Definition of the concept
The human nervous system consists of a central section, including the brain and spinal cord, and a peripheral section - motor, sensory, and autonomic fibers.
Any order from the brain in the form of an electrical impulse begins its journey in the convolutions of the cortex, then along the conducting paths it arrives at the second point - a cluster of motor nuclei of nerve cells. Through the fibers of these structures that form the nerves, the impulse arrives at its destination - the skeletal muscles.
Most cranial nerve centers are located in the medulla oblongata.
The muscles of the trunk and limbs have their own motor nuclei at different levels of the spinal cord. The muscles of the head and neck are controlled by clusters of nerve cells located in the most ancient formation of the central nervous system - the medulla oblongata. Paired motor centers that control hearing, facial and oculomotor muscles, muscles of the tongue, pharynx, neck and upper shoulder girdle are concentrated in a small area. These nerve cells make up the nuclei of the cranial nerves and are designated by Roman numerals from one to twelve. In close proximity there are centers that control breathing and blood movement through the vessels.
Cranial nerves control the muscles of the face, neck, eyes, tongue
Bulbar syndrome is a medical term denoting a combined lesion of the nuclei of the ninth, tenth, twelfth pairs of cranial nerves and their motor pathways.
Synonyms of the disease: bulbar palsy, bulbar paresis, bulbar disorder syndrome.
In bulbar syndrome, peripheral paralysis occurs, in which the nerve impulse is blocked at the level of the cranial nuclei or subsequent motor fibers of the nerve . When the source of impulses in the cortex or its pathways is damaged, a largely different condition is formed - central palsy of the ninth, tenth and twelfth cranial nerves, called pseudobulbar syndrome. The clinical picture in this situation will differ in many ways.
Differences between bulbar and pseudobulbar syndrome - table
| Type of paralysis | Pseudobulbar=central palsy | Bulbar=peripheral paralysis |
| Damage level | Central motor neuron:
| Peripheral motor neuron:
|
| Symptoms | Triad of symptoms:
| |
| Atrophy of the tongue muscles, drooping soft palate | Characteristic | Not typical |
| Reflex raising of the soft palate in response to a stimulus | Enhanced | Weakened |
| Violent laughter, crying | Characteristic | Not typical |
| Reflex contraction of the mouth muscles in response to a stimulus | Characteristic | Not typical |
Drug therapy
The diagnosis of bulbar palsy is an indication for taking the following medications:
- artificial cholinesterase inhibitors (Proserin) improve swallowing function, restore gastric motility, and also normalize blood pressure;
- antibacterial agents help stop the development of infection;
- diuretics (Furosemide, Torasemide) eliminate swelling of the soft tissues of the brain;
- medications containing glutamic acid restore metabolic processes that are responsible for the functioning of the central nervous system;
- vasoactive agents (Parmidin, Alprostan) are taken by patients with disorders of the vascular system;
- Group M cholinergic receptor blockers (Atropine) are indicated for use in patients who suffer from excessive salivation.
Damage to the cranial nerves is also an indication for taking medications that contain vitamin B, thereby speeding up the recovery of the central nervous system. Such medications include the drugs Neuromultivit and Vitagamma.
Classification
Bulbar palsy is classified into three main types:
- acute paralysis, developing rapidly against the background of some catastrophe in the brain: infectious lesion or acute circulatory disorder;
- progressive paralysis, which is a natural component of degenerative diseases of the nervous system;
- alternating syndrome, in which damage to the bulbar nuclei is combined with damage to the muscles of half the body.
Bulbar syndrome can be acute and progressive
Symptoms
The symptoms of bulbar palsy are quite specific, and unlike the pseudobulbar type, the disease can lead to cardiac or respiratory arrest.
The main symptom of this disease is difficulty in the swallowing reflex, which can lead to increased uncontrolled salivation in the patient.
In addition, the disease is characterized by:
- violation of speech functions;
- difficulty chewing food;
- twitching of the tongue, in case of paralysis;
- protruding tongue located in the throat in the direction opposite to paralysis;
- sagging upper palate;
- phonation disorder;
Phonation – using the larynx to produce sounds
- arrhythmia;
- violation of the respiratory and cardiac functions of the body.
Infectious bulbar palsy is similar to pseudobulbar palsy in many symptoms, however, with the second type of disease there is no arrest of cardiac and respiratory activity. Also, no tongue twitching was noted during tongue paralysis.
Causes and factors for the development of paralysis
With bulbar syndrome, the pathological process affects the nuclei of three pairs of cranial nerves. The ninth pair (glossopharyngeal) is responsible for conducting nerve signals to the muscles of the tongue and pharynx, and also provides the perception of taste sensations from the back third of the tongue. The tenth pair (vagus nerve) transmits signals to the muscles of the larynx, salivary glands and other internal organs located in the chest and abdominal cavity. The twelfth pair (hypoglossal nerve) controls the muscles of the tongue.
Peripheral paralysis of these nerves is characterized by a triad of symptoms: a decrease in muscle strength and tone in the form of paresis or paralysis, muscle atrophy and convulsive contractions of individual muscle fibers (fascicular twitching).
The nuclei of the cranial nerves of the bulbar group can suffer as a result of various pathological processes.
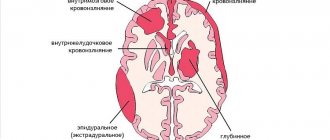
Bulbar syndrome often occurs as a consequence of cerebrovascular accident. Disruption of blood flow in the central nervous system is, as a rule, in the nature of hemorrhage or ischemia due to blockage of blood vessels by atherosclerotic plaques. A large volume of blood leaking into the cranial cavity inevitably leads to compression of adjacent structures in a confined space. Nerve cells are also very sensitive to a lack of oxygen, so even a short episode of reduced blood flow in the vessels can cause damage.
Stroke is a common cause of bulbar syndrome
Clinical aspects of hemorrhagic stroke - video
The tumor process can also affect the bulbar group of cranial nerve nuclei. A malignant neoplasm can be primary in nature and have nerve cells of the medulla oblongata as its source. In another case, the primary tumor is located in another organ, and the nuclei of the cranial nerves are affected by secondary foci of the process - metastases.
A brain tumor can cause destruction or compression of the bulbar centers
The formation of edema of the gray and white matter against the background of various pathological processes can lead to herniation of the medulla oblongata into the lumen of the adjacent round bone formation - the foramen magnum. This event is extremely dangerous due to damage not only to the nuclei of the cranial nerves, but also to the respiratory and vasomotor centers.
Traumatic brain injury can also cause the development of bulbar syndrome. A fracture of the bones of the base of the skull leads to swelling, compression and damage to the fragile nerve fibers of the cranial nuclei by fragments.
Fracture of the base of the skull is a traumatic cause of the development of bulbar syndrome
The cause of bulbar syndrome can also be inflammation of the substance and membranes of the brain of an infectious nature. Such a process inevitably leads to swelling of brain structures, including the nuclei of the cranial nerves. These diseases include tick-borne encephalitis, polio, meningococcal meningitis, enteroviral meningitis, diphtheria, syphilis, and HIV infection. In addition, nerve cells suffer due to pathogen toxins released into the blood. One such substance is botulinum toxin, secreted by the bacterium C. Botulinum.
An infectious agent can cause damage to the bulbar nuclei
Degenerative processes in the brain substance can also cause bulbar syndrome. These diseases lead either to diffuse damage to nerve cells or affect a specific substance - myelin, which forms their surface sheath. Similar pathologies include amyotrophic lateral sclerosis, Kennedy bulbar amyotrophy, Werdnig-Hoffmann spinal amyotrophy, and motor neuron disease.
Chronic progressive diseases of the nervous system can cause the development of bulbar syndrome
ALS: what is the disease, what are the symptoms and how to treat?
- Genetic.
- Degenerative.
- Infectious.
As a rule, Bulbar palsy and pseudobulbar palsy develop as a result of one or another disease, and depending on this, the above division occurs. For example, Kennedy amyatrophy is a genetic disease that results in this disease.
What does a twisted tongue look like during paralysis?
In turn, diseases such as Guyet Barre syndrome, Lyme disease or polio act as degenerative causes.
Important! People who have had to deal with such a phenomenon as ischemic stroke (transient disturbance of cerebral circulation) are at risk of acquiring infectious bulbar paralysis.
If with adults everything is more or less clear, then with young children not everything is as clear as it seems.
Thus, in young children it is difficult to diagnose the disease based on the main symptom - increased salivation as a result of a difficult swallowing reflex. Every 3 children experience such a symptom, not because there is pathology, but because of the characteristics of the child’s body.
How to recognize an illness in a child? To do this, you need to examine the baby’s oral cavity and pay attention to the position of the tongue. If it is unnaturally shifted to the side or there is twitching, it makes sense to contact a specialist for a thorough analysis.
In addition, a sick child may experience partial facial paralysis, which manifests itself in the absence of changes in the baby’s facial expressions.
Diagnosis of this disease does not include a huge number of tests and instrumental treatment methods. The basis is an external examination of the patient by a specialist, as well as a procedure such as electromyography.
Based on the data obtained, the doctor makes a conclusion and prescribes treatment.
In some cases, urgent assistance is necessary to save life with bulbar syndrome.
The main goal of this assistance is to neutralize the threat to the patient’s life. before being taken to a medical facility, where treatment will then be determined and prescribed.
The doctor, in accordance with the symptoms and nature of the disorder, can predict the outcome of the disease, as well as the effectiveness of the prescribed treatment for bulbar syndrome, which is carried out in stages, namely:
- resuscitation, support of body functions that were impaired due to the disorder - restoration of breathing, activation of the swallowing reflex, reduction of salivation;
- This is followed by treatment of manifestations aimed at alleviating the patient;
- treatment of the disease that caused the syndrome;
- Patients are fed using a feeding tube.
The photo shows special gymnastics for bulbar syndrome
Good results are achieved in the treatment of pseudobulbar syndrome using stem cells.
Their administration to a patient with pseudobulbar disorder leads to the fact that they replace functionally affected cells. As a result, the person begins to live normally.
It is quite important to carefully monitor the oral cavity in case of pseudobulbar and bulbar syndromes. and also, if necessary, monitor the patient while eating so that he does not suffocate.
Amyotrophic lateral sclerosis (Charcot's disease, motor neuron disease, ALS) is a fairly rare disease of the nervous system, when a person develops muscle atrophy and weakness, which progresses further and leads to death.
With the development of this disease, degeneration of the peripheral and central neurons of the main pathway of the nervous system occurs. In this case, some elements are replaced by glia. The pyramidal fasciculus is usually affected much more severely in the lateral columns. Hence the epithet – lateral. As for the peripheral neuron, it is very strongly affected in the area of the anterior horns.
That is why the disease is accompanied by another epithet – amyotrophic. Moreover, the name accurately emphasizes one of the clinical signs of the disease – muscle atrophy. ALS syndrome is a fairly serious disease. It is worth noting that the name that Charcot gave to the disease maximally reflects all its characteristic features: symptoms of damage to the pyramidal fasciculus, located in the lateral column, are combined with muscle atrophy.
Clinical picture
Bulbar palsy is characterized by a triad of clinical signs in the form of articulation, voice and swallowing disorders.
Voice disorder (dysphonia) is characterized by a change in voice timbre and the appearance of a nasal sound. The cause of the first sign is non-closure of the glottis due to paresis of the laryngeal muscles. Nasality (rhinolalia) is caused by the immobility of the soft palate.
Vocal fold paresis is a consequence of damage to the vagus nerve nucleus
Articulation disorder (diasarthria) is a consequence of damage to the motor activity of the tongue muscles. The patient's speech in this situation becomes slurred or impossible.
Swallowing impairment (dysphagia) is a consequence of damage to the glossopharyngeal nerve. The brain is unable to control the act of swallowing. The consequence of this process is choking when taking liquid food and getting it into the nasal cavity.
The patient’s appearance is also very characteristic: there is no lively facial expression on the face, the mouth is slightly open, saliva flows from the corner of the mouth, since the brain, through the vagus nerve, is not able to control salivation. The tongue, as a rule, is noticeably reduced in volume on the affected side and deviated from the midline.
Deviation of the tongue from the midline is a typical sign of bulbar syndrome
The most severe consequence of the pathological process in the group of bulbar nuclei of the cranial nerves is respiratory failure and cardiac dysfunction.
Diagnostics
Diagnosis and treatment of bulbar palsy is carried out by specialists in the field of neurology. Diagnostic measures are aimed at identifying the immediate cause of the pathology and consist of examining the patient, identifying all the symptoms of the disease and conducting electromyography. The obtained clinical data and research results make it possible to determine the severity of paralysis and prescribe treatment. These are mandatory diagnostic techniques, which are supplemented by a general blood and urine test, brain tomography, esophagoscopy, cerebrospinal fluid examination, electrocardiography, and consultation with an ophthalmologist.
During the first neurological examination, the patient’s neurological status is determined: speech intelligibility, voice timbre, salivation, swallowing reflex. Be sure to study the appearance of the tongue, identify atrophies and fasciculations, and evaluate its mobility. Assessment of respiratory rate and heart rate is of important diagnostic importance.
Then the patient is sent for additional diagnostic examination.
- Using a laryngoscope, the larynx is examined and sagging of the vocal cord on the affected side is detected.
- X-ray of the skull - determination of bone structure, the presence of fractures, injuries, neoplasms, areas of hemorrhage.
- Electromyography is a research method that evaluates the bioelectrical activity of muscles and allows one to determine the peripheral nature of paralysis.
- Computed tomography is the most accurate images of any part of the body and internal organs, made using X-rays.
- Esophagoscopy - determining the functioning of the muscles of the pharynx and vocal cords by examining their inner surface using an esophagoscope.
- Electrocardiography is the simplest, most accessible and informative method for diagnosing heart disease.
- MRI - layer-by-layer images of any area of the body, allowing you to study the structure of a particular organ as accurately as possible.
- Laboratory tests show characteristic changes: in the cerebrospinal fluid - signs of infection or hemorrhage, in the hemogram - inflammation, in the immunogram - specific antibodies.
Complications and prognosis
The prognosis for treatment of bulbar syndrome largely depends on the underlying disease that caused the pathological condition. If the damage to the nuclei of the cranial nerves is infectious, a complete recovery is possible. The prognosis for hemorrhage is unfavorable in half of the cases. In degenerative diseases of the nervous system, bulbar palsy is progressive.
In severe cases, the following complications may develop:
- cerebral edema;
- cerebral coma;
- breathing disorders, including those requiring artificial ventilation;
- traumatic epilepsy;
- complete inability to swallow food independently and use feeding through a feeding tube.
Necessary diagnostic tests
Bulbar syndrome is not an independent disease. Therefore, confirming the presence of a problem comes down to identifying the cause of its occurrence, as well as establishing the nature of the pathological disorders. For this purpose, standard diagnostic tests are carried out - blood, urine and stool tests, as well as a general examination of the patient and medical history.
In many cases, the use of visual methods is required, in particular, magnetic resonance imaging, which makes it possible to detect the presence of tumor and ischemic processes in the cranial cavity. Electromyography, used to differentiate central and peripheral paralysis, is also informative.
Prevention
Prevention of bulbar syndrome includes the following measures:
- timely vaccination prevention of infectious diseases;
Vaccine prevention is a way to avoid bulbar syndrome of an infectious nature
- adequate treatment of atherosclerosis and hypertension;
- adequate treatment of diabetes mellitus;
- timely diagnosis of tumor processes;
- proper nutrition;
- feasible physical activity.
Adequate physical activity is an integral part of a healthy lifestyle.