramidal and extrapyramidal), and the lateral ones contain descending and ascending pathways:
- anterior and posterior spinocerebellar tracts (Gowers and Flexig)
- lateral spinothalamic tract
- lateral corticospinal tract (pyramidal)
- red nuclear tract
In the white matter of the posterior cords there are ascending pathways:
- thin (delicate) Gaulle bun
- wedge-shaped bundle of Burdach
The connection between the spinal cord and the periphery is carried out using nerve fibers passing through the spinal roots. The anterior roots contain centrifugal motor fibers, the posterior roots contain centripetal sensory fibers. This fact is called the law of distribution of afferent and efferent fibers in the spinal roots - Francois Magendie's law. Therefore, with bilateral transection of the dorsal roots of the spinal cord, the dog loses sensitivity, and the anterior roots lose muscle tone below the transection site.
The spinal cord is covered externally by 3 meninges:
- inner – soft
- medium – arachnoid
- outer - hard
Between the hard shell and the periosteum of the spinal canal there is an epidural space filled with fatty tissue and venous plexuses. Between the hard and arachnoid there is a subdural space, penetrated by thin connective tissue crossbars. The arachnoid membrane is separated from the soft membrane by the subarachnoid subarachnoid space containing cerebrospinal fluid. It is formed in the choroid plexuses of the ventricles of the brain (protective and trophic functions). The spinal cord contains special inhibitory cells - Renshaw cells - that protect the central nervous system from overexcitation.
Functions of the spinal cord.
- Reflex: carried out by the nerve centers of the spinal cord, which are segmental working centers of unconditioned reflexes. Their neurons communicate with receptors and working organs. Each metamer (transverse section) of the body receives sensitivity from 3 roots. Skeletal muscles also receive innervation from 3 adjacent segments of the spinal cord. Efferent impulses go to skeletal muscles, respiratory muscles, internal organs, blood vessels and glands. The overlying parts of the central nervous system control the periphery with the help of segmental parts of the spinal cord.
- Conduction: carried out through the ascending and descending tracts of the spinal cord. Ascending pathways transmit information from tactile, pain, temperature and proprioceptors of muscles and tendons through neurons of the spinal cord to other parts of the central nervous system to the cerebellum and cerebral cortex.
Conducting tracts of the spinal cord.
Ascending tracts of the spinal cord.
They transmit pain, temperature, tactile sensitivity and proprioceptive sensitivity from receptors to the cerebellum and the brainstem.
- anterior spinothalamic tract – afferent pathway of touch and pressure
- lateral spinothalamic tract – path of pain and temperature sensitivity
- anterior and posterior spinocerebellar pathways – Gowers and Flexig pathways – afferent pathways of muscular-articular sensitivity of the cerebellar direction
- thin (gentle) fascicle of Gaulle and wedge-shaped fascicle of Burdach - afferent pathways of muscle-articular sensitivity of the cortical direction from the lower extremities and lower half of the body and from the upper extremities and upper half of the body, respectively
Descending tracts of the spinal cord.
They transmit nerve impulses (commands) from the brainstem and underlying sections to the working organs. They are divided into pyramidal and extrapyramidal.
Pyramidal tracts of the spinal cord.
They conduct impulses of voluntary motor reactions from the CBM to the anterior horns of the spinal cord (control of conscious movements).
- anterior corticospinal tract
- lateral corticospinal tract
Extrapyramidal tracts of the spinal cord.
They control involuntary movements. An example of their work is how a person maintains balance in the event of a fall.
- reticular-spinal tract (reticulospinal): from the reticular formation of the brain
- tegmental–spinal tract (tetospinal): from the pons
- vestibulospinal (vestibulospinal): from the balance organs
- red nuclear - spinal (rubrospinal): from the midbrain
Spinal nerves and nerve plexuses.
The human spinal cord has 31 segments, hence 31 pairs of spinal nerves.
- 8 pairs of neckbands
- 12 pairs of breasts
- 5 pairs of lumbar
- 5 pairs of sacral
- 1 pair of coccygeal
Formation of the spinal nerve.
Each spinal nerve is formed by connecting the anterior motor and posterior sensory roots. When leaving the intervertebral foramen, the nerve divides into 2 main branches: anterior and posterior. Their functions are mixed. In addition, the meningeal branch departs from the nerve, which returns to the spinal canal and innervates the dura mater of the spinal cord and the white connective branch, which approaches the nodes of the sympathetic trunk. With various curvatures of the spinal column (pathological lordosis, kyphosis and scoliosis), the intervertebral foramina are deformed and pinch the spinal nerves, which leads to dysfunction, neuritis and neuralgia. With the help of these nerves, the spinal cord innervates:
- sensitive: trunk, limbs, part of the neck
- motor: all muscles of the trunk, limbs and partly the neck
- sympathetic: all organs that have it
- parasympathetic: pelvic organs
The posterior branches of all spinal nerves have a segmental arrangement and pass along the posterior surface of the body, where they are divided into cutaneous and muscular branches that innervate the skin and muscles of the back of the head, neck, back and pelvis. These branches are named after the corresponding nerves: the posterior branch of the first thoracic nerve, the second, etc. Some have names: the posterior branch of the first cervical nerve is the suboccipital nerve, the second cervical nerve is the greater occipital nerve. All anterior branches of the SMN are thicker than the posterior ones. 12 pairs of thoracic SMNs have a segmental arrangement and run along the lower edges of the ribs - intercostal nerves. They innervate the skin and muscles of the anterior and lateral walls of the chest and abdomen. May become inflamed - intercostal neuralgia. The anterior branches of the remaining SMNs form plexuses (pleksus), the inflammation of which is plexitis.
- Cervical plexus
: formed by the anterior branches of the four superior cervical nerves. located in the area of the 4 upper cervical vertebrae on the deep muscles of the neck. In front and on the side it is covered by the sternum - clavicular - mastoid muscle. Sensory, motor and mixed nerves depart from this plexus.
- Sensory nerves: lesser occipital nerve, greater auricular, transverse neck nerve, supraclavicular nerves (innervate the skin of the lateral part of the back of the head, auricle, external auditory canal, anterolateral neck, skin in the clavicle area and below it)
- Muscle branches innervate the deep muscles of the neck, trapezius, sternocleidomastoid and sublingual muscles
- Mixed branches: the phrenic nerve, which is the largest nerve plexus. Its motor fibers innervate the diaphragm, and its sensory fibers innervate the pericardium and pleura.
- Brachial plexus
: formed by the anterior branches of the four lower cervical, part of the anterior branch of the fourth cervical and first thoracic SMN. The plexus has supraclavicular (short) and subclavian (long) branches. Short branches innervate the muscles and skin of the chest, all the muscles of the shoulder girdle and the muscles of the back.
The shortest branch is the axillary nerve, which innervates the deltoid muscle, teres minor and the capsule of the shoulder joint. Long branches innervate the skin and muscles of the free upper limb.
- Medial cutaneous nerve of the shoulder
- Medial cutaneous nerve of the forearm
- Musculocutaneous nerve (shoulder flexor muscles and skin of the anterolateral surface of the forearm)
- Median nerve (anterior group of muscles of the forearm, except the flexor carpi ulnaris, on the hand, the muscles of the eminence of the thumb, with the exception of the adductor muscle, 2 lumbrical muscles and the skin of the lateral part of the palm)
- Ulnar nerve (flexor carpi ulnaris, eminence of the little finger, all interosseous, 2 lumbricals, adductor pollicis, and skin of the medial hand)
- The radial nerve is the largest nerve of this plexus (muscles - extensors of the shoulder and forearm, skin of the back of the shoulder and forearm)
- Lumbar plexus
: formed by the anterior branches of the upper 3 lumbar nerves and partly by the anterior branches of the 12 thoracic and 4 lumbar nerves. Located deep in the psoas muscle. Short branches of the plexus innervate the quadratus lumborum muscle, the iliopsoas muscle, the abdominal muscles and the skin of the lower abdominal wall and external genitalia (muscle branches, iliohypogastric and ilio-inguinal and femoral-genital nerves). Long branches innervate the free lower limb.
- Lateral cutaneous nerve of the thigh
- Femoral nerve (anterior thigh muscles and skin over it). The largest nerve of this plexus. Its largest subcutaneous branch is the saphenous nerve (descends along the medial surface of the leg of the foot)
- The obturator nerve descends into the pelvis through the obturator canal, exits onto the medial surface of the thigh and innervates the medial group of thigh muscles, the skin over them and the hip joint.
- sacral plexus
: formed by the anterior branches of the 4th - 5th lumbar nerves and the upper 4th sacral. Located in the pelvic cavity on the anterior surface of the piriformis muscle. Short branches:
- superior gluteal
- inferior gluteal
- sexual
- internal obturator
- pear-shaped
- quadratus femoris nerve
Long branches:
- posterior cutaneous nerve of the thigh
- sciatic nerve
- Both nerves exit through the infrapiriformis foramen, where the posterior cutaneous nerve of the thigh innervates the skin of the perineum, gluteal region and posterior thigh, and the sciatic (the largest in the body) innervates the entire posterior group of thigh muscles. It then splits into 2 branches:
- tibial
- common fibular
The tibial nerve behind the lateral malleolus divides into plantar nerves, and the common peroneal nerve divides into superficial and deep nerves. They come out on the back of the foot. Uniting on the back of the leg, both nerves form the sural nerve, which innervates the skin of the lateral edge of the foot.
- Neuritis – inflammation of the nerve
- Radiculitis – inflammation of the spinal cord roots
- Plexitis – inflammation of the nerve plexus
- Polyneuritis – multiple nerve damage
- Neuralgia – pain along the nerve, not accompanied by dysfunction of the organ
- Causalgia is a burning pain along the nerve that occurs after damage to the nerve trunks
- Lumbago - acute pain that occurs in the lumbar region during physical activity (lifting weights)
- Discogenic radiculopathies are painful motor disorders caused by damage to the spinal cord roots due to spinal osteochondrosis.
- Myelitis - inflammation of the spinal cord
- Epidurit – purulent inflammation of the tissue in the epidural space of the spinal cord
- Syringomyelia is the formation of cavities in the gray matter of the spinal cord
- Poliomyelitis is an acute viral disease characterized by damage to the cells of the anterior horns of the spinal cord and the motor nuclei of the cranial nerves.
Spinal cord membranes
The spinal cord is covered by three membranes:
- soft,
- arachnoid,
- solid.
These membranes pass into similar membranes of the brain.
The inner shell is soft, tightly covers the spinal cord, penetrating into all the cracks and lining them.
The arachnoid membrane is thin, transparent, covering all convexities. Unlike the soft shell, it does not extend into the fissures and grooves of the brain, resulting in the formation of a subarachnoid space filled with cerebrospinal fluid.
The dura mater is the outer shell, forms a dense fibrous sac around the brain, which extends to the roots and ganglia. Below, the hard shell surrounds the cauda equina and, together with the filum terminale, grows to the periosteum of the coccyx.
Connective tissue fibers (22 - 23 pairs) extend from the hard shell, forming jagged ligaments between the hard and soft shells. Thus, it strengthens the spinal cord.
Between the dura mater and the arachnoid membrane, a subdural space is formed, which is filled with cerebrospinal fluid.
The space between the periosteum of the spinal column and the dura mater of the spinal cord is called the epidural. It contains fatty tissue and venous plexuses.
Neural structure of the spinal cord
Sensory cell bodies are located outside the spinal cord. Some of them are located in special ganglia (somatic afferent skeletal muscles), others - in extra- and intramular nodes of the autonomic nervous system. Thanks to them, only the internal organs are sensitive.
Sensitive cells have a process that divides directly near the cell body into two branches: along one, excitation passes from the receptors to the cell body, and along the other, from the neuron body to the nerve cells of the brain or spinal cord. Excitation from one branch to another sometimes occurs without the participation of the neuron body.
In total, the human spinal cord contains about 13 million neurons. Of this total, only about 3% are efferent, motor, or motor neurons, while the remaining 97% are interneurons. Motor neurons are the original cells of the spinal cord. Among them are alpha and gamma motor neurons, as well as preganglionic neurons of the autonomic nervous system.
Neuronal composition of the spinal reflex ring
The receptive fields of various reflexes are not limited, but overlap each other. Different reflexes can be obtained from the same receptive field depending on the strength of stimulation or on the state of the central nervous system. With a constant strength of stimulation and approximately the same functional state of the central nervous system, the same reflex is obtained from a certain receptive field in the body.
When the receptor is stimulated, excitation waves are transmitted in a centripetal direction along the neurite of a neuron located in the spinal intervertebral node, and along the short neural process of the same neuron, which is part of the dorsal roots, they enter the spinal cord. Therefore, the afferent pathway consists of one neuron.
The short neural process of the afferent neuron can come into contact in the spinal cord with the cell body of the efferent motor neuron located in the anterior horn of the spinal cord. The long nerve process of this efferent neuron is part of the anterior roots and then along the mixed nerve reaches the myoneural apparatus, through which the excitation passes to the striated muscle. Consequently, the efferent pathway also consists of one neuron. The entire path along which excitation passes from the receptor or receptive field through the central nervous system into the muscle is referred to as the “reflex arc.”
Schematically, a “reflex arc” consists of at least two neurons. The knee, elbow, Achilles, and other tendon-muscle reflexes are thought to have two-neuron “reflex arcs.” But in most cases, the “reflex arc” consists not of two, but of three or many neurons. The short neural process of the afferent neuron reaches only the posterior horns, where the body of the intercalary, or intermediate, neuron is located, the neural process of which, either on this side or on the opposite side, is in contact with the cell of the efferent neuron of the anterior horns. In a three-neuron "arc", therefore, there are two synapses.
All parts of the "reflex arc" are necessary for the reflex to occur. The reflex cannot be obtained after destruction or poisoning of the skin, i.e. after the receptors are turned off. The reflex is not evoked even after transection of the afferent nerve or after a temporary interruption of its conduction by the action of narcotic substances (cocaine, novocaine, etc.), as well as after destruction of certain segments of the spinal cord involved in the implementation of this reflex. The reflex activity of a certain organ ceases even after the efferent nerves approaching it are cut. However, one should not conclude that under natural conditions the somatic reflex occurs only within one segment of the spinal cord. There are numerous nerve connections between the segments of the spinal cord and due to this, a fairly large number of segments take part in the implementation of the reflex in natural conditions. The higher the development of an animal organism, the more developed its nervous system, the more complex its structure and the greater the connections between its individual parts.
The evolution of the nervous system consists of the formation of nerve centers above the segments of the spinal cord, which have a more complex non-metameric structure, which are called supra-segmental.
Many reflexes involve numerous interneurons with high excitability. The peculiarities of excitation in “reflex arcs” are determined by the complex relationships between receptor and numerous interneurons and motor neurons (for example, transformation of the strength and rhythm of impulses, etc.).
Inhibition is also caused by interneurons. With antidromic stimulation of the anterior root, inhibition of the motor reflex can be caused. This is the result of irritation of special inhibitory interneurons (Renshaw cells) that are located in the anterior horn.
Renshaw neurons are excited by the action of acetylcholine and give antidromic impulses to the motor neurons of the anterior horns of the spinal cord, causing their inhibition (recurrent inhibition). The EPSP of the Renshaw neuron is caused by a single synchronous arrival at the synapse of a volley of presynaptic impulses and after approximately 2 ms it turns into a large trace potential, lasting 50 ms and causing a long rhythmic discharge of impulses. The highest impulse frequency in Renshaw neurons is up to 1500 impulses/s.
The latent period of recurrent inhibition caused by Renshaw neurons varies from 1 to 2 ms. In addition to the direct inhibitory effect on motor neurons, Renshaw neurons also have an inhibitory effect on the synapses of interneurons of the tonic inhibitory pathway leading to motor neurons. When Renshaw neurons inhibit interneurons of the tonic inhibitory pathway, motor neurons are disinhibited and excited.
Recurrent inhibition of motor pyramidal neurons of the brain is caused by special inhibitory widely branching basket neurons, the axons of which end at synapses on the bodies of 200-500 pyramidal neurons, forming a dense plexus around their cell bodies, similar to a basket.
Inhibitory basket neurons are excited directly or through axonal branches of pyramidal neurons, giving a high-frequency discharge (500-1000 impulses/s), causing recurrent inhibition.
Reflex function of the spinal cord (SC)
Note 3
In the study of reflex activity of the brain, an important role is played by the discoveries and generalizations of the British physiologist, Nobel Prize winner Charles Sherrington.
The scope of functions that the SM performs is extremely large. The spinal cord contains centers:
- motor reflexes (except for the muscles of the head),
- reflexes of the rectum and genitourinary system,
- reflexes that provide thermoregulation,
- reflexes that regulate tissue metabolism,
- center of contraction of the diaphragm
- centers of most vascular reflexes, etc.
Under natural conditions, these reflexes are constantly influenced by parts of the brain.
The reflex arcs of spinal reflexes are mono- and polysynaptic.
A detailed analysis of peripheral influences and control of the reflex activity of the spinal cord is carried out thanks to long multi-level reflex arcs, the centers of which are localized in the cerebral cortex and subcortical areas.
The degree of manifestation of the reflex depends on whether the connection between the structures of the spinal cord and the brain is maintained.
Example 1
After decerebralization (removal of the brain) or spinalization (removal of the spinal cord), many complex forms of activity that are provided by the spinal cord disappear. This is explained by a violation of the reflex arcs responsible for carrying out certain reactions. In this case, periodic discharges of the respiratory muscles that provide respiratory movements and tonic discharges of sympathetic neurons that maintain vascular tone and, accordingly, blood pressure may disappear.
SC reflexes include:
- protective,
- vegetative,
- visceromotor (caused by irritation of receptors of internal organs, or changes in their functions),
- stretch reflexes of antagonist muscles.
Note 4
This classification is quite arbitrary, since even in a spinal animal it is difficult to determine reflexes that belong only to one of the named groups.
Conducting function of the spinal cord
Along with reflex activity, an important function of the SC is conduction - the conduction of nerve impulses by white matter (nerve spinal fibers).
Pathways are groups of nerve fibers with a common structure and function that connect the spinal cord and brain, as well as parts of the spinal cord.
Nerve fibers are distinguished according to their functional characteristics:
- associative,
- commissural,
- projection (afferent and efferent).
Thanks to associative fibers, one-way communication is carried out between individual parts of the SM, combining different segments and forming their own bundles.
Commissural fibers unite opposite sections of various parts of the SC, homogeneous in their functions.
Projection fibers connect the SC with the sections located above. With their help, the main pathways are formed, consisting of ascending (centripetal, afferent, sensory) and descending (centrifugal, efferent, motor) pathways.
The ascending pathways of the spinal cord transmit information from receptors that perceive information from the environment and internal environment.
Depending on the type of sensitivity carried out, the pathways are divided into:
- extero-sensitivity (external),
- propriosensitivity (articular-tendon-muscular, tissue mechanoreception),
- interosensitivity (external).
Along the descending pathways of the spinal cord, impulses are transmitted from the structures of the brain to the motor nuclei, and thus appropriate reactions to external and internal stimuli are carried out, that is, the higher parts of the central nervous system communicate with the effector neurons of the spinal cord.
Biology test with answers “Spinal cord and brain” 8th grade
1. The significance of the grooves and convolutions on the surface of the cortex is: a) An increase in the surface area of the cortex + b) An increase in brain volume c) An increase in the activity of cortical neurons
2. Which part of the brain is a continuation of the spinal cord: a) Midbrain b) Medulla + c) Cerebellum
3. The cerebral hemispheres are connected to each other by: a) Vermis b) Brain stem c) Corpus callosum +
4. What regulates and controls the body’s voluntary reactions: a) The cerebral cortex + b) The medulla oblongata c) The parietal lobe of the cerebral hemispheres
5. The cerebral hemispheres first appeared in: a) Fish b) Reptiles c) Amphibians +
6. In what lobe of the cerebral hemispheres are the centers that control vision located: a) In the frontal b) In the occipital + c) In the parietal
7. Coordination of movements and maintenance of skeletal muscle tone is a function of: a) Pons b) Medulla oblongata c) Cerebellum +
8. What is the name of the part of the brain that provides coordination and consistency of movements, as well as body balance: a) Cerebellum + b) Medulla oblongata c) Hypothalamus
9. The centers of thirst, hunger, as well as maintaining the constancy of the internal environment of the body are located in: a) In the cerebellum b) In the midbrain c) Diencephalon +
10. Ganglia are called: a) Two symmetrical halves of the spinal cord b) Nerve ganglia + c) Spinal ganglia
11. Orienting reflexes to visual and auditory impulses are carried out by: a) Midbrain + b) Diencephalon c) Cerebellum
12. What is the spinal cord washed with: a) Spinal fluid b) Cerebrospinal fluid + c) Brain fluid
13. Part of the brain connecting the cortex with the spinal cord: a) Pons + b) Diencephalon c) Cerebellum
14. What are the names of the areas of the cerebral hemispheres that receive information from certain sensory organs: a) Reflexes b) Sections c) Zones +
15. Control centers for the cardiovascular, respiratory and digestive systems are located: a) In the medulla oblongata + b) In the diencephalon c) In the midbrain
16. In what lobe of the cerebral hemispheres are the centers that control muscle movements located: a) In the occipital b) In the frontal + c) In the parietal
17. The most ancient part of the brain in evolutionary terms is: a) Cerebellum b) Cerebellum c) Brainstem +
18. Where does all the information from the senses go: a) To the hypothalamus b) To the thalamus + c) To the right hemisphere
19. The mass of the human brain ranges from: a) From 500 to 1000 g b) From 2000 to 2500 g c) From 1100 to 2000 g +
20. What is a reflex: a) Nervous excitation b) Response to external stimulation + c) Nerve impulse
21. In which sections is thickening of the spinal cord observed: a) In the cervical and lumbar + b) In the lumbar and sacral c) In the thoracic and lumbar
22. Which part of the brain is the spinal cord connected to: a) Forebrain b) Medulla oblongata + c) Diencephalon
23. What reaction (action) of the body with the help of a reflex arc is directly related to the spinal cord: a) Squats b) Eye movements c) Sneezing +
24. Where does the spinal cord end: a) At the level of the first sacral vertebra b) At the level of the first lumbar vertebra + c) At the level of the coccyx
25. What are the ascending pathways: a) Transmission of signals from the brain to organs b) Transmission of signals from the brain to the spinal cord c) Transmission of signals from the spinal cord to the brain +
26. What is a spinal filum: a) Bundles of neuron processes stretching from the spinal cord to the organs b) A narrow process of the spinal cord fused with the periosteum of the coccyx + c) A hollow canal passing through the center of the spinal cord
27. How many pairs of nerve roots extend from the spinal cord: a) 31 + b) 43 c) 19
28. In what sequence are the membranes of the spinal cord located (from the center to the periphery): a) Hard, arachnoid, soft b) Hard, soft, arachnoid c) Soft, arachnoid, hard +
29. What is gray matter: a) Cluster of nerve cells + b) Cluster of myelin fibers c) Cluster of nerve cell processes
30. What fills the space between the spinal canal and the spinal cord: a) Adipose tissue and white matter b) Adipose tissue, blood vessels, cerebrospinal fluid + c) Cerebrospinal fluid, white matter, adipose tissue