Craniotomy during a stroke often becomes the only way to save the life of a patient with a hemorrhagic form of pathology. The disease is accompanied by intracranial hemorrhage, which occurs due to damage to the artery. The hematoma has various sizes, it compresses the surrounding tissues, causing severe neurological disorders. For large hematomas, surgical treatment is prescribed.
Indications and contraindications for
Craniotomy refers to emergency surgical interventions that are performed for:
- increased intracranial pressure;
- pronounced swelling of brain tissue;
- the presence of large hematomas;
- thrombosis and atherosclerosis of cerebral arteries;
- the presence of malignant tumors;
- the addition of infections and inflammatory processes;
- the need for tissue sampling for histological examination.
In some cases, the operation is dangerous to the health and life of the patient. The list of contraindications to craniotomy includes:
- severe arterial hypertension;
- operations in the intracranial space undergone during the last 6 months;
- decompensated acute and chronic heart failure;
- severe diseases of the central nervous system;
- old age (in this case, surgery is performed only for life-threatening conditions that are not amenable to drug therapy);
- exacerbation of chronic diseases of internal organs;
- late stages of oncological pathologies;
- purulent lesions accompanied by soft tissue necrosis.
Craniotomy for stroke: indications, preparation, rehabilitation
A stroke is a serious disorder of cerebral circulation with rupture of a vessel, causing bleeding.
This pathology leads to dangerous disorders of brain function, but the worst thing is the consequences of hemorrhage that forms a hematoma - possible disability and even death (if medical assistance was not provided within 6 hours). Treatment with conservative methods is usually impossible, therefore, in order to help the patient and prevent the hematoma from enlarging, a decision is made to undergo surgery. In particular, if a person has a hemorrhagic stroke, then craniotomy is considered the only way to save him.
What are the indications?
Craniotomy (French - trépanation, Latin - trepanatio) is an operation that involves opening the skull to provide access to hematomas in the brain area with their subsequent removal. Timely and correctly performed surgery reduces intracranial pressure. In 85%, the prognosis after trepanation is favorable.
Craniotomy is indicated for stroke in the following cases:
- infectious processes, inflammation in the brain;
- traumatic brain injuries;
- oncology;
- presence of blood clots;
- increased intracranial pressure;
- serious problems with blood vessels;
- the need to obtain brain tissue for biopsy.
Surgery for a cerebral stroke is performed by a neurosurgeon. Its success depends on the professionalism of the doctor and the availability of high-quality specialized equipment.
Preparation and stages of the operation
During the preoperative period, the patient is required to undergo a number of studies: chest x-ray, blood test, MRI, ECG. Also, the doctor should be aware of the patient’s allergies of various etiologies.
Non-steroidal anti-inflammatory drugs and blood thinners are not taken before surgery.
It is extremely important that at least 14 days before craniotomy, the patient completely gives up bad habits - smoking and alcohol.
The day before surgery, food intake is excluded, blood pressure readings are carefully monitored, and personal sensations are monitored.
What actions does the operation contain:
- Administration of anesthesia, insertion of lumbar drainage, removal of cerebrospinal fluid.
- An incision in the skin to gain access to the skull, scraping the skin from the bones of the skull. If this is not done, the remains of the dermis will fall into the open cranium.
- Treatment of the head with an antiseptic preparation along the hairline.
- Opening the skull: drilling several holes to gain access to the brain. The pieces of bone obtained by drilling are placed in a separate container - after the hematomas are removed, they are put in place.
- Removing blood stagnation, stitching together burst vessels, stopping bleeding. Screening monitors the patient's vital signs.
- Restoring the structure of the skull with missing parts.
- Completing the operation.
The surgical process takes 3-4 hours, but sometimes the operation can last up to 8 hours - it all depends on the stage of the pathology.
Risks of complications
Craniotomy is a complex operation that involves certain actions on the brain. It is impossible to guarantee a favorable outcome of a surgical intervention, since this is influenced by many factors: the individual characteristics of the body, the extent of the stroke, the patient’s age, and concomitant pathologies that occurred even before the operation.
The so-called risk group includes patients who have: diabetes mellitus, cardiovascular diseases, atherosclerotic formations, excessive accumulation of fatty deposits. Possible complications include general and surgical ones.
Experts include the second type of complications:
- infection of brain tissue;
- heavy internal bleeding or local hemorrhage;
- cerebral edema;
- mechanical trauma (damage to brain tissue, blood vessels with surgical instruments);
- epilepsy;
- paresis, paralysis;
- disorders of the central nervous system - memory impairment, absent-mindedness, slurred speech.
General complications, expressed in deterioration of health (vomiting, intestinal upset, critical weight loss, dizziness), develop after surgery, when the patient recovers from anesthesia and gradually returns to normal life. Patients who have had to undergo craniotomy, which is a serious operation, often experience a stressful state.
Who should not undergo surgery?
After an attack, a person needs a lot of time for rehabilitation. At this time, the body is still very weak, and surgery after a stroke doubles the load on it, which can lead to a relapse. For example, cataract removal should be carried out no earlier than six months after the end of a stroke; preference should be given to laser surgery rather than ultrasound.
Despite the effectiveness of craniotomy proven by medical practice, there are a number of contraindications that do not allow this operation to be performed. These include:
- hypertension;
- the time interval between heart attack and stroke is less than 6 months;
- congestive heart failure;
- progressive brain diseases;
- poor blood clotting;
- renal and liver failure;
- old age - after 70 years (not in all cases a reason for refusal to undergo surgery);
- malignant tumor;
- acute phase of inflammation accompanied by the formation of pus;
- neurological deficit.
Trepanation is prohibited if the patient is in a coma.
Rehabilitation
After the operation, trepanned patients are transferred to intensive care, where medical personnel monitor the functions of vital organs.
Particular importance is attached to the condition of the discharge through the drainage and the holes of the resection trepanation.
The appearance of a postoperative hematoma and increased cerebral edema may be indicated by swollen facial tissue, bruises and bruising around the eyes.
If the postoperative period is successful, the patient can be transferred to the neurosurgery department on the second day, where he will remain for up to 2 weeks.
After craniotomy, deformation of the skull and the formation of a colloidal scar may be observed (if tissue regeneration processes are disrupted). These phenomena are eliminated by surgical correction.
Recovery after surgery should include adequate drug treatment, elimination of neurological disorders, social and occupational therapy of the patient. Physical therapy classes (kinesitherapy) are required.
To improve the healing of sutures, you need to provide high-quality wound care every day and promptly change the dressing. Hair can be washed no earlier than 2 weeks after surgery, depending on the condition of the stitches.
Patients often experience severe pain in the head, for which analgesics are prescribed. For seizures, anticonvulsants are indicated, and for anxiety, sedatives.
If different parts of the brain are affected, patients often have to be re-taught to speak, walk, and help with memory restoration. Close people play a huge role. It is they who, in the first time after surgery, will help the patient cope with some inconveniences in everyday life, for example, taking water procedures, preparing and eating food.
Physical activity is excluded during the rehabilitation period; the patient must be provided with complete peace in psycho-emotional terms.
Disability after surgery is not always assigned, since craniotomy is not a reason for this.
If a person feels well and recovers quickly, then after a while he may well return to his usual lifestyle, going to work.
If he has complications, for example, in the form of neurological pathologies that limit life activity, then the issue of disability can be considered by a special commission consisting of different specialists.
Source: https://GolovaUm.ru/zabolevaniya/udar/trepanatsiya-cherepa-pri-insulte.html
Preparation
Preparation for trepanation for hemorrhagic stroke includes:
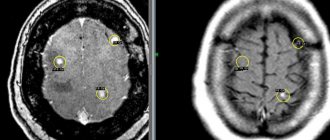
- Examination. Before the operation, blood and urine tests are taken. The qualitative and quantitative composition and blood clotting are assessed, signs of inflammatory diseases that can become contraindications to intervention are identified. Indications for surgery are determined using CT or MRI of the brain. An ECG is performed to assess the functions of the cardiovascular system.
- Refusal to take medications. 2 weeks before the procedure, the attending physician discontinues medications that can cause postoperative complications. These include anticoagulants and antiplatelet agents that reduce blood clotting. On the day of the procedure, stop taking all medications.
- Refusal to eat the day before the intervention. On the day of surgery, drinking liquids is not allowed.
- Consultation with a neurosurgeon. The doctor tells the patient about the chosen treatment method and possible risks. At this stage, the medical history is studied.
Important information: What to do and how to treat headaches after a stroke
Restoration activities
Craniotomy for stroke is necessary to prevent the development of complex pathologies and brain diseases. The recovery period should help the patient return to normal life.
Restoration measures allow:
- eliminate the consequences of craniotomy;
- prevent the development of any complications;
- restore all vital functions of the body as quickly as possible.
The recovery process must proceed according to a certain pattern: the actions will depend on the type of trepanation. The sutures are removed after about 10 days, and the patient can be sent home.
But in the hospital the patient’s recovery is already beginning:
- Medicines are used to relieve pain. Therapy will also be needed to prevent any infection from developing.
- The functioning of all brain functions must be checked.
- Wounds are treated with antiseptics and dressings are performed regularly.
- And the prevention of various diseases is also important.
In this case, medications must be prescribed that can improve bleeding through the vessels. All medications are prescribed only by a doctor. He also recommends carrying out all restoration measures.
How is trepanation done?
Depending on the size of the lesion and the general condition of the patient, the operation can take from 5 to 10 hours. The surgical plan includes the following steps:
- Patient preparation. Drugs for general anesthesia are administered intravenously, after which the trachea is intubated. The patient's head is fixed using a special device that holds the skull in an upright position. This allows you to completely immobilize the operated area during surgical procedures. At the same stage, a lumbar drainage is installed, which is necessary to drain the cerebrospinal fluid. Sometimes cerebrospinal fluid pressure is reduced with medication.
- Skin incision. The surgical wound lies along the hairline. They try to minimize the risk of cosmetic defects after the intervention. The skin flap is separated from the cranial bones.
- Opening the skull. A drill makes several small holes. Using a medical saw, a bone flap of the required size is cut out. It is stored throughout the surgical procedure for the purpose of subsequent return to its place.
- Gaining access to the medulla. The surgeon puts on glasses with an operating microscope, and then makes an incision in the dura mater. The organ is tightly compressed by the skull, so it is impossible to move its tissues. To perform manipulations, the neurosurgeon uses thin instruments inserted into the thickness of the brain. The focus of necrosis or hematoma is removed, the intervention is combined with constant monitoring of the condition of the cranial nerves and the cardiovascular system.
- Closure of the skull defect. The cut bone flap is returned to its original position or fixed with metal staples. The surgical wound is sutured, after which a sterile bandage is applied.
Important information: What are the prognosis for recovery after ischemic stroke of the brain stem?
Why is surgery needed after a brain injury?
Surgery is indicated in the presence of hemorrhage. Efficiency does not always occur, and in addition, the localization of the source of the stroke does not allow surgery in all cases.
Indications for surgery are the following conditions:
- Cerebellar stroke, the focal lesion of which is above 3 cm. Especially if the neuralgic changes progress, and there are also signs of cerebral edema or compression;
- The presence of hemorrhage on the surface of the cortex;
- Pouring of blood into the cerebral ventricles;
- Brain swelling;
- Coma, from which the patient does not recover for more than 6 hours;
- Vascular pathologies with bleeding.
The following types of operations are carried out:
- Aneurysm clipping. Performed when an aneurysm ruptures. A catheter is inserted through the artery in the thigh, and the aneurysm is fixed with clips;
- Trepanation of the skull. It is rarely indicated for cases of large hemorrhage and hematoma pressure on the brain, leading to severe headaches, high blood pressure and fainting. This method is used when there is a clear threat to the patient’s life and when stroke recurs. During this procedure, the skull is opened, the surgeon removes the accumulated blood, and then the removed part of the bone can be replaced with screws or a plate. If the lesion is large, decompression trepanation is prescribed - part of the skull is removed, which reduces the pressure on the undamaged areas of the brain;
- Carotid endarterectomy. It is carried out for frequent ischemic attacks, as well as for diagnosing vessel narrowing;
- Selective thrombolysis. A catheter is inserted through a large artery, and a special thrombolytic is administered through it - a drug that dilutes the blood clot and removes it from the vessel;
- Stenting. Most often, this operation is performed to prevent recurrent strokes.
Read also: Standard of care for stroke patients
Consequences
Craniotomy after a stroke can cause the following complications:
- intracranial bleeding;
- swelling of brain tissue;
- epileptic seizures;
- addition of bacterial infections;
- injury to tissue or blood vessels of the brain;
- complete or partial paralysis of the limbs;
- speech disorder;
- memory impairment;
- disruption of the processes of memorization and perception of new information;
- severe headaches, nausea and vomiting (in the early postoperative period, pain is eliminated with narcotic analgesics);
- the presence of a cosmetic defect associated with the removal of a bone flap (cranioplasty helps solve this problem);
- dysfunction of the digestive and respiratory systems;
- muscle weakness.
Rehabilitation after trepanation includes:
- stay in the intensive care unit (during the first 2 days you need to monitor the performance of the brain and heart);
- care of the surgical wound (the bandage is changed daily, the wound is treated with antiseptic solutions, the sutures are removed after 10-14 days);
- following a special diet (the patient should eat easily digestible foods that do not interfere with intestinal motility);
- exercise therapy (helps avoid stagnation of blood and lymph caused by prolonged immobilization);
- drug therapy (at this stage, nootropics and neuroprotectors are used that normalize brain functions).
Disability after craniotomy is assigned in the presence of severe consequences of a stroke and the operation itself.
Surgical treatment of stroke - is there an alternative?
Since the consequences of a stroke are often irreversible, sometimes only surgery can save the patient's life. One of the most common methods of surgical treatment of stroke, helping to stop bleeding or restore blood supply (in severe ischemic strokes) is craniotomy, or craniotomy, a complex operation that requires special equipment and experienced doctors.
It is craniotomy that is often the only way to give a person a chance to recover and return to normal life.
Before surgery, the following mandatory studies are carried out:
- duplex ultrasound scanning;
- computer or magnetic resonance imaging of the brain;
- angiography.
They allow you to accurately determine the location of the hematoma, its size, and the presence of plaques. And also assess the current state of blood flow, which ultimately helps the neurosurgeon determine the scope of the operation. It is worth understanding that a large hematoma will not resolve on its own, and if it is not promptly removed by craniotomy, the outcome will most likely be fatal.
Craniotomy after stroke consequences – HealthStep
In neurology, there are a number of conditions in which direct access to the patient's brain is necessary to help the patient. For these purposes, craniotomy is performed - a complex surgical procedure. Historians have found a lot of evidence that the procedure was carried out by doctors even before our era.
Due to the lack of knowledge of anatomy and asepsis, such experiments usually ended in death. Today, craniotomy, as well as its consequences after surgery, have been carefully studied. This made it possible to reduce the incidence of complications to a minimum, but the procedure is still considered one of the most dangerous in medicine.
Surgical intervention
Trephination is a surgical procedure in which a hole is created in the skull. This is routinely performed to gain access to the brain and further work with the organ.
Urgent manipulation is indicated in situations where there is a risk of compression of the organ and disruption of its function. For example, such an operation is often performed for hemorrhagic stroke and other life-threatening emergencies.
Considering the degree of risks when using the technique, it is used only if there are obvious indications. This is done in cases where other options for accessing the brain are not able to give the desired result or there are no conditions for their implementation.
Indications for surgery
Every year the number of options for non-invasive effects on the brain is growing. And yet there are a number of conditions in which opening the skull cannot be avoided.
Before prescribing a planned procedure, the patient is required to undergo a CT or MRI of the head, angiography or duplex ultrasound of the vessels.
This allows you to determine the location of the organ lesion with maximum accuracy and determine the working area.
Craniotomy is prescribed for:
- Hemorrhagic stroke - surgery after a stroke allows you to stop bleeding in a short time and prevent the formation of a hematoma;
- tumors, hematomas, abscesses in the brain;
- injuries to the skull, in which bone fragments begin to put pressure on the brain matter;
- abnormalities of the skull;
- cerebral aneurysm.
There are several options for craniotomy. The optimal one is selected depending on the specifics of the situation, the severity of the patient’s condition, and the availability of the necessary tools.
Contraindications to surgery
Trepanation is resorted to only when it is impossible to use more gentle techniques. Due to the specifics of the approach, prohibitions on performing open brain surgery are not absolute. The decision is made individually in each case. The neurosurgeon must compare the risks of inaction and dangerous intervention, and assess the general condition of the patient.
Relative contraindications to the procedure:
- the patient's age is over 75 years;
- the presence of organic pathologies in the stage of decompensation - renal, cardiac, liver or pulmonary failure, diabetes mellitus;
- violation of the blood clotting process;
- oncological and purulent lesions of other organs;
- coma or shock (if they are not indications for the procedure).
Even the listed conditions are rarely taken into account when manipulation is needed to relieve pressure on the brain. In any case, the neurosurgeon must take them into account in order to minimize the risk of negative consequences for the patient and increase his chances of recovery.
Several types of trepanation
The surgical procedure is performed in one of two ways. Decompression (resection) trepanation is the best option for dealing with emergency conditions.
Most often, a small hole is made in the area of the temporal bone to minimize damage to the brain and subsequently hide the scar. First, the surgeon cuts through the soft tissue with a scalpel.
He then uses a hand hammer and a wire saw to create the surgical opening.
Decompression craniotomy in case of injury, stroke, hematoma, or abscess can quickly reduce intracranial pressure and prevent compression of the brain. Often, after surgery, a bone defect remains, which is dealt with additionally.
Osteoplastic trepanation is not limited to a specific location. During the procedure, the neurosurgeon cuts out a large flap, which provides him with convenient access to the desired area. Once the surgery is complete, the tissue is placed in place to avoid any bone defect. This type of impact is more gentle. The rehabilitation process in this case is easier.
Carotid endarterectomy
Often, a concomitant cause of the development of cerebral catastrophe is atherosclerosis of the carotid artery. In some cases, prevention against such a background cannot be limited to conservative approaches. Here it is better to resort to surgical treatment of ischemic stroke.
Carotid endarterectomy involves making an incision along the carotid artery and removing the inner layer of the vessel along with the atherosclerotic plaque. The hole is then sutured or covered with a flap. This allows you to restore blood flow and prevent a brain catastrophe after a transient attack or a second stroke.
Before the procedure, the patient must undergo a CT scan of the head, angiography, and duplex ultrasound of the vessels.
Anesthesia
In most cases, open brain surgery requires general anesthesia. This allows you to keep the patient in a state of sleep and blocks any unpleasant sensations. In this approach, the solution chosen by the anesthesiologist is delivered through a system mounted on the shoulder or arm.
Sometimes a neurosurgeon needs to assess the patient’s condition directly during surgery. In this case, he is temporarily taken out of anesthesia, limiting himself to local anesthetics. When performing a targeted treatment, local anesthesia can be used.
It involves local treatment of the area undergoing surgery.
Rehabilitation after trepanation
Opening the skull rarely occurs without negative consequences for the body. After such an aggressive procedure, the human body is gradually restored to its original state. Often he needs professional help. The timing of the patient’s return to normal life depends on his age, the type of illness he suffered, the quality of the doctor’s work, and the general condition of the body.
Rehabilitation after craniotomy is aimed at:
- smoothing or eliminating the consequences of the operation;
- identification of risk factors and prevention of complications;
- fight against brain disorders;
- preventing recurrence of the original problem.
Regardless of the type of intervention, the first 10 days after surgery are considered critical.
During this period, the patient should not be overloaded. Everything is limited to specialized drug treatment, wound care and rest. Then the medication is supplemented with physical therapy, testing of brain functions, and gentle physical activity. If necessary, sessions with a psychotherapist are held.
What are the possible consequences of the operation?
The surgical technique is considered extremely aggressive and dangerous, but sometimes only it can save a person’s life.
Problems in the postoperative period may be associated with brain damage even before the patient receives help, violation of the rules of patient care, medical errors, or body characteristics.
There is a high probability of bleeding and the development of cerebral edema. A change in tissue structure is possible, leading to convulsions, paralysis, imbalance, and chronic fatigue.
Injury to certain parts of the brain is fraught with a decrease in the quality of vision, problems with memory, speech and the functioning of internal organs.
Infectious complication
The entry of pathogens onto the tissues inside the skull is practically impossible if the rules of asepsis are observed during the operation. Problems with a wound on the head arise much more often, but they can be quickly resolved with the help of quality care for the area.
There is also a risk of infection of internal organs: bladder, intestines, lungs. This occurs due to a forced change in the rhythm of life of the victim and limitation of his activity. Prevention of conditions is to follow a diet, conduct exercise therapy, and maintain a daily routine.
In extreme cases, antibiotics are used.
To follow the regime, download the daily routine diary.
Blood clots and blood clots
Restricted mobility and pathological biochemical processes in the body lead to the adhesion of blood cells and the formation of blood clots. Most often they form in the veins of the lower extremities. The rupture of such a formation and its rise through the bloodstream into the lungs, heart or brain can lead to the death of the patient.
The thrombus clogs the lumen of a smaller vessel, blocks the circulation of biological fluid, and provokes a malfunction of the organ. To prevent complications, the patient is given a massage, prescribed anticoagulants, placed on leg compresses and recommended to return to physical activity as quickly as possible.
Neurological disorders
Craniotomy can cause swelling of the brain tissue near the surgical site. This leads to the appearance of temporary neurological disorders, the type of which depends on the location of the manipulation.
Most often, as the swelling subsides, such signs disappear on their own. To speed up the process, patients may be prescribed steroid medications.
With deep and extensive violations of the tissue structure, symptoms can persist for several months and even become permanent.
Bleeding
During trepanation, a large number of vessels are damaged. For this reason, the wound may bleed for several days after the procedure.
To prevent complications against this background, the patient is given a drainage so that the biomass does not accumulate in the skull. Otherwise, it risks affecting motor centers or nerve fibers, leading to seizures.
If the bleeding does not subside, repeated surgery may be necessary to suturing or cauterizing the vessels.
Craniotomy is a complex and dangerous procedure, which in recent years has been attempted as rarely as possible.
Experts have developed a number of manipulation techniques depending on the indications. The use of one of them in a specific case allows you to minimize injury to brain tissue and reduce the risk of negative consequences. Compliance with the rules of postoperative rehabilitation is the key to the patient’s quick return to normal life.
Source: https://zdorovshag.ru/trepanacija-cherepa-posle-insulta-pos.html