Causes of hemorrhagic stroke
Common causes of stroke include smoking, obesity, and a diet high in trans fats and sugar. In rare cases, strokes are caused by taking sympathomimetic drugs (cocaine), and even less often by congenital aneurysms, a type of arteriovenous or vascular malformation, trauma, primary brain tumor, overdose of anticoagulants, intracranial arterial dissection, vasculitis.
In 20-40% of patients with ischemic infarction, hemorrhagic transformation is observed within a week after the first attack - saturation of the ischemic area with blood.
Subarachnoid hemorrhage occurs between the arachnoid and pia mater. In 85% of cases, the cause is congenital berry aneurysm. There is a separate type of traumatic subarachnoid hemorrhage. Aneurysmal bleeding can occur at any age, but most often occurs after 40 years. Less common causes include arteriovenous malformations and bleeding disorders.
The risk of hemorrhagic cerebral stroke increases with the participation of the following factors:
- age after 55-60 years;
- hypertension (up to 60% of cases);
- history of strokes;
- alcohol and drug abuse.
Stroke with hemorrhage develops against the background of hypertension, cerebral amyloidosis, coagulopathy, anticoagulant therapy, thrombolytic agents after myocardial infarction, arteriovenous malformations, vasculitis, tumors.
Etiology of the disease
The leading cause of the development of hemorrhage into the cranial cavity is reduced elasticity and strength of the vessels supplying blood to the brain. Such changes are associated with the following pathological conditions:
- Arterial hypertension of any cause. Changes in blood vessels are observed during hypertensive crises and a constant slight increase in blood pressure.
- The presence of congenital or acquired vascular anomalies. Malformations, characterized by areas of chaotic connection of arteries and veins with each other, as well as aneurysms increase the risk of vascular rupture. An aneurysm is a protrusion of the vascular wall, which is often thin and inelastic.
- Atherosclerotic lesion of arteries. Lipid plaques located in the arterial wall lead to its fragility. Most often, atherosclerosis is detected at the site of vessel branching.
- Inflammation of the arterial wall, which is observed during meningitis, encephalitis, intoxication conditions and against the background of autoimmune diseases.
- Pathology of the blood coagulation system. Reduced activity of platelets or coagulation factors can cause hemorrhagic stroke. Hematological diseases and irrational use of Aspirin, Heparin and other blood-thinning medications lead to such changes.
In addition to these diseases, doctors identify risk factors that increase the likelihood of developing hemorrhagic stroke. These include overweight, hypercholesterolemia, leukopenia (decreased number of white blood cells), poor nutrition, bad habits, chronic stress, diabetes, heart disease and family history with cases of cerebrovascular accidents in relatives.
Mechanism of development of hemorrhagic stroke
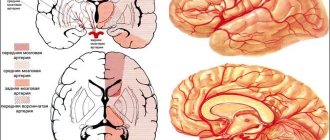
Understanding the mechanisms of its development will help you understand what a hemorrhagic stroke is. Blood as a result of intracerebral hemorrhage accumulates in the form of a hematoma, which compresses adjacent brain tissue, causing neuronal dysfunction. Large clots increase intracranial pressure. The pressure of supratentorial hematomas and subsequent cerebral edema provokes hernias - compression of the brain stem and secondary hemorrhages in the pons.
Hemorrhage that disrupts the integrity of the ventricles of the brain causes acute hydrocephalus. Cerebellar hematomas can block the fourth and disrupt the function of the trunk. With a diameter of more than 3 cm, hernias are provoked.
Hernias, hemorrhages in the subcortical brain and ventricles, acute hydrocephalus and pressure on the brain stem are the causes of loss of consciousness, coma and death.
The accumulation of blood in the subarachnoid space causes chemical meningitis, which increases intracranial pressure over several days or weeks. Secondary vasospasm causes focal cerebral ischemia. 25% of patients develop signs of transient ischemic attack or ischemic stroke. With major cerebral edema, the risk of vasospasm is greatest within 72 hours to 10 days. Secondary acute hydrocephalus may develop, and sometimes repeated bleeding occurs within a week.
Hematoma formation occurs in almost 40% of cases and is accompanied by persistent neurological deficit. Aneurysms of the anterior communicating artery lead to hematomas in the frontal lobe, and of the pericallosal artery - in the corpus callosum and cingulate gyrus. In case of aneurysms of the internal carotid artery, the hematoma affects the basal ganglia and the middle part of the temporal bone, and the middle medulla affects the temporal part and the Sylvian fissure. Complications arise in cases of hematoma breakthrough. Almost 26% of aneurysm ruptures result in hemorrhage into the ventricles of the brain, especially when localized in the anterior communicating artery.
Symptoms and first signs
The duration of the pre-stroke condition can vary from several hours to days. Based on some signs, you can detect the development of pathogenic processes and seek help from doctors, which will prevent serious complications. Warning signs of stroke caused by cerebral hemorrhage include:
- headaches, dizziness;
- nausea, vomiting;
- impaired sensitivity of the limbs;
- general weakness;
- fast fatiguability;
- facial skin hyperemia;
- changes in heart rate.
If there are several signs that precede a hemorrhagic stroke, you need to seek help from a medical facility. If these symptoms are detected in a loved one, there is a standard test that can determine the onset of an attack:
- crooked smile;
- turning the tongue to the side;
- inability to lift the upper limbs and keep them in one position;
- incoherent speech.
Hemorrhagic stroke is characterized by suddenness. All symptoms are getting worse every minute. A sharp headache, which is accompanied by loss of consciousness, indicates rapid hemorrhage, since with the ischemic variant of the disease, pathological processes proceed more slowly. Symptoms of the disease also include:
- impaired coordination of movements;
- hearing loss;
- lack of focus;
- heart failure;
- intermittent breathing;
- loss of sensitivity in the facial muscles;
- paralysis;
- coma.
It is important to know what a hemorrhagic stroke is and what its symptoms are. If you detect any signs of the disease, you should immediately seek help from specialists. This will prevent the development of serious complications and preserve basic brain functions.
Classification of intracerebral bleeding
Types of hemorrhagic stroke depend on the location. Parenchymal hemorrhage occurs in the brain tissue, intraventricular hemorrhage occurs in the ventricular system, subdural and epidural localization is distinguished - blood accumulates above and below the dura mater. Subarachnoid bleeding occurs between the arachnoid and pia mater. The first and last types of cerebral hemorrhages are the most common.
Intracerebral hemorrhage
A cerebral hemorrhage is bleeding from a damaged vessel into the brain parenchyma, leading to cell death. Symptoms almost always occur while awake: suddenly or increase gradually. Typically, the following clinical manifestations worsen within 30-90 minutes:
- sudden weakness;
- paralysis, numbness in any part of the body;
- speech problems;
- eye movement disorders;
- vomit;
- walking disorder;
- irregular breathing;
- loss of consciousness, stupor, coma.
Brain hemorrhage accounts for about 10% of all strokes, but has a much higher percentage of deaths. Almost half of patients with major bleeding die within a few days. Most survivors do not regain all of their lost brain function. After 60 years, intracerebral hemorrhage is more common than subarachnoid hemorrhage.
Subarachnoid hemorrhage
Subarachnoid hemorrhage is the filling of the space between the arachnoid and pia mater. The accumulation of blood increases pressure on the brain tissue, leading to headaches. Most often, hemorrhage occurs due to an aneurysm. In almost 50% of cases, this type of stroke is fatal within four weeks, and survivors face severe disabilities. Subarachnoid hemorrhage occurs more often in women. The risk increases with smoking, alcohol abuse, and hypertension.
Subarachnoid hemorrhage accounts for 15% of all strokes and nearly a quarter of deaths as a result. In almost 75-80% of cases, the cause is a rupture of an aneurysm in the circle of Willis or its arterial branches. In 10% of cases, the condition develops due to arteriovenous malformation.
The main signs of hemorrhage in the subarachnoid space:
- sudden and severe headache;
- pain in the face and eye area;
- double vision;
- impairment of peripheral vision.
Without repair of the blood vessel, bleeding continues for another 14 days in every fifth surviving patient. Without surgical intervention, relapses occur within six months in 50% of cases.
Causes and risk factors
The development of hemorrhagic stroke is caused by the rupture of a cerebral blood vessel, which most often occurs against the background of a significant and sharp increase in blood pressure. Such ruptures are predisposed to:
- vascular anomalies (congenital aneurysms, miliary aneurysms);
- destruction of the vascular wall caused by the inflammatory process occurring in it (vasculitis).
Much less often, the development of hemorrhagic stroke is caused by diapedetic, i.e., bleeding that appears as a result of increased permeability of the vascular wall, and not a violation of its integrity (10-15% of cases). The pathological mechanism of this form of bleeding is based on disturbances in vasomotor reactions, which first lead to a prolonged spasm of the blood vessel, followed by its pronounced dilatation, i.e., expansion. This process is accompanied by an increase in the permeability of the vascular wall, as a result of which the formed elements of blood and plasma begin to sweat through it into the medulla.
The reasons leading to the development of hemorrhagic stroke are:
- arterial hypertension;
- cerebral aneurysms;
- arteriovenous malformation of the brain;
- vasculitis;
- amyloid angiopathy;
- hemorrhagic diathesis;
- systemic connective tissue diseases;
- therapy with anticoagulants and/or fibrinolytic agents;
- primary and metastatic brain tumors (as they grow, they grow into the walls of blood vessels, thereby causing their damage);
- carotid-cavernous fistula (pathological connection between the cavernous sinus and the internal carotid artery);
- encephalitis;
- hemorrhages in the pituitary gland;
- idiopathic subarachnoid hemorrhages (i.e., those hemorrhages in the subarachnoid space of the brain, the cause of which cannot be determined).
The following factors can enhance the damaging effects of the above reasons:
- excess body weight;
- long history of smoking;
- alcohol abuse;
- drug addiction (especially the use of cocaine and amphetamines);
- lipid profile disorders;
- chronic intoxication;
- hard physical labor;
- prolonged nervous overstrain.
The focus of hemorrhage in 85% of cases is localized in the cerebral hemispheres, much less often in the brain stem. However, such an atypical localization has an extremely unfavorable prognosis, since the respiratory and vasomotor centers, as well as the thermoregulation center, are located in this area.
In cases where the hematoma formed during hemorrhage is located deep in the brain tissue, it disrupts the cerebrospinal fluid and venous outflow. As a result, cerebral edema increases, leading to increased intracranial pressure, displacement of brain structures and the development of vital dysfunctions.
Pouring into the area of the basal cisterns, the blood mixes with the cerebrospinal fluid, which, in turn, causes the death of neurons, hydrocephalus and spasm of blood vessels.
Clinical picture
With intracerebral bleeding, more often than with cerebral ischemia, headaches, changes in mental state, convulsions, nausea and vomiting, and severe hypertension are observed. Due to the displacement of the structural brain by the hematoma, coma more often occurs in hemorrhagic stroke. But clinical signs are not enough to differentiate the type of stroke.
Symptoms of cerebral hemorrhage depending on their location
General cerebral signs of cerebral hemorrhage include nausea, vomiting, headache, impaired level of consciousness - signs of increased intracranial pressure. Seizures are more typical for hemorrhagic stroke and occur in 28% of cases during the first 24 hours. With cortical bleeding, memory is lost and intelligence decreases.
When the shell is damaged, severe disturbances of consciousness occur, plegia of the arms and legs on the side opposite to the affected hemisphere, and impaired sensitivity. If the dominant left hemisphere is damaged, aphasia develops. With hemorrhage in the right hemisphere, the patient does not realize the severity of the disease (anosognosia) and ignores the healthy right side of the body and space (hemiagnosia or niglect).
When an artery in the thalamus ruptures, there is an increased risk of coma and herniation of edematous tissue into the brainstem. With thalamic lesions, sensitivity is impaired, strabismus appears, and visual fields are limited.
When the cerebellum is damaged, dizziness, vomiting, gait disturbance and the inability to maintain a vertical position, uncoordinated movements, and paresis of the eye muscles occur. There is a risk of compression of the brain stem.
Left-hand side
Focal symptoms or neurological deficits depend on the specific area of the brain affected. With a left-sided hemorrhagic stroke, the following symptoms appear:
- hemiparesis of the right side of the body;
- loss of sensation in the right arm or leg;
- left eye dominance;
- limitation of the right field of vision;
- aphasia;
- niglect (not typical for lesions of the left hemisphere).
Characterized by impairment of logical thinking and mental state disturbance.
Right side
Right-sided hemorrhagic stroke is a lesion of the non-dominant hemisphere, leading to the following symptoms:
- left eye muscle disorder;
- hearing loss;
- violation of spatial perception of the left side (limb position);
- depression or aggression;
- poor color perception.
Right-sided lesions occur in almost 60% of cases and are accompanied by drooping of the left corner of the mouth and eye.
Symptoms of cerebral hemorrhage
Hemorrhagic stroke has a fairly characteristic clinical picture, but it can vary depending on the location of the bleeding. This is worth paying special attention to.
Clinic of subarachnoid bleeding:
- acute onset;
- intense headache - a “blow to the head”, and then a feeling of “warming” inside;
- nausea, vomiting;
- motor excitement of varying degrees or, conversely, loss of consciousness;
- photophobia;
- visual impairment;
- convulsive seizures.
Hemispheric hemorrhages are characterized by the following symptoms:
- occur acutely, often during physical exertion, reminiscent of a “blow to the head”;
- possible psychomotor agitation or the development of an epileptic seizure;
- the face is purplish-red or, on the contrary, sharply pale;
- hemiplegia (complete loss of voluntary movements in the leg and arm on one side) with low tone of paralyzed muscles;
- when raised, paralyzed limbs fall like whips;
- deep reflexes are not evoked;
- the nasolabial fold on the affected side is smoothed, the corner of the mouth is lowered, and the cheek “sails” when breathing;
- often vomiting;
- breathing problems (intermittent breathing);
- involuntary urination and defecation.
With stem hemorrhages the following are observed:
- respiratory and cardiac disorders;
- motor and sensory disorders, possible paralysis of all limbs;
- trembling of the eyeballs;
- inability to speak and swallow.
Clinic of hemorrhage in the cerebellum:
- dizziness with a feeling of rotation of surrounding objects;
- headache in the back of the head, sometimes pain in the neck and back;
- repeated vomiting;
- rigidity (stiffness) of the neck muscles;
- decreased or absent muscle tone;
- ataxia - movement coordination disorder;
- trembling of the eyeballs.
Clinic of ventricular hemorrhages:
- rapid deterioration of condition, up to deep coma;
- bloody vomiting;
- increased body temperature;
- hemiplegia is combined with motor restlessness in non-paralyzed limbs - they pull the blanket over themselves, “swatting away flies”;
- hormetonic syndrome (from the Greek horme - impulse, tonos - tension), which is expressed in periodically repeated severe tonic muscle spasms of paralyzed limbs.
Features of stroke in a child
Many people believe that stroke only affects adults. This is, of course, a myth. Children are also susceptible to pathology. According to some data, there are approximately six sick children per hundred thousand healthy children. They mainly experience:
- unexpected occurrence of hemiparesis (weakening of the muscles of one half of the body);
- sudden development of hemiplegia;
- problems with swallowing;
- crying, whims;
- frequent falls due to inability to maintain balance;
- tension in the muscles of the neck and back.
Hemorrhagic stroke - video
Diagnosis and differential diagnosis
Hemorrhagic stroke develops rapidly against the background of physical activity or stress. There may be warning signs of hemorrhage in the form of a headache and flushing of the face. Hemorrhagic stroke is characterized by prolonged coma, increased temperature and blood pressure, wheezing, and lack of pupillary response. Muscle tone is quickly disturbed, sometimes contractures occur early - increased reflexes.
The patient begins to vomit, have problems urinating, and movement of the eyeballs. A blood test reveals an increase in white blood cells, and in the urine - red blood cells, protein and glucose.
Epidural hemorrhage is more common in cases of traumatic brain injury, but blood in the cerebrospinal fluid is detected in subarachnoid hemorrhage in any case. Its appearance indicates damage to the cerebellum and pons during a hemorrhagic stroke.
To diagnose subarachnoid hemorrhage, the HUNT scale is used, which determines the degree of damage from 0 to 5. An increase in the degree of damage correlates with an increase in meningeal and cerebral symptoms: headache, stiff neck, disturbances of consciousness, stupor, autonomic disorders up to coma and agony .
Computed tomography of the brain
Confirmation of the diagnosis is possible only using visual methods:
- computed tomography determines the size of the hemorrhage, both in the subarachnoid space and in the parenchyma. The method detects tissue edema, ventricular hemorrhage and hydrocephalus;
- Magnetic resonance imaging is necessary to detect small hematomas in the structures of the hindbrain (pons, medulla oblongata), arteriovenous malformations without the use of contrast, unlike CT.
Hemorrhagic stroke on CT in the first hours is visualized using a dense clot.
Treatment and rehabilitation after hemorrhage
How to recover from a cerebral hemorrhage? This disease requires long-term rehabilitation to return to a normal, familiar life. Let's look at what you need to do to improve your well-being.
Recovery can also be done at home, if the process is monitored from time to time by the attending physician.
Rehabilitation can be roughly divided into several stages:
- First stage. It begins from the moment of the attack and lasts 1 month. During this period, drug therapy, positional treatment, massages, and passive gymnastics are carried out;
- Second phase. Early recovery, its duration is from 2 to 6 months;
- Third stage. Late recovery lasts from 6 months to 1 year. During this period, forces are aimed at restoring movements and returning the functions of the musculoskeletal system. At the third stage, the dynamics towards recovery are most visible;
- Fourth stage. It occurs 1 year after a hemorrhagic stroke. If the patient has not fully recovered, he continues to carry out rehabilitation measures in the complex. The emphasis is on exercise therapy.
With the help of medications
Drug therapy is an integral part of rehabilitation after a stroke. The surviving neurons after an attack take on the functions of the destroyed ones.
Therefore, they require additional recharge, since the load on them increases significantly. To normalize the condition at an early stage of recovery in a hospital setting, the following medications are prescribed:
- Nootropics - Piracetam, Cerebrolysin, Gliatilin, Actovegin, their analogues;
- Medicines to improve neuromuscular conduction - Proserin, Neuromidin, etc.;
- B vitamins - Milgamma, Neurorubin.
The patient receives all these medications in the form of injections.
Important! After discharge from the hospital, the patient continues the course of drug treatment. But the drugs can already be taken in tablet form.
With the help of physical therapy
The basis of therapeutic exercises is the appropriate position of the body, active and passive gymnastics. If the patient is completely immobilized, he must be turned over regularly to avoid stagnation. This will improve his blood circulation and metabolism.
When the patient can move the limbs independently, exercises should be done to strengthen the muscle tissue. To begin with, it is simply raising and lowering an arm or leg. Then you need to start more complex exercises in a sitting position.
When the patient can already sit down independently, it is necessary to begin gymnastics while standing. It will help restore coordination of movements.
Important! Exercise therapy is the main method of rehabilitation after a stroke. If you regularly perform therapeutic exercises, the patient will get back on his feet more quickly.
We invite you to watch a useful video on the topic:
Massage
If a patient has paralyzed upper and lower limbs, he cannot do without massage procedures. Therapeutic procedures are performed 3-4 weeks after the stroke.
You should start in a gentle mode, gradually moving to more intense kneading. Massage helps improve blood circulation and neuromuscular conduction.
Speech therapist
In cases where the patient has problems with speech, exercises are required to restore articulation.
First, a person learns to pronounce vowels, then syllables, and short sentences. If such manipulations do not give a positive result, the help of a speech therapist is necessary . This specialist will conduct a course of treatment to allow the patient to speak again.
Mind and memory training
In order for the patient to return to the usual rhythm of life, it is necessary to restore memory. The following exercises are suitable for this:
- Finger games. Fine motor skills help improve brain activity. To do this, you can bend your fingers and count at the same time, sort through small objects, clap your hands;
- Game of cities. This children's game is very useful during rehabilitation after a stroke. Especially if you remember the cities in which the patient was;
- Memories of funny, touching, positive moments from the patient’s life. In this case, under no circumstances should you mention the events that preceded or caused the disease;
- Ask questions about the weather, about hobbies. The patient will not respond quickly at first; you need to be patient.
Important! The memory mechanism is very complex. Sometimes, in order to remember some events, it is enough to mention some minor detail.
Partial or complete memory loss is a serious test for both the patient and his loved ones. Only patience and hard daily work will help restore your mind and memory.
Diet
Adjusting nutrition during a hemorrhagic stroke is not only a way to maintain physical strength, but also one of the ways to fully recover. The diet helps not only with rehabilitation, but also as a preventative measure for recurrent strokes.
Eating after an attack involves dosing food - you need to eat often (5-6 times a day), but in small portions.
Important! Under no circumstances should you overeat!
The basis of your daily diet should be the following foods:
- porridge;
- vegetable dishes;
- fruit desserts;
- lean meat;
- dairy and fermented milk products with a low fat content.
In this case, the daily intake of liquid should be about 1 liter, salt - 4-5 grams, calorie content - up to 2700 kcal.
It is completely necessary to exclude from the diet foods and drinks that have a stimulating effect on the cardiovascular and central nervous system. These include:
- alcoholic drinks;
- strong tea;
- coffee;
- spicy and highly salty dishes;
- spices.
The principle of eating after a hemorrhagic stroke generally does not differ from the main points of proper nutrition.
Complication of intracerebral hemorrhage
A cerebral hemorrhage that occurs means that the consequences of a hematoma will occur for two weeks. The main complications of hemorrhagic stroke are cerebral edema, compression of the brain stem and vasospasm.
A sign of edema is considered to be impaired consciousness: the patient is often in an unconscious state, falls into a stupor, or coma. Osmotic diuretics are used to correct edema.
Vasospasm develops within a week after hemorrhage due to the release of serotonin and other substances. It is manifested by an increase in drowsiness, visual impairment, speech, and logic. Calcium antagonists are used to reduce vascular spasm.
When hemorrhages into the ventricles of the brain, they stretch and ischemia of the surrounding tissues. Necrosis develops in the hypothalamic ganglia, cells of the caudate nucleus and thalamus. The nuclei of the cranial nerves, the hypoglossal and the vagus, die. Surviving patients are unable to speak or swallow.
What diseases can it be associated with?
Hemorrhagic stroke is a spontaneous hemorrhage in the brain, but its occurrence is always preceded by underlying diseases of the cardiovascular system:
- atherosclerosis,
- amyloid angiopathy,
- arterial hypertension,
- aneurysms and vascular malformations of the central nervous system,
- erythremia,
- thrombophilia,
- vasculitis,
- systemic connective tissue diseases.
In the acute period of hemorrhagic stroke, decompensation of previously existing somatic complications is highly likely:
- pneumonia,
- dysfunction of the liver and kidneys,
- diabetes
Due to the immobility of the patient, pulmonary embolism poses a great danger.
Therapeutic measures
Treatment of patients with acute cerebral hemorrhage is based on life support of the body, reducing bleeding, seizures, arterial and intracranial pressure. In emergency care, three types of drugs are used: anticonvulsants, antihypertensives, and osmotic diuretics.
Therapy begins with stabilization of vital signs. Endotracheal intubation is performed for patients in a coma, and artificial ventilation . If high intracranial pressure is suspected, hyperventilation is performed.
Conservative treatment
Blood pressure is reduced to safe numbers - in the range from 170 to 130 mm Hg. for diastolic and 120 to 185 mmHg. Art. for systolic. This will avoid vasospasm.
Blood pressure is controlled with beta blockers, calcium antagonists, and ACE inhibitors. Phenobarbital is used against epileptic seizures, and diazepam is used for emotional manifestations.
To stop bleeding and strengthen the walls of blood vessels, etamsylate, antiprotease drugs, calcium gluconate, rutin, and ascorbic acid are administered. Therapy is used to prevent thrombosis with gamma-aminocaproic acid and colloidal dextran solution for better brain microcirculation.
Neurosurgical intervention
Hemorrhagic stroke and hemorrhage in the membranes of the brain require surgery as the main type of treatment. The persistence of a hematoma in the cerebellum, thalamus and temporal lobe can lead to death, therefore removal of hematomas, where possible, is mandatory. The operation is performed within the first 24-48 hours if the hemorrhage occurs due to a ruptured aneurysm. The vessel is clipped, sutured with muscle, or the internal carotid artery is occluded inside the skull. The operation can quickly reduce the size of the hematoma, cerebral edema and the risk of herniation.
Rehabilitation and nursing
The patient is in the intensive care unit until hemodynamic parameters stabilize. Current practice emphasizes early verticalization of patients, even those who are intubated. What are special beds used for?
Care involves preventing cerebral edema by raising the head end of the bed. Anti-decubitus beds are used with pillows placed in the most vulnerable areas. The nurse constantly changes the position of the patient's body, using positioning techniques to prevent contracture.
Rehabilitation begins from 5-7 days, depending on the patient’s condition and the severity of the disorders, and it continues for a long time. After the intensive care unit and neurological hospital, it is preferable to send the patient to a rehabilitation center, where they are taught to dress, wash, and eat. A psychologist, occupational therapist, and physiotherapist also work there.
Is it possible to prevent hemorrhage?
Although hemorrhagic strokes occur less frequently, their risk factors can also be calculated and reduced:
- Learn to monitor your blood pressure daily, record your readings, and take medications prescribed by your doctor.
- Avoid fatty, fried foods, simple carbohydrates, and excess sugars. Eat more vegetables, fruits, nuts, fish.
- Take essential omega-3 fatty acids, vitamin E. use the amino acid glycine for severe emotional stress.
- Pay attention to physical activity: walk 30-40 minutes daily, dance, ride a bike. However, if you have high blood pressure, which increases in response to intense physical activity, avoid lifting weights and jumping.
- Quit smoking, limit alcohol consumption. Introduce new healthy habits: meditation, diaphragmatic breathing.
Be sure to consult a doctor to monitor blood counts, blood pressure, and the condition of internal organs.
Consequences and prognosis
Patients in coma are on ventilators. The prognosis depends on the degree of damage to vital functions. It is believed that if swallowing is preserved, the prognosis is favorable. Long-term rehabilitation is required, primarily aimed at restoring the ability to swallow, breathe, and speak (communicate needs). According to statistics, about 80% of stroke victims constantly need help from doctors and rehabilitation specialists. The level of disability reaches 25%, and only 10% of patients return to their previous lives.
Prevention
Drug prevention of stroke involves managing blood pressure. Antihypertensive drugs work in two ways: they open blood vessels or reduce the force of cardiac output. Therapy is selected individually depending on age and concomitant diseases.
Patients with diabetes must monitor their blood sugar levels with a glucometer and follow a diet. At the first signs of cognitive decline, a neurologist may recommend angioprotectors for blood vessels and microcirculation correctors in brain tissue.
Forms of the disease
Depending on the location of the hemorrhage, the following types of hemorrhagic strokes are distinguished:
- subarachnoid - bleeding comes from the vessels of the arachnoid membrane, blood flows into the subarachnoid space (i.e., the space between the arachnoid and soft membranes);
- intracerebral - the hematoma is located in the thickness of the brain tissue;
- ventricular - blood enters the cerebral aqueduct or ventricles;
- mixed - combines characteristics of two or more species.
The location of the hematoma in a certain anatomical region of the brain is accompanied by the appearance of specific symptoms, which in some cases makes it possible to determine its location during the initial examination of the patient.
The focus of hemorrhage in 85% of cases is localized in the cerebral hemispheres, much less often - in the brain stem
According to etiology, hemorrhagic strokes are divided into two types:
- primary - hemorrhage occurs as a result of microangiopathy (thinning of the walls of blood vessels). During a hypertensive crisis, when blood pressure suddenly and significantly increases, the thinned section of the artery cannot withstand it and ruptures;
- secondary - bleeding occurs as a result of rupture of an acquired or congenital malformation of cerebral vessels.