Benign paroxysmal positional vertigo (BPPV)
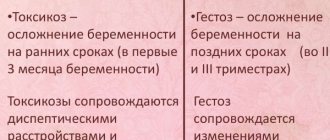
–
a disease of the inner ear
, manifested by short-term dizziness that occurs when the position of the head (body) changes.
Most often, dizziness
occurs in the morning after sleep or at night when turning over in bed.
According to a number of researchers, the probability of developing the disease during a lifetime is about 10%. The average duration of the disease is about two weeks; in some cases, the patient reports only 1-2 episodes of dizziness
, less common are patients suffering from
positional vertigo
for up to 1 year or more.
Symptoms of benign paroxysmal positional vertigo
The human vestibular apparatus is located in the inner ear and is a system of semicircular canals located in three planes and filled with fluid. There, in the channels, there are sensory cells, information from which is transmitted to the vestibular nerve. With any of our movements, fluid moves in one or more channels, this movement is captured by sensitive cells, and information is transmitted along the vestibular nerve to the brain.
With the development of BPPV
Calcium carbonate crystals (otoliths) accumulate in one of the canals.
When the head moves, for example, when throwing back or turning over in bed, the clot of otoliths in the canal begins to move and irritate the sensory cells, causing a feeling of dizziness
.
The symptoms of dizziness
most clearly in the morning or after prolonged exposure to a constant position, because... in this case, the crystals form a fairly large and dense clot. Over the course of the day, the clot usually dissipates somewhat and the symptoms subside.
Diagnosis of BPPV
When contacting a neurologist, a medical history is taken and a series of specific tests are performed. The diagnosis of benign paroxysmal positional vertigo is made primarily on the basis of clinical data. To confirm it, the doctor performs the Dix-Hallpike test.
The person being tested, sitting on the couch and turning his head to the affected side (the angle of rotation should be 45⁰), fixes his gaze on the bridge of the nose of the person conducting the test. Then you quickly need to lay him down on his back so that the fixed head hangs down slightly.
After 20 seconds, return to its original state, repeat on the other side and evaluate the result:
- If after 1-5 seconds in a lying position the patient becomes dizzy and rotatory nystagmus (rotation of the eyeballs) occurs, BPPV is diagnosed. When returning to the starting position, the eyes move in the opposite direction.
- The absence of both symptoms indicates that the test is negative.
- A positive bilateral result indicates a traumatic origin of the pathology.
- Dizziness without nystagmus is confirmation of the diagnosis, but with the prefix “subjective”.
If the test is repeated several times in a row, the accumulation of otoliths that irritate the ciliated cells will dissipate. Accordingly, the head will no longer feel dizzy when tilted, and the nystagmus will be exhausted. To fix the latter during diagnostics, special techniques are used. Electronystagmography or videooculography. Recording equipment is needed because eye movements during the Dix-Hallpike test cannot always be recorded visually.
For reference. To further confirm benign paroxysmal positional vertigo, a so-called rotation test is performed.
The patient, lying on his back, throws his head back at an angle of 30⁰. The doctor sharply turns it to the affected side and observes the horizontal nystagmus that occurs after a short latent interval.
By the nature, speed and direction of movement of the eyeballs, one can determine the localization of otoliths, and in the case of canalolithiasis, in which particular canal the accumulation of otoliths is located.
The main symptoms of BPPV are characteristic of some other vestibular disorders, diseases of the nervous and cardiovascular systems. Differential diagnosis is required if vestibular neuronitis, multiple sclerosis, Meniere's disease, arterial hypotension, Barré-Lieu and vertebral artery syndromes are suspected. With these pathologies, in addition to dizziness, hearing loss, neurological disorders, tinnitus, cephalalgia, and neck pain are also observed.
Treatment of BPPV
Treatment of BPPV
consists of performing a so-called positional maneuver, the purpose of which is to move the calcium carbonate crystals from the semicircular canal to the vestibule of the labyrinth, where they will no longer cause
dizziness
.
During this procedure, the doctor performs a series of sequential movements of the patient's head and body. When performed correctly, the maneuvers are very effective: after the first procedure, complete cure is achieved in 80-90%. Your doctor may also recommend performing special exercises at home. With adequate exercise, most patients experience relief of symptoms within a few days. In some cases, spontaneous recovery is possible due to the dissolution of the crystals or the spontaneous movement of the crystals back into the vestibule of the labyrinth.
BPPV - what is it?
BPPV is, as stated above, an abbreviation for the term “benign paroxysmal positional vertigo.” An attack of this type of dizziness is associated with a change in the position in space of the body and head. However, it differs from, for example, orthostatic collapse in the duration and condition after the attack.
For reference. That is, BPPV is a short-term vestibular disorder observed when turning the head.
It is accompanied by nausea, and in some cases, vomiting. The cause of the pathology is the presence of freely floating otoliths (crystallized calcium bicarbonate) in the endolymph. Their displacement causes irritation of the ciliated cells and, accordingly, dizziness.
For diagnostic purposes, special tests are used, and for therapeutic purposes, vestibular gymnastics, Epley and Semont maneuvers are used. The effectiveness of drug therapy has not been proven, so prescribing medications is advisable only as an adjunct.
Diagnosis of the cause of dizziness
A detailed history of your medical condition is the most important information your doctor needs to diagnose the cause of your vestibular disorder and then administer appropriate ART.
The doctor will ask you to describe your vestibular symptoms in detail. Any symptoms you experience above or others should be mentioned. Your doctor will want to know when the first episode of your symptoms occurred, how long they lasted, and whether they were related to any other events, such as a car accident, head injury, illness, or infection.
He will also want to know how often symptoms have recurred since the first episode and the general pattern of symptom frequency. Find out exactly what causes your symptoms, such as moving your head in a certain direction or getting out of bed. For dizziness, your doctor will ask about the nature of what you're feeling and whether you experience episodes of true dizziness where you have a spinning sensation.
The doctor will also want to know if there is anything that reduces or increases your symptoms, and if you are taking any medications, or if you have a family history of any inner ear disorders or central nervous system disorders.
He may ask you to rate the intensity of some of your symptoms on an objective scale. Finally, they will ask about all the daily activities that are related to your vestibular problem, such as walking, driving, working, and even household activities such as dressing, bathing, showering, and housekeeping.
He will also want to know if you have any falls.
The doctor will examine your eye movements by asking you to follow certain objects with your eyes or by asking you to move your head while keeping your attention on a specific target.
An examination of the joints and neck muscles is also carried out to determine the cervicogenic nature of dizziness.
Finally, your doctor may ask you to fill out a questionnaire to determine the intensity of your vestibular symptoms.
Depending on what the doctor finds during the initial examination, they may send you for a series of other tests to further determine the cause of your vestibular symptoms.
Vestibular rehabilitation
As stated above, ART can be used to treat various disorders that cause dizziness or balance problems. Almost any disorder that occurs due to vestibular dysfunction and does not receive sufficient compensation can be treated with ART. The effectiveness of ART depends on correct diagnosis of the cause of the imbalance, the skill/training of the therapist in developing and administering the treatment, and adherence to the prescribed exercise program.
As explained earlier, the purpose of ART exercises is to encourage the brain and spinal cord to compensate for any balance deficits that arise due to diseases or abnormalities of the inner ear or central nervous system. In other words, patients teach their vestibular system to do one of several things; adapt to the stimuli presented, substitute other sensory pathways, or become accustomed to changing vestibular signals sent to their brain so that they can manage their vestibular disorder and maintain normal functioning despite possible ongoing symptoms.
In some cases, ART can eliminate vestibular symptoms. Unfortunately, however, this is not always the case, so minimizing symptoms or the frequency of recurrence of symptoms is considered a successful outcome of ART.
Research in the field of ART shows that, in general, ART exercises are effective in reducing many symptoms of vestibular disorder and that these improvements can often persist for several months after therapy. However, the effectiveness of therapy often depends heavily on what exactly is causing the vestibular symptoms in the first place and the use of individualized exercises rather than a standard exercise protocol.
ART, however, is not always effective for all vestibular problems. There are even some vestibular problems where exercise is not considered appropriate, so proper diagnosis of the cause of the symptoms is important.
ART exercises
If your physiotherapist feels that ART is right for you after completing your assessment, they will prescribe a range of individual exercises for you to do regularly. These exercises will focus on your specific vestibular problem and associated symptoms.
Additionally, the exercises you are prescribed will focus on any day-to-day problems you are facing as a result of your symptoms. Some exercises will be done with your physical therapist on a stability platform, and others will be retrained so that you can do them on your own as part of a home exercise program.
Medications to treat your symptoms may be an addition to ART and should be discussed with your doctor.
Types of BPPV
The anomaly can occur in any ear, so both right-sided and left-sided vertigo are distinguished. Since the localization locations of moving particles of the otolith membrane can be different, otolithiasis is divided into the following forms:
- Cupulolithiasis. The fragments are fixed on the cupula. This placement causes constant irritation of the ear receptors.
- Canalolithiasis. Otoliths move freely through the endolymph in the canal cavity. Changing the position of the head leads to the development of an attack.
When making a diagnosis, doctors must indicate the side of the lesion, as well as the semicircular canal - posterior, anterior or external - where the pathology was detected.
Warn and do no harm
The following measures can be taken to prevent the development of BPPV:
- prevention of damage to the balance organ by viral and other infectious agents;
- caution when performing work and other vital functions;
- careful attention to the use of medications;
- prevention of vascular disorders in the head and neck area.
The prognosis depends on the severity of concomitant pathology. The disease can become dangerous when the patient is at a significant altitude or depth with associated changes in atmospheric pressure, as well as in the event of a seizure developing in the operator of the mechanisms.
Mechanics of the disease and its causes
Preventive measures for benign positional paroxysmal vertigo have not been developed to date since the etiological factors in the development of the disease have not been fully elucidated.
As a recommendation, patients should not drive a car for some time.
The pathological condition may persist for several days or weeks after treatment. As for the restoration of ability to work, it can also be difficult for several weeks, but one should take into account the fact that benign positional vertigo can recur over time and when such a moment occurs is not known.
The “Christmas ball” helps to understand benign positional vertigo - when shaken, a “blizzard” of small sparkles rises in the liquid that fills it.
With BPPV, a similar condition occurs when changing the position of the head or shaking it.
The otoliths, which remain in place, react quickly and adequately to the emerging “wave”. But the broken off otoliths form a suspension in the endolymph, firstly, thickening it and lengthening the “wave” time, and secondly, they distort the reflex.
The most accessible channel for the accumulation of such “junk” is the posterior canal (aka vertical), which has the lowest bottom both when the head is in a horizontal position and when it is in a vertical position.
While the “blizzard” of otolith debris is swirling, the manifestations of the syndrome are maximum; as the “garbage” settles, everything subsides.
In a large percentage of cases, the basis for the occurrence of the phenomenon of otolithiasis—the accumulation of “fallen” otoliths-statoliths in the cavities of the labyrinth—has not been identified.
Causes that can cause benign paroxysmal positional vertigo:
- TBI ( traumatic brain injury);
- viral labyrinthitis;
- Meniere's disease;
- ototoxicity of medications;
- migraines due to NCD (with spasm of the labyrinthine artery);
- surgery on the ear or brain.
Folk remedies
Toning infusions of lemongrass, mint or lemon balm will help reduce signs of dizziness. A collection of clover, hawthorn and sage flowers effectively smoothes out attacks of faintness. You can also mix essential oils: camphor (10 drops), fir (3 drops) and juniper (1 drop). Rub the resulting mixture into the temple area. A few spoons of pomegranate or grape juice will help relieve nausea.
Rubbing will help relieve the condition:
- earlobes;
- fingertips, starting with the little finger;
- the upper edge of the eyebrow arches;
- areas between the nose and lip.
Cholesteatoma of the ear
Diagnosis of cholesteatoma of the ear
To diagnose cholesteatoma of the ear, you will need to consult not only an otolaryngologist, but also a neurologist and neurosurgeon.
Radiography
To identify and study cholesteatoma of the ear, a number of tests are performed. Traces of cholesteatoma of the ear can often be detected by skull radiography. On radiographs, cholesteatoma stands out as a homogeneous shadow containing medium density; it is located in a round pathological cavity with smooth, distinguishable edges. This image helps the specialist determine the size and location of the cholesteatoma.
CT scan
Computed tomography is also sometimes used, with its help the doctor obtains three-dimensional images of cholesteatoma. For the least amount of radiation, the patient undergoes one of the procedures, X-ray or computed tomography.
MRI
Another effective analysis is MRI with a contrast agent. MRI does not irradiate the patient, but it creates a three-dimensional image of cholesteatoma. The introduction of a contrast agent into the body before the procedure allows you to obtain good quality images of soft tissues. During this analysis, the size, shape of the formation and defects in adjacent ear structures are revealed.
Audiometry
Audiometry reveals the level of hearing loss. An analysis is carried out with a tuning fork, this analysis determines the patency of the auditory tube, electrocochleography, acoustic impedance measurement, otoacoustic emission, vestibulometry, electronystagmography, stabilography. Using special headphones, sounds of different frequencies and intensities are passed through them; based on the indicators, the doctor identifies the degree of hearing impairment in the patient.
Tympanometry
The tympanometry method evaluates the mobility of the eardrum, which makes it possible to exclude the presence of liquid matter in the middle ear. When performing otoscopy, it becomes possible to determine perforation of the edges in the eardrum and signs of destruction of the bone parts of the ear canal, with the growth of cholesteatoma. Detection of marginal perforation leads to probing of the middle ear cavity with a button probe and rinsing of the supratympanic area. If there is a destructive process, the surface of the bone will be rough when examined with fingers. Also, the presence of cholesteatoma of the ear will be indicated by the presence of epidermal scales in the washing substance.
Additional tests for a patient with cholesteatoma of the ear will include hearing and vestibular analyzer studies. Ear cholesteatoma can be confused with tumors and other foreign components of the ear, cochlear neuritis, cerumen plug, glomus tumor, adhesive otitis media, specific granulomas in tuberculosis or syphilis, for which a number of the above studies are carried out.