The consequences of a stroke are varied. Disruption of blood flow in the vessels of the brain can result in minor damage to neurons with subsequent recovery. But a tragic outcome is also possible in severe stroke, when the focus of necrosis is extensive, vital centers are affected, or a pronounced displacement of brain structures occurs. The early stages of stroke (acute and acute) have the greatest number of life-threatening complications. The specified period is the period of time from the onset of the disease to 3 weeks (the most acute period is the first 24 hours). The more severe the patient's condition, the greater the threat to life at the onset of the disease.
Stroke can vary in severity
That is why basic treatment measures should be carried out as early as possible. Correct provision of assistance in the initial stages of stroke reduces the likelihood of death and increases the chances of recovery. The survival of patients with severe stroke directly depends on the location of the vascular accident and the quality of treatment.
Mechanism of violation
An extensive stroke differs from a localized form of the disease.
They consist in the fact that other types of strokes are characterized by blockage of blood vessels in the brain (ischemic type of disorder) or hemorrhage (hemorrhagic), in which large vessels are damaged, and with an extensive stroke, the lesions are localized in several parts of the brain. Because of the extensive damage to the brain, patients with a major stroke have little chance of survival, and survivors have little chance of regaining lost function.
Classification
What classification allows you to distinguish between strokes? The most significant category is the extent or extent of the lesion. The following types are distinguished:
- Transient ischemic attack (TIA). Symptoms are isolated and disappear within 1 hour. The maximum duration of their existence is 12-24 hours. Typically, a TIA does not leave any focal changes in the brain that are noticeable on an MRI or CT scan.
- “Minor stroke” is a transient attack, the symptoms of which last for 2-21 days. In this case, complete regression of the neurological clinic is observed a month after the attack;
- Progressive stroke. There are general cerebral and focal syndromes. The acute phase develops over 2-3 days, followed by incomplete restoration of function;
- Completed stroke. With it, a focus of necrosis has formed, there is a loss of functions and only partial regression of the clinic in the recovery period.
What causes trouble?
A major stroke can be caused by any cause associated with a negative effect on the blood vessels of the brain. Thus, the following conditions can be considered as prerequisites for the occurrence of extensive brain damage:
- vascular atherosclerosis;
- presence of diabetes mellitus (this disease contributes to the formation of blood clots);
- hypertonic disease;
- obesity due to physical inactivity;
- the presence of heart pathologies (defects, arrhythmias, and also in patients with an artificial valve in the heart);
- ischemic attacks;
- high cholesterol.
In addition, people who lead an unhealthy lifestyle, abuse alcohol and smoke, are at risk.
Statistics: how long do they live after an attack?
The first days after the stroke are crucial in the course of the disease and life expectancy. Up to 25% of patients die in the first 7-30 days. Reasons for this:
- pulmonary artery blockage;
- pneumonia;
- cerebral edema;
- renal failure.
Young, children and teenagers
Although ischemic stroke occurs more often in people over 60 years of age, recently it has also become “younger.”
Women who use oral contraceptives, pregnant women and mothers of newborns, as well as young people and even children with vascular pathologies or diabetes are at particular risk. also be a consequence of traumatic brain injury.
The prognosis for life in young people is favorable; more than 75% of patients under the age of 45 survive.
Elderly people
- People over 45 years of age suffer strokes more often and more severely than younger people. With age, the number of concomitant diseases increases, significantly complicating recovery. The majority suffer from arterial hypertension and have certain diseases of the cardiovascular system. In 30% of cases, older people suffer a second stroke within the next 2-3 years.
- In rare cases, if the leading areas of the brain are not affected, treatment is started in a timely manner, lifestyle and nutrition are adjusted, and doctors’ recommendations are followed - patients over 50 years of age have a chance to live another 5-7 years.
- The likelihood of having a stroke among those over 60 doubles every 10 years. Statistics show that 75% of the total number of strokes occurs in people over 65 years of age.
- After 70 years, the chances of surviving a stroke are minimal, the consequences are severe - complete paralysis, coma. Full recovery is impossible; a person will no longer be able to care for himself.
Differences between left- and right-sided lesions
A major brain stroke can affect both the left and right hemispheres of the brain. With disorders on the left side, the patient’s psycho-emotional state is much more disturbed than with damage to the right side of the brain.
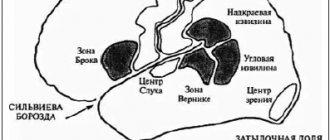
Since the speech center is located in the left hemisphere, if there is a disturbance in this part of the brain, the patient is completely or partially deprived of the ability to speak.
If the right side is damaged, such consequences can only occur for a left-handed person, since the speech center in such patients is located on the right.
With damage to the right hemisphere, recovery of motor activity is more difficult and slower than with left-sided strokes. This happens because the patient’s psyche is affected to varying degrees, and in the first case he is most often apathetic and indifferent to everything.
Consequences of a cerebral stroke
Cerebral stroke ranks second, after myocardial infarction, in the structure of mortality of the Russian population. Considering this fact, stroke belongs to the category of diseases that require mandatory rehabilitation measures - restorative treatment, which is also a guarantee against relapse of the disease.
Brain stroke, its types and risk factors
Depending on the cause of stroke, it is divided into three types: hemorrhagic, ischemic and subarachnoid. However, in medical statistics, ischemic stroke predominates (70–85%), when compression or blockage of blood vessels occurs as a result of thrombosis, embolism or other diseases of the blood vessels, heart or blood.
Unlike ischemic stroke, where there is compression of blood vessels, in the hemorrhagic type (20–25%) they rupture, followed by hemorrhage into the brain, under its membranes or into the ventricles. The least common (1–7%) is subarachnoid stroke, which is of a traumatic nature: due to rupture of an arterial aneurysm or traumatic brain injury. When it occurs, hemorrhage occurs in the space between the arachnoid and pia mater of the brain.
A stroke is considered an attack in which a neurological deficit (focal or cerebral) lasts more than a day; this period is called transient disturbances of the blood supply to the brain. A condition in which neurological functions are restored within three weeks is designated a minor stroke.
The mortality rate for different types of strokes varies, and on average is:
- for ischemic stroke – no more than 15%;
- for hemorrhagic stroke – no more than 33%;
- with subarachnoid hemorrhage - up to 50%.
You can reduce the likelihood of a stroke by not forgetting about the risk factors that are considered to be:
- age from 50 years (diet and sleep regime required);
- male gender;
- arterial hypertension (keeping a “blood pressure diary” is recommended);
- chronic heart diseases (timely examinations and surgical operations);
- transient ischemic attacks (considered to be harbingers of heart attacks and brain);
- type of work (for example, with high nervous stress);
- smoking (affects blood pressure);
- obesity and high cholesterol;
- diabetes;
- asymptomatic stenosis of the carotid arteries;
- stroke in direct relatives.
In Russia, risk factors include emergency hospitalization, which does not exceed 30% of all stroke cases, the lack of properly equipped intensive care units and failure to implement rehabilitation programs.
Primary stroke diagnosis and assistance
During the initial examination, the patient is asked to perform several actions:
- Extend your arms in front of you, palms up, with your eyes closed. If one of the arms begins to uncontrollably “go” down and to the side, this is a sign of a stroke.
- Raise both arms above your head. They should rise evenly to the same height.
- Stick out tongue. If it is modified (curved) and/or “falls” to the side, this is another sign of a stroke.
- Say one simple sentence. With a stroke, speech defects often appear, diction and articulation deteriorate.
- Smile. In a patient who has suffered a stroke, the smile will be distorted, and the corners of the lips will “look” in different directions.
If suspicions of a stroke are confirmed, you must immediately call an ambulance and inform doctors about the symptoms noticed, regardless of their disappearance or intensification. Hospitalization is needed urgently: in the hospital, MRI, transcranial Doppler ultrasound, MR spectroscopy and other types of studies that will confirm or refute fears should be performed.
If signs of a stroke are detected, after calling an ambulance, first aid must be provided, which consists of several actions:
- raise the patient's head above body level by 30 degrees;
- loosen tight clothing: belts, collars, etc.;
- measure pressure;
- take a medicine that normalizes blood pressure from those that have already been used by the patient previously;
- if you don’t have the necessary medications on hand, you can put your feet in a basin of moderately hot water;
- turn the patient onto the right side (place a tray under the lower jaw if there is vomiting).
After completing all the steps, it is recommended to open the front door in advance and wait for the ambulance team to arrive. And after her arrival and the patient’s reluctance to go or the paramedics to take him to the hospital, insist on immediate hospitalization.
Symptoms and consequences of stroke
As a result of the death of nerve cells in the brain from oxygen starvation, neurological disorders occur during a stroke, which, depending on the type of stroke, may initially lead to dizziness, weakness or loss of consciousness, up to the development of a coma, as well as perspiration on the forehead, pulsation of the cervical arteries, a sharp drop in pressure, vomiting, hoarse unnatural breathing, rare pulse, numbness of the limbs, pallor, pain in the head and sometimes in the heart area. Symptoms may be more or less pronounced, depending on the location of the circulatory disorder and its extent.
A stroke can occur in three variants: favorable (consciousness is restored after a few minutes or hours), intermittent or progressively severe (when consciousness returns only after three days or more). With a favorable prognosis of treatment for a stroke, over time it is possible to restore all impaired brain functions; in the intermittent variant, most of the disorders are subject to restoration, although a recurrent stroke and the addition of additional diseases are possible: pneumonia, heart disease. The progressive course of a stroke is accompanied by an increase in symptoms and often ends in death.
Neurological disorders typical of a stroke include partial or complete paralysis, speech defects or complete loss, visual impairment, hearing impairment, and memory loss.
The consequences of a stroke cannot be avoided, but conditions can be created for partial or complete recovery. Among these conditions the following should be highlighted:
- quick and correct diagnosis;
- immediate hospitalization;
- compulsory rehabilitation.
Of course, there are factors that a person cannot influence, such as the strength and type of stroke, its location and extent, with the exception, perhaps, of careful attention to risk factors and preventive actions.
Rehabilitation after stroke
In Russia, no more than 20% of patients who have suffered a stroke are admitted to rehabilitation centers and departments. The rest are either treated at home or do not undergo active rehabilitation programs at all. Moreover, statistics show that early thirty-day mortality in patients after a stroke occurs in 43% of cases if they were treated at home, and 24% if they were treated in a hospital.
- pedagogy;
- psychotherapy;
- drug therapy;
- occupational therapy;
- speech therapy;
- physiotherapy;
- kinesiotherapy;
- acupuncture;
- manual therapy and massage;
- hirudotherapy;
- dietetics, etc.
It is very important to conduct active rehabilitation programs in environmentally friendly places where fresh, unpolluted air is available. After all, the human brain consumes up to a quarter of all inhaled oxygen, and after a stroke, the requirements for air quality increase.
People who have had a stroke often experience neurocognitive problems such as sudden mood changes or fatigue. All this requires rehabilitation in conditions as close as possible to home ones, reproducing not only everyday coziness and comfort, but also ensuring attentive attention from all service and treatment personnel.
The rehabilitation center uses traditional, latest and original recovery methods for people who have suffered a stroke.
Extensive practice and rich knowledge of the treating staff in the field of rehabilitation medicine allow us to provide comprehensive rehabilitation at the highest level, meeting Western standards.
Rehabilitation service. located in a picturesque coniferous forest, corresponds to the status of a four-star hotel with 35 single rooms. The fruits of the joint work of a nutritionist and the chef of the Three Sisters restaurant, who knows how to make balanced nutrition tasty, will not leave anyone indifferent.
Persons Ministry of Health of the Moscow Region
No. LO-50-01-003671 dated August 29, 2012
There are contraindications. Consult your doctor.
Symptoms and manifestations
The clinical picture of a major stroke is so clear and specific that there are no difficulties in making a diagnosis. Symptoms of the disorder are:
- violation of facial symmetry, crooked smile;
- severe weakness in the limbs;
- slurred speech or complete absence of speech.
Also, such disorders are accompanied by less pronounced symptoms, namely:
- coordination of movements is impaired;
- severe headaches appear;
- disturbances of consciousness occur in varying degrees of severity;
- the patient practically does not perceive other people's speech.
If such symptoms occur, seek medical help immediately.
What are the consequences and chances
The consequences of a major stroke depend on how large the area of brain damage is. Here are some common complications.
The patient's functions are impaired:
- speech;
- vision;
- hearing;
- coordination of movements;
- orientation in space.
The following are completely or partially lost:
- sense of smell;
- feeling of pain;
- tactile sensations.
And:
- memory is impaired, attention becomes distracted, the patient experiences difficulties in the process of perceiving information;
- paralysis occurs in one of the body parts or limbs;
- with significant brain damage, coma and death may occur.
The effects also depend on what part of the brain is affected. Thus, with an extensive stroke of the right hemisphere, paralysis of the left side of the face and body occurs, as well as memory impairment.
If the left side is damaged, speech and thinking abilities are impaired, and paralysis of the face and body on the right side is observed.
If a massive stroke affects both hemispheres of the brain, it leads to complete paralysis.
Coma with OI
Sometimes extensive strokes lead to coma, this occurs in cases of massive hemorrhages.
Loss of consciousness occurs, and the patient cannot come to his senses. He does not react to external stimuli, and there is also a lack of reflexes, only swallowing and breathing are preserved. There are frequent cases of arbitrary urination and defecation.
In this state, destructive processes occur in the body, and the longer the patient is in a coma, the more extensive they are.
In the case where coma occurs as a result of a hemorrhagic stroke, most often the patient dies within 24-36 hours due to the development of cerebral edema.
Ischemic stroke or cerebral infarction
Ischemic stroke, or cerebral infarction, is an acute condition in which cerebral circulation is impaired, accompanied by damage and softening of tissue, changes in brain function due to the cessation of blood supply to its areas.
The disease is characterized by a sudden onset and an increase in symptoms over the course of a day.
During this period, death or a significant reduction in a person’s vital abilities occurs. A period of 28 days from the onset of the first signs of stroke (acute period) is also considered dangerous. At this time, about 35% of initially surviving patients die.
Commitment to stroke
Among all strokes, ischemic ones account for about 85%. Over the course of a year, more than 5 million people worldwide die from this disease; in Russia, more than 400 thousand become completely disabled; approximately 40% of those who survive survive and only 8% are able to return to full-time work.
People over 45 years of age are most susceptible to strokes, more often men. In recent years, there has been a trend towards the development of cerebral infarction among young people - 30 years and older.
Pathogenesis: what happens during an attack?
The degree of damage to brain tissue depends on the duration and extent of the decrease in cerebral blood flow. The optimal intake is 50-60 ml. blood per 100 g of brain tissue per minute. If this figure drops to 35 ml. There is a violation of glycolysis (the breakdown of glucose), which leads to a change in the state of the cerebral cortex.
If the blood flow volume decreases to 15 ml. this causes rapid irreversible damage to neurons and the formation of an infarct area (softening).
Progression of the disease is observed due to further disruption of the blood supply to the area adjacent to the damaged area. The final formation of the ischemic area ends after 56 hours.
Pathological processes are accompanied by cerebral edema, increased intracranial pressure, as well as the migration of leukocytes into tissues and their damage to healthy cells. A common cause of death in patients is compression of the medulla oblongata or cerebellum by swollen tissue.
Causes of the disease
The disease is preceded by disruption of the activity of cerebral vessels as a result of the pathological influence of certain diseases. The carotid, vertebral and cerebral arteries and their branches are predominantly affected.
The etiology of ischemic stroke includes the following factors:
- Vascular atherosclerosis.
- Thromboembolism.
- Diabetes.
- Congenital vascular pathologies.
- Hypertension.
- Rheumatism.
- Vasculitis.
- Carotid artery stenosis with progression of osteochondrosis, spondylosis.
- Infectious and allergic arteritis.
- Blood diseases (for example, leukemia).
- Diseases of the heart muscle (defects, coronary disease).
- Severe renal dysfunction.
- Bronchial asthma.
Often, a hemorrhagic stroke resulting from a rupture of an aneurysm is complicated by an ischemic one.
Old age and a hereditary predisposition to vascular diseases also affect the incidence of strokes.
The following can serve as a trigger for the development of the disease or long-term aggravate the condition of the blood vessels:
- stress;
- smoking;
- abuse of fatty foods, obesity;
- alcoholism.
Classification
Depending on the period of occurrence, strokes can be:
- Primary (developing for the first time in life).
- Secondary (repeated ischemic stroke in a patient who previously had the disease).
According to etiology, ischemic strokes are distinguished as follows:
- Thromboembolic (occur due to blood thickening and impaired blood supply to the brain).
- Cardioembolic (resulting from myocardial infarction or heart valve disease).
- Hemodynamic (develop due to spasm of cerebral vessels, for example, due to abnormal blood pressure).
- Lacunar (observed when small arteries are affected - up to 15 mm.).
According to severity, strokes are:
- Transient ischemia (focal disorders that regress within 1 day).
- Small strokes (symptoms of the disease regress within 21 days).
- Progressive stroke (a disease with an increase in symptoms up to 3 days).
- Total stroke (formed area of cerebral infarction).
Periods of ischemic stroke:
- very acute (3 days), including the first 3 hours – the “therapeutic window”, when brain cells are able to recover subject to the restoration of blood supply;
- acute (28 days);
- early recovery (6 months);
- late recovery (2 years).
Symptoms and common signs of stroke
The clinical picture is largely determined by the area of brain damage . Most strokes occur in the carotid region as a result of dysfunction of the middle cerebral and carotid arteries. If the disease develops due to occlusion of a large artery, an extensive ischemic stroke is possible when the area of softening of the brain is large. This entails an immediate increase in the clinical picture of a stroke, most often leading to death in the first hours.
A stroke can occur at any time of the day, more often after drinking alcohol, stress, or swimming in hot water.
Depending on whether the patient has a left- or right-sided stroke, symptoms may affect only one side of the body.
Focal neurological symptoms of the disease, increasing over 3-4 hours, several weeks or developing at lightning speed:
- leg weakness;
- numbness of hands;
- unilateral decreased vision, strabismus;
- paresis and paralysis of organs in one part of the body (feet, hands);
- violation of flexion, grasping reflexes, fine motor skills;
- urinary retention;
- inability to swallow, chew;
- hearing and speech disorders;
- failure of respiratory functions;
General cerebral symptoms of stroke do not occur in every case and are determined by the degree of development of edema, more often
- for bilateral strokes:
- vomit;
- clouding of consciousness;
- severe headache;
- dizziness;
- overexcitement;
- falls;
- disorientation in space;
- mental disorders;
- decreased or absent sensitivity;
- increased body temperature, sweating;
- in the case of a major stroke, coma may develop.
Consequences and complications for humans
Complications that often accompany the course of a stroke and can cause the death of the patient are:
- pneumonia;
- myocardial infarction;
- renal failure;
- thromboembolism;
- dehydration, bedsores.
After an ischemic stroke, the patient's condition is caused by changes in the left hemisphere of the brain.
Health consequences may include:
- Inability to swallow food.
- Partial, complete loss of vision.
- Deviant behavior – aggression, phobias, reluctance to communicate.
- Incontinence of feces and urine.
- Mental and cognitive disorders.
- Headaches, seizures, epilepsy.
With a stroke of the brain stem or other significant parts, surviving patients often completely lose functions coordinated by the nervous system, which leads to disability with the inability to self-care.
Prognosis for recovery
The prognostic calculation for the preservation of life and recovery depends on the volume of cerebral infarction, as well as the location of its localization.
A third of people die within a month after the onset of the disease, most of them 1-2 days after the attack.
The lowest incidence of deaths is among patients with lacunar stroke (only 2%). Only a small proportion of patients recover completely. The majority of people who have suffered an ischemic stroke and survived become disabled to varying degrees of severity. Restoration of basic vital functions is possible within 1 year after the episode of illness. The 5-year survival rate is about 50%. A recurrent stroke develops in 30% of people.
Diagnosis
During a physical examination, the doctor evaluates the signs of the disease, notes murmurs in the heart and carotid artery, and the difference in pressure measured on the left and right arms. A person's medical history can help determine the cause of an ischemic stroke.
Instrumental research methods are ultrasound with Doppler sonography, angiography, CT or MRI of the brain. An ECG, ultrasound of the heart, and laboratory tests (general clinical, biochemical) are required. The disease is differentiated from hemorrhagic stroke, tumors, inflammatory diseases or toxic brain lesions.
First aid for stroke
First aid to the patient should be provided immediately after the first symptoms of the disease are detected. The person must be placed in bed, preventing any movement. In case of loss of consciousness, it is necessary to revive him with the help of ammonia, wine vinegar, and splashing cold water on the face.
To avoid tongue sinking, the head should be slightly higher than the level of the body. Feet and hands can be rubbed with a soft brush or a towel moistened with warm water.
Treatment options
The patient is urgently hospitalized, after which emergency therapy is performed (can also be carried out by an ambulance team):
- Improving blood circulation in the stroke area - reopolyglucin drip.
- Normalization of neuronal metabolism - cerebrolysin, nootropil intravenously.
- Reducing blood pressure - Relanium, droperidol, dibazol intravenously.
The complex of treatment measures for stroke includes:
- Normalization of respiratory function using air ducts, sometimes tracheostomy, intubation.
- Relieving pulmonary edema - cardiotonic drugs, oxygen inhalations, sodium bicarbonate injections.
- Reducing cerebral edema - glucocorticosteroids, mannitol, Lasix injection.
- For fever - a solution of amidopyrine, analgin, diphenhydramine, novocaine.
- Improving cerebral circulation - nootropic, vasodilating, antiaggregation agents.
- Planned correction of blood pressure.
- With a sharp decrease in pressure - solutions of mezaton, korglykon, norepinephrine intravenously.
- Prevention of dehydration – up to 2.5 l. saline solution with glucose per day, drip.
- For potassium deficiency - injections of potassium chloride, potassium nitrate.
- Reducing vascular permeability - ascorbic acid in the form of injections.
- If pneumonia develops, use antibacterial therapy.
- In case of urinary retention - catheterization and lavage of the bladder.
- To avoid bedsores, wipe the patient’s skin with camphor alcohol, antiseptics, and turn over 4 times a day.
- After removal of acute symptoms - anticoagulant therapy (heparin, phenylin, ecofemin, fibrinolysin), administration of antihypoxants (phenobarbital, gutimin), neuroprotectors.
- In some cases, surgical intervention may be necessary, the purpose of which is to reduce intracranial pressure and restore cerebral blood flow.
After the patient leaves the hospital, lifelong prevention of recurrent strokes is recommended:
- taking antihypertensive drugs, antiplatelet agents, anticoagulants, muscle relaxants, antioxidants, lipid-lowering drugs;
- correction of blood glucose levels;
- treatment of heart rhythm disorders.
The patient undergoes examinations several times a year by a neurologist and other specialists, and also adheres to a diet and engages in exercise therapy.
Lifestyle and rehabilitation
After a person is placed in a rehabilitation ward, bed rest is gradually replaced by ward rest, and then by free rest. After 2-3 months he is discharged from the hospital. The best option for recovery after a stroke is to visit a specialized sanatorium. At home, mandatory measures to maintain and improve the health of a stroke survivor are:
- Massage, electrical stimulation of muscles.
- Acupuncture.
- Passive and active gymnastics (twice a day for 40 minutes).
- Water procedures.
- Learning to walk or use a wheelchair.
- Providing tube feeding in case of swallowing dysfunction.
- Use of diapers or convenient location of the patient near the toilet.
- Skin care.
- Classes with a speech therapist.
- Psychotherapy, fight against depression.
- Teaching self-care skills, writing, reading, counting.
- Occupational therapy.
The patient's relatives should monitor any changes in his condition, since the risk of a recurrent stroke at first is very high.
Diet after stroke
The main goal of the nutritional system is to reduce animal fats and salt in the diet, as well as normalize weight.
Products allowed for consumption after a stroke:
- any vegetables, fruits;
- juices;
- fermented milk food (low fat);
- lean meat, fish;
- cereals;
- fructose-based sweets;
- compotes, jelly, herbal infusions.
You should eat bananas, citrus fruits, dried apricots, carrots, and cabbage as often as possible. Drinking regime – up to 1 liter. liquids per day.
Foods recommended for exclusion:
- fat meat;
- eggs;
- fatty dairy products;
- baked goods, sweets;
- marinades, pickles;
- smoked meats;
- over-salted food.
Treatment with folk remedies
During the rehabilitation period, it will be useful to give the patient remedies prepared according to folk recipes:
- To improve the functioning of the nervous system - tincture of marina root (1 liter, 3 times a day).
- For the same purpose - mumiyo (according to the instructions).
- Visual and hearing impairments can be eliminated by regular intake of infusions of hawthorn berries, walnut partitions, birch leaves, and onion peels.
- Every day you need to consume pollen, as well as 1 spoon of lemon juice and beet juice.
- Restoration of paralyzed limbs: infuse 3 l. bay leaf per 200 ml. vegetable oil 7 days. Then lubricate the affected areas daily.
First aid
In case of a stroke, first aid is of great importance. The outcome of the disease and how severe the consequences will depend on timely and correct actions.
When a person suddenly becomes ill, an ambulance should be called immediately. In addition, the following actions should be taken while waiting for the arrival of doctors:
- lay the victim down, it is better if the surface is hard;
- unbutton the collar and remove clothing that restricts movement;
- open the windows in the room to provide access to fresh air;
- turn the patient's head to the side to prevent vomit from entering the respiratory tract;
- apply cold water to your head;
- massage paralyzed limbs.
While waiting for an ambulance, you should not give the patient food or water, or monitor his breathing and pulse.
It must be remembered that in case of acute circulatory disorders in the brain, minutes count and you cannot delay in providing help.
Therapeutic assistance
As first aid during the first few hours after the onset of a stroke, the following measures are taken:
- connecting an oxygen device;
- decrease in blood pressure;
- fight against cerebral edema;
- relief of seizures;
- heart rate correction;
- blood thinning measures.
Diagnosis is carried out using MRI, ECG and CT, as well as blood tests. Based on the results, treatment is prescribed. Its goal is to eliminate the consequences, restore blood circulation in the brain and lost body functions.
The selection of medications is based on the characteristics of the patient’s condition, and also depends on the type of stroke.
Major ischemic stroke requires thrombolytic drug therapy. Medicines are prescribed that thin the blood and act on the formed blood clots.
Treatment is carried out using:
- Aspirin and Cardiomagnyl for blood thinning ;
- vasoactive drugs (Pentoxifylline, Vinpocetine, Trental, Sermion);
- antiplatelet agents (Plavix, Tiklid);
- anticoagulants (Heparin, Fragmin, Nadroparin);
- neurotrophics (Piracetam, Cerebrolysin, Nootropin, Glycine);
- angioprotectors (Etamsylate, Prodectin);
- antioxidants (vitamin E, vitamin C, Mildronate).
In hemorrhagic strokes, on the contrary, it is necessary to increase blood clotting in order to stop the bleeding that occurs due to rupture of blood vessels.
Most often used:
- Strophanthin (for heart support);
- Lasix and Uregit (as diuretics);
- Reopoliglyukin;
- various drugs that lower blood pressure.
In especially severe cases, only neurosurgery can save the patient. Inpatient treatment is followed by a period of rehabilitation and recovery.
Principles of inpatient treatment
Patients diagnosed with a severe form of stroke are hospitalized in the intensive care unit. Very often they arrive in a state of coma, often with breathing problems, which requires them to be connected to a ventilator. Hemodynamics in such patients is also seriously affected. Control and stabilization of blood pressure and myocardial contractility must be carried out (vasopressors, antihypertensive therapy, cardiac glycosides, antiarrhythmic drugs, depending on the situation).
In the treatment of cerebral edema, drugs from the group of diuretics (mannitol, furosemide) are of great importance, ensuring the removal of excess fluid from the body. At the same time, it is important to restore normal blood circulation in the vessels of the brain and improve cellular metabolism. Antiplatelet agents and neuroprotectors are used for these purposes.
Antihypertensive therapy is of great importance in the treatment of hemorrhagic stroke, as it helps reduce the intensity of bleeding. However, it must be performed under blood pressure control, since severe hypotension will aggravate neuronal hypoxia. At the same time, hemostatic drugs (dicinone) are prescribed.
With a hemorrhagic stroke, dislocation of the brain often occurs, that is, displacement of its elements by an increasing hematoma. This is an extremely dangerous condition because it can lead to compression of vital parts of the brain. In this case, there is a need for surgical intervention. However, it should be remembered that coma, uncompensated concomitant pathology and the unstable serious condition of the patient are contraindications to surgery.
Recovery and rehabilitation
In order to restore a patient after a major stroke, a lot of effort will be required. Moreover, there is no need to talk about complete recovery.
Rehabilitation of such patients is carried out in specialized centers and sanatoriums and includes:
- Drug therapy . Its main goal is to maintain blood vessels and the heart, as well as restore impaired body functions.
- Massage . Various massage techniques are used, from light stroking to deep kneading to restore blood circulation in the affected limbs.
- Acupuncture . The targeted effect has a general strengthening effect and helps normalize blood circulation.
- Physiotherapeutic procedures . Most often, magnetic therapy and electrophoresis are prescribed for a deep effect on muscle tissue.
- Therapeutic physical education . Gymnastics helps restore motor activity and strengthen muscles.
In addition, the patient needs to follow a diet and spend more time in the fresh air. It is good if relatives have the opportunity to pay more attention to such patients, this has a beneficial effect on the psycho-emotional state of the patient.
The rehabilitation process can take from several months to 2-3 years, it depends on the severity of the lesions.
How to recover
Recovery after a stroke occurs in several stages. Rehabilitation is necessary - during this period, all vital functions lost after the stroke are restored. To speed up recovery, patients need to go to a specialized center. Rehabilitation consists of 3 periods:
- early (up to 6 months);
- late (from 6 to 12 months);
- residual (from 12 months).
Important information: How to quickly recover a person after a stroke at home (rehabilitation)
Each stage of recovery must be accompanied by therapeutic physical training. Special exercises help develop paralyzed limbs. Speech and psycho-emotional state are restored under the supervision of specialists - a speech therapist and a psychotherapist.
For prevention purposes
To prevent strokes, the following preventive measures are recommended:
- lead a healthy lifestyle.
- quit smoking and alcohol.
- play sports, planning exercise in accordance with age and health status.
- try to avoid stress.
- eat right, reduce consumption of fatty foods, flour, sweets, as well as coffee and strong tea.
- control weight.
- in the presence of diabetes mellitus and hypertension, carry out timely treatment.
It should be noted that strokes do not appear out of nowhere; they are preceded by a number of signs and symptoms, by which one can determine the approach of the disease and take appropriate measures.
Prevention of recurrent stroke
Prevention of recurrent stroke should be carried out in several directions at once. First of all, you need to adjust your lifestyle in accordance with your new condition and limitations.
With the help of specialists, the patient’s physical activity standards and permitted loads are determined for each specific case.
In addition, it is necessary to support many processes in the body, control the levels of sugar and cholesterol in the blood.
Drug therapy as a preventive measure involves the use of drugs that normalize blood pressure, blood viscosity and prevent the formation of blood clots.
In addition to the above, we should not forget about the ban on smoking and alcohol, as well as proper nutrition.
Life after a stroke
Bleeding in the brain rarely goes away without dangerous consequences for the body. The disaster suffered affected all organs and systems, so life after it must obey new rules. Measures will avoid a major blow and minimize the risk of relapse.
The victim is obliged:
- Avoid strong psycho-emotional outbursts.
- Control and treat stress disorders.
- Do not overload the body with physical activity, exhausting exercises, or lift heavy objects.
- Follow a diet.
- Avoid weight gain—extra pounds cause increased blood pressure.
- Refuse to work that requires daily mental and physical stress.
- Constantly monitor blood pressure levels - if the numbers are consistently high, consult a doctor.
- Undergo periodic examinations at least once every 6 months - see a neurologist, cardiologist, or therapist. If you have chronic diseases, contact a specialized specialist.
- Analyze medications taken - they should only be prescribed by a doctor, and the patient must inform him about the ischemic or hemorrhagic stroke suffered.
Life after a cerebral infarction can be at a decent level. The patient learns to fully care for himself, his speech, the ability to move, and orient himself in space are restored. But in order to speed up the process and prevent a relapse, you should seek help from professionals.