Description
Encephalopathy.
A general name for pathological processes of various origins, the basis of which is the degeneration of brain neurons due to disturbances in their metabolism. Encephalopathy is manifested by polymorphic neurological disorders, disorders in the intellectual-mnestic and emotional-volitional spheres. The diagnostic search consists of a comprehensive neurological examination and establishment of the causative pathology. Treatment of encephalopathy comes down to eliminating the pathological condition that caused it, treating the causative disease and maintaining optimal metabolism of cerebral neurons.
How to treat?
Non-drug therapy
Treatment of the disease is aimed at reducing the severity of signs of DEP, improving blood flow and preventing progression.
Since the cause of dyscirculatory encephalopathy is often vascular blockage, one of the methods of combating is to optimize lifestyle:
- eliminating bad habits,
- increased motor activity,
- normalization of nutrition.
An effective treatment method is physiotherapy. For example, UHF, galvanotherapy, therapeutic baths, electrosleep. Systematic courses of physiotherapy have a beneficial effect on the body.
If the blood supply is impaired, the following may be indicated:
- general massage and manual therapy,
- hirudotherapy,
- adequate intellectual load,
- exercise therapy,
- stabilometric training,
- rational psychotherapy.
Treatment with drugs
At stage II, hospitalization is indicated only if DEP occurs against the background of a stroke or other severe somatic disorder. In other cases, treatment is carried out on an outpatient basis.
Treatment is carried out in two directions: improving cerebral circulation and eliminating the root cause.
Therapy aimed at normalizing blood pressure is of great importance.
Getting rid of a hypertensive crisis has a beneficial effect on the reaction of the vascular wall to the composition of the blood, optimizes cerebral blood flow, prevents the progression and re-exacerbation of cerebral circulatory disorders.
Reference! Blood pressure should be maintained at 150-140/80 mmHg.
For hypertension, ACE inhibitors (Fosinopril, Captopril, Enalapril), beta-blockers (Anaprilin, Metoprolol), calcium channel blockers (Diltiazem, Verapamil), diuretics are prescribed, and a salt-free diet is prescribed.
Atherosclerosis is treated with statins (Lovastatin, Lipostat, Simvastatin), anion exchange resins (Gemfibrozil, Cholestyramine), fibrates (Lipanor, Miscleron), unsaturated fatty acids (lipoic acid), antioxidants (vitamin E). A diet excluding animal fats is recommended.
Therapy for thrombosis: antiplatelet agents (Aspirin, Dipyridamole), thrombolytics (Streptokinase, Tenecteplase).
For inflammatory vascular diseases, it is recommended to take glucocorticoids, NSAIDs, ACE inhibitors, and antiplatelet agents.
Specific drug treatment for stage II DEP includes drugs:
- Aimed at improving cerebral blood flow, strengthening connections between neurons, restoring cognitive functions (Piracetam, Ginkgo biloba, Nootropil, Cavinton);
- Stimulating metabolic processes in the brain (Cortexin, Cerebrolysin, Actovegin);
- Protecting neurons from destruction (Cerenton, Gliatilin).
Folk remedies
Traditional medicine methods are effective in combination with drug therapy, non-drug methods and diet.
Important! The use of certain folk remedies must be agreed with a doctor.
The most commonly used herbal decoctions and infusions are:
- Clover infusion;
- Propolis infusion;
- Hawthorn infusion;
- Herbal infusions with chamomile, motherwort, rose hips, mint, lemon balm, valerian and hop cones;
- Onion infusion;
- Fresh onions and garlic;
- Madder roots;
- Roots of marsh cinquefoil;
- Roots of Caucasian hellebore.
The treatment of encephalopathy with folk remedies is described in the video:
Diet
If you have DEP, it is recommended to follow a low-calorie diet.
Products to be excluded:
- high in fat
- fatty meat and fish,
- rich broths,
- spicy, salty, smoked,
- fast food.
https://youtu.be/n3NfdDgSQo4
Additional facts
Encephalopathy is a complex concept that combines numerous syndromes of diffuse cerebral damage, which is based on dysmetabolism and neuronal death. The idea of combining polyetiological cerebral diseases into one group arose in connection with the commonality of their pathogenesis and morphological changes. The term is formed by combining the Greek words “encephalon” - brain and “pathos” - disease. Encephalopathy includes 2 groups of diseases: perinatal and acquired encephalopathy. The concept of perinatal encephalopathy was introduced in 1976 and implies cerebral lesions that occur during the period from the 28th week of pregnancy to the 7th day of life. Perinatal encephalopathy manifests itself in children in the first months of life. Acquired encephalopathy is secondary in nature and is observed mainly in adults, more often in middle-aged and elderly people, in the presence of severe chronic diseases, after injuries, intoxications. Encephalopathy is an interdisciplinary pathology, in accordance with the etiology, requiring attention from specialists in the field of neurology, pediatrics, traumatology, gastroenterology, narcology, cardiology, endocrinology, toxicology, urology.
Encephalopathy
Stages of the disease
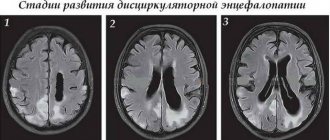
According to the Research Institute of Neurology of the Russian Academy of Medical Sciences, there are 3 stages of dyscirculatory encephalopathy.
Stage I. It is reversible and is characterized by local organic lesions of the brain. Clinical signs are mild, social adaptation is not impaired.
Important! Stage I DEP often occurs in children and young people, but due to subtle signs, diagnosis becomes difficult and can be confused with another disease.
Causes of the disorder:
- lack of healthy sleep,
- unhealthy diet
- violation of the environmental situation,
- insufficient physical activity.
Stage II. Progressive. Motor and mental disorders become more obvious, social and professional adaptation suffers.
The person becomes incapacitated, but is still able to perform the simplest actions for personal care (change clothes, eat, go to the toilet). However, the patient can often injure himself. In this case, it is possible to assign 2 or 3 disability groups.
Causes
Trigger factors that may result in perinatal encephalopathy include: fetal hypoxia, intrauterine infections and intoxications, Rh conflict, asphyxia of the newborn, birth trauma, genetically determined metabolic disorders and developmental abnormalities (for example, congenital heart defects). The risk of perinatal pathology increases with anomalies of labor, a large fetus, premature birth and prematurity of the newborn, a narrow pelvis, and entanglement of the umbilical cord. Acquired encephalopathy can develop as a result of a traumatic brain injury, exposure to ionizing radiation, intoxication with neurotropic chemicals (ethyl alcohol, lead, chloroform, drugs, barbiturates) and bacterial (diphtheria, tetanus, botulism, etc.) toxins. Encephalopathies caused by vascular disorders are widespread: atherosclerosis, arterial hypertension, venous discirculation, angiopathy of cerebral vessels with amylomidosis, leading to chronic cerebral ischemia. A large group consists of encephalopathies associated with exposure to endotoxins and which are a complication of various diseases of somatic organs: acute pancreatitis, acute and chronic renal failure, liver cirrhosis and liver failure. Lung diseases leading to pulmonary ventilation disorders (pneumonia, pulmonary tuberculosis, lung abscess, atelectasis, bronchiectasis, pulmonary embolism) provoke encephalopathy of hypoxic origin. Encephalopathy, observed in a number of patients after resuscitation measures, has a similar genesis. Glucose is important in cerebral metabolism. Encephalopathy can develop both when its level decreases (hypoglycemia) and when it increases (hyperglycemia), which is often observed in diabetes mellitus. The cause of metabolic cerebral disorders is hypovitaminosis (primarily a lack of B vitamins). In some cases, encephalopathy is a consequence of a drop in osmotic pressure and hyponatremia, resulting from water retention due to hypersecretion of antidiuretic hormone (hypothyroidism, adrenal insufficiency, tumor processes, etc.). Rarely encountered is leukoencephalopathy, which has a viral etiology and is observed in immunocompromised patients.
What is DEP?
For the normal functioning of the entire body, it is necessary that every organ, tissue and cell receive a sufficient amount of nutrients and oxygen. They are delivered by the bloodstream.
When the vessels for some reason cannot cope with their work, the supply of nutrients to the tissues is reduced. This may be due to exhaustion, damage, narrowing, clogging of blood vessels with cholesterol and toxins, sudden surges in pressure and other reasons. As a result, first individual cells die, then cell colonies, and in advanced cases, large areas of tissue.
Discirculatory encephalopathy (ICD code 10 - G93.4 - encephalopathy unspecified) is one of the most dangerous consequences of impaired blood flow in the brain.
The danger of the disease is that tissue damage makes it impossible to function. Since each brain structure is responsible for a specific function, it is transferred to the neighboring area. Over time, the healthy part of the brain begins to be unable to cope with a large number of responsibilities, as a result of which vital activity decreases.
Reference! It was previously thought that DEP only occurred in older people. Currently, the disease is rapidly getting younger and can appear as early as 40 years of age. Men are more susceptible to the disease.
It is discirculatory encephalopathy of the 2nd degree that is a fairly common disease of mixed origin, which occurs in 75% of all cases of the disease.
The disease develops in stages, sometimes taking years, and sometimes everything happens in a few months. This especially depends on what part of the brain is damaged.
Experts identify three development options:
- Rapidly progressing, when one stage takes about 2 years;
- Remitting, when symptoms increase more slowly than intelligence decreases;
- Classic - a gradual, slow increase in symptoms up to senile dementia.
So, the disease occurs in several stages:
- Lack of oxygen in cells;
- Cerebrovascular accident;
- Decreased functionality of a part of the brain;
- Violation of vital functions.
The video describes the stages of dyscirculatory encephalopathy:
Classification
In accordance with the etiological factor, encephalopathy is classified into post-traumatic, toxic, metabolic, vascular (dyscirculatory), and radiation. Post-traumatic encephalopathy is a long-term consequence of TBI and can develop several years after it. Toxic variants include alcoholic encephalopathy, observed in chronic alcoholism, as well as cerebral disorders that occur in drug addicts. Metabolic options: hepatic (portosystemic, bilirubin), uremic (azotemic), diabetic, pancreatic, hypoglycemic, hypoxic, anoxic (post-resuscitation) encephalopathy and Gaye-Wernicke syndrome. Discirculatory encephalopathy is divided into atherosclerotic, hypertensive, and venous. Binswanger's disease is a separate form of hypertensive encephalopathy. In clinical practice, a gradation of encephalopathy by severity is used, but this distinction is very arbitrary. I degree of severity implies a subclinical course, i.e., the absence of manifestations in the presence of cerebral changes recorded by instrumental diagnostic methods. At this stage, pathology can be diagnosed during a clinical examination of patients with chronic, primarily vascular, diseases. The presence of mild or moderate neurological symptoms, often transient, characterizes severity level II. In grade III, severe neurological disorders are observed, in most cases causing the patient’s disability.
Clinical symptoms
Manifestations of pathology may be different, depending on the etiology and type, but there are a number of symptoms that are necessarily present in the presence of a cerebrovascular disorder: intense headaches, frequent dizziness, memory disorders, disturbances of consciousness (apathy, persistent depression, desire to die), absent-mindedness and irritability, insomnia. Indifference to others, lack of interests, and difficulty in communication are also noted. Depending on the etiology, emotional disorders, dyspeptic disorders (nausea, vomiting, stool disorders), jaundice, pain in the extremities, obvious weight loss up to cachexia, signs of metabolic disorders (rashes, changes in the skin, swelling) may also be observed.
Symptoms
Chronic encephalopathy is more common, characterized by an asymptomatic onset and gradual development. Most often it is dyscirculatory and post-traumatic in nature. Acute encephalopathy is characterized by a sudden onset and rapid deterioration of the patient's condition, the presence of disturbances of consciousness. It can occur with intoxication and dysmetabolic disorders. Examples are acute pancreatic, uremic, hepatic encephalopathy, Gaye-Wernicke syndrome, hypoxic encephalopathy in PE. Chronic encephalopathy in the early stages is manifested by difficulties when trying to remember recent events or recently acquired information, decreased attentiveness and mental performance, fatigue, sleep disturbance, insufficient flexibility when changing types of activities, and psycho-emotional lability. Patients may experience increased irritability, daytime sleepiness, noise in the head, and headaches that do not have a specific localization. Symptoms may vary between patients. In the neurological status, nystagmus, moderate hyperreflexia and muscle hypertension, the presence of reflexes of oral automatism and foot signs, instability in the Romberg position, discoordination, insufficiency of the cranial nerve (decreased vision, hearing loss, mild ptosis, gaze paresis), signs of autonomic dysfunction are possible. The progression of encephalopathy is accompanied by aggravation of symptoms with the formation of one or another clearly dominant neurological syndrome: vestibulo-atactic, parkinsonian, hyperkinetic, pseudobulbar. An increase in disturbances in the intellectual and emotional-volitional spheres leads to the formation of dementia. Possible mental disorders. Lethargy. Clonic seizures. Myoclonus. Irritability. Absent-mindedness. Vomit. Cramps. Dry mouth. Nausea. Emotional lability.
Types of dysmetabolic encephalopathy
CNS encephalopathy has the following types, each of which is accompanied by separate disorders and symptoms:
- Hepatic form of encephalopathy.
- Uremic form of encephalopathy.
- Pancreatic view.
- Diabetic look.
Let us consider each of these types of disease in more detail.
How does HIV encephalopathy manifest: prognosis for patients.
All about dyscirculatory encephalopathy of the brain: causes, symptoms, treatment.
Hepatic encephalopathy
The hepatic type of encephalopathy (see Hepatic encephalopathy) develops due to serious disturbances in liver function. Most often, this type of disease occurs against the background of cirrhosis of the liver, which was not carefully treated with medication or was not treated at all.
Also, this type of brain damage often occurs due to acute liver failure, hepatitis, various bacterial lesions, as well as poisoning (drugs, toxins from mushrooms, poisons).
This condition is accompanied by serious neurological disruptions and a sharp suffocation of the central nervous system. In this case, it is often difficult for the patient to hold the body in one fixed position. There is also instability when walking (see Impaired coordination of movements), falls, and all kinds of eye dysfunction.
In the initial phase of the disease, a person experiences headaches, muscle weakness, decreased performance and impaired attention. Gradually his condition worsens.
Treatment for hepatic encephalopathy is quite long and complex. In this condition, it is best to undergo a liver transplant, but such an operation requires lengthy preparation and time, which the patient often simply does not have.
As a drug therapy, a person can be prescribed various potent medications:
- Detoxification (electrolyte solutions, glucose).
- Hepatoprotectors (Hepasol A, Heptral, Glutargin).
- Antibiotics (Metronidazole).
- Duphalac (intestinal cleansing).
- Glucocorticosteroids (Dexamthasone).
- Gordox, Etamzilat (for disturbances of homeostasis and coagulation).
- Blood transfusion, plasma, administration of blood substitutes.
Uremic appearance
Uremic or renal encephalopathy occurs due to an acute disruption of the renal system, in particular its filtration functions. This condition occurs due to improper treatment of chronic kidney diseases (pyelonephritis). A kidney transplant in a person can also contribute to its appearance.
Uremic encephalopathy manifests itself in the form of weakness, irritability, nervous excitability and sleep disturbances. As the disease progresses, a person experiences severe pain in the kidney area, which can be sharp, stabbing, pressing or aching. Also characteristic signs of this disease are impaired consciousness and speech, disorientation and headaches.
In the absence of timely treatment, the patient's reflexes are impaired, muscle twitching and convulsions are observed. This condition is especially dangerous for older people, since the functions of their central nervous system can be very quickly depressed and lost.
Pancreatic view
Pancreatic encephalopathy can manifest itself in the form of acute mental agitation, loss of consciousness and even coma. This condition occurs due to the influence of an acute form of pancreatitis, fat embolism, or exacerbation of chronic inflammation of the organ. Encephalopathy is provoked by dangerous enzymes that come out of the affected pancreas.
This disease progresses very quickly. If a person does not begin timely treatment, he may experience impaired speech and motor function, hallucinations and weakness. Also, the patient may not answer questions or respond to people around him.
Read what residual encephalopathy of the brain is: symptoms and treatment.
Find out what encephalopathy in a newborn is and where it comes from.
Everything about toxic encephalopathy of the brain: causes, signs, assessment of work capacity.
Diagnostics
The primary diagnosis of encephalopathy is carried out by a neurologist based on the results of a survey and neurological examination. Additionally, a comprehensive instrumental neurological examination is carried out: electroencephalography, echoencephalography, rheoencephalography or ultrasound of the vessels of the head. EEG, as a rule, reveals diffuse disorganization of the bioelectrical activity of the brain with the appearance of slow waves. Epi-activity can be detected. Echo-EG allows you to assess intracranial pressure. Vascular studies provide information about the state of cerebral circulation. The degree of morphological changes can be analyzed using MRI of the brain. This method also makes it possible to differentiate encephalopathy from other cerebral diseases: Alzheimer's disease, intracerebral tumor, encephalitis, disseminated encephalomyelitis, stroke, corticobasal degeneration, Creutzfeldt-Jakob disease, etc. The most important in understanding the etiology of encephalopathy is the collection of anamnesis, examination of somatic organs and consultations of related specialists: cardiologist, nephrologist, gastroenterologist, endocrinologist, pulmonologist, narcologist. According to indications, hormonal studies, determination of cholesterol and blood sugar levels, urine analysis, biochemistry of blood and urine, ultrasound of the liver, ultrasound of the pancreas, excretory urography, ultrasound of the urinary system, CT of the kidneys, chest radiography, CT of the lungs are carried out.
Treatment
Acute encephalopathy is an indication for urgent hospitalization and urgent therapy. It may require measures such as mechanical ventilation, hemodialysis, parenteral nutrition. In the treatment of both acute and chronic encephalopathy, the leading place belongs to the treatment of the causative disease. In case of intoxication, detoxification is carried out, including administration of infusion solutions; for dysmetabolic disorders - correction of metabolism (selection of the dose of glucose-lowering drugs or insulin, administration of glucose solution, intravenous administration of thiamine). Treatment of hepatitis, cirrhosis, pancreatitis, nephritis, lung diseases, hypertension, atherosclerosis is provided. It is recommended to follow a diet corresponding to the underlying pathology and a regimen adequate to the patient’s condition. The presence of an ischemic component in the pathogenesis of encephalopathy is an indication for vascular therapy: pentoxifylline, ticlopidine, vinpocetine, nicergoline. Atherosclerotic encephalopathy requires the inclusion of lipid-lowering pharmaceuticals (for example, simvastatin, gemfibrozil) in the treatment regimen. Therapy for hypertensive encephalopathy is carried out with the prescription of antihypertensive drugs and monitoring of blood pressure numbers. If dyscirculatory encephalopathy is caused by occlusion of the carotid arteries or vertebral artery, surgical treatment is possible: reconstruction or prosthetics of the vertebral artery, carotid endarterectomy, carotid-subclavian bypass, creation of extra-intracranial anastomosis. Neuroprotective and metabolic therapy is mandatory. It includes nootropics (hopanthenic acid, piracetam, pyritinol, lucetam), amino acids (glycine, glutamic acid), vitamins (B1, B6, C, E), GABA preparations (picamilon, phenibut). For mental disorders, psychotropic drugs are needed: diazepam, bromides, droperidol, phenozepam. For seizures, anticonvulsant therapy is carried out; nootropics are contraindicated. Pharmacotherapy is carried out in repeated courses 2-3 times a year. Physiotherapy methods are used as an auxiliary treatment: reflexology, electrophoresis, magnetic therapy.
Forecast
In many cases, the prognosis of secondary encephalopathy determines how effectively the causative pathology can be treated. The outcome of therapy also depends on the degree of cerebral changes that have occurred. In some cases, stabilization of encephalopathy is considered a positive effect. With further progression, encephalopathy reaches stage III and leads to severe neurological and emotional-mental disorders that disable the patient. In the case of perinatal or acute encephalopathy, the outcome depends on the massiveness and severity of damage to brain tissue. Often, acute toxic encephalopathies are accompanied by deep and irreversible brain damage.
Assignment of disability
With DEP, social adaptation, motor and cognitive components are impaired, so it is necessary to assign a disability. The group depends on the severity of the disease and can be assigned at stages II and III.
Reference! At stage II of dyscirculatory encephalopathy, work that requires adequate situational behavior, precise coordinated movements, prolonged walking and with neuropsychic stress is prohibited.
In what cases is it necessary to contact the Bureau of Medical and Social Expertise to establish disability?
- Contraindicated types and working conditions;
- Rapidly developing disease;
- Inability to carry out professional activities, frequent exacerbations and signs of dementia.
Prevention
Prevention of perinatal encephalopathy is a matter of correct choice of method of delivery, adequate management of pregnancy, and compliance with the rules of care for the newborn. Prevention of secondary encephalopathy consists of timely detection and adequate treatment of vascular, urological, gastroenterological diseases, pulmonary pathology, endocrine and metabolic disorders. Proper nutrition, an active lifestyle, and quitting smoking, drugs and alcohol can be considered as preventive measures.