In this article we will look at the types of cerebral stroke and their consequences.
Stroke in medical practice refers to conditions of various causes and mechanisms that lead to acute disruption of blood flow in the arterial and venous vessels of the brain. The patient with such failures experiences focal neurological disorders.
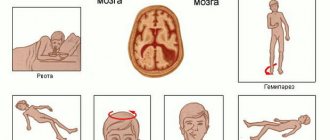
Types of cerebral strokes are classified depending on the localization, severity and prevalence of the process, and each of them is characterized by specific deviations in the functioning of the nervous system (vomiting, depression of consciousness, darkening of the eyes).
Types of strokes
To help the patient, it is necessary to accurately determine the type of cerebral stroke. In clinical practice, they are divided into two main types, which have different origins and require the use of different treatment regimens:
- Ischemic (cerebral infarction), which occurs due to exposure to factors that do not allow blood to pass freely through the vessels and supply brain cells with oxygen. Its development is possible after blockage, sustained and sharp spasm and narrowing of the lumen and occurs in approximately 85% of cases.
- Hemorrhagic stroke, which develops as a result of the release of blood from a vessel, the wall of which ruptures (not due to injury) and compresses the tissue, leading to its gradual death.
According to the severity of manifestations and type of course, strokes are classified into:
- Initial degree (minor stroke). Symptoms in this case manifest themselves in the form of neurological disorders and are moderate or insignificant. It disappears within a few weeks. It is observed in 13% of patients with a proven diagnosis.
- Mild or moderate. Signs of disorders disappear under the influence of medications. There are no symptoms of cerebral edema.
- Severe degree, which is marked by serious disorders of the functioning of the central nervous system. With such a deviation, the patient is most often unconscious and has extensive damage to all parts of the brain and swelling. Types of ischemic cerebral stroke are the most common.
If the disturbances last no more than a few hours, the phenomenon is called transient ischemic attack. This anomaly is considered a precursor to the possible development of more severe conditions. Its occurrence indicates the need for comprehensive therapy and prevention.
Types of cerebral strokes by developmental mechanism
In the International Classification of Diseases (ICD-10), cerebrovascular pathologies are allocated 10 subsections, of which 5 cover stroke directly (I60-I64). The types of pathology differ in the nature of its course, etiology, and treatment tactics used.
Based on the mechanism of development of the disease, there are 3 main groups:
- ischemic;
- hemorrhagic;
- transient ischemic attacks.
Each type is classified within the group, depending on the factors associated with the disease.
The division of pathology into hemorrhagic and ischemic is quite arbitrary, since with these two forms, foci of both types of strokes appear in the patient’s brain tissue. But based on the predominance of diagnostic criteria, priority is given to one of the types.
Correctly classifying the disease at an early stage is extremely important, since the choice of treatment method and prognosis directly depend on it.
Ischemic
Types of stroke related to ischemic are the most common (80% of cases).
The disease is common in people over 50 years of age against the background of concomitant pathologies: rheumatism, diabetes, cardiac dysfunction, and previous myocardial infarction. A separate category is migraine stroke, which is the result of regular paroxysmal headaches (migraines). This type is more common in women under 45 years of age.
The provoking factor is the occurrence of obstacles to free blood flow inside and outside the skull, which leads to metabolic disorders in brain cells. As a result, necrosis (ischemia) develops.
A person feels:
- weakness;
- headache;
- dysfunction of motor coordination;
- numbness in the arms or legs.
Classification of ischemic stroke includes types:
- Atherothrombolic - occurs with atherosclerosis of large and medium arteries. An obstruction to blood flow is created by a plaque that has clogged the vessel; the size of the necrosis focus can vary. Symptoms of the pathology increase gradually over several hours or days; the condition worsens at night. The disease is often heralded by a transient ischemic attack, and multiple microstrokes are possible.
- Cardioembolic - the culprit of the disease is cardiogenic embolism. It is caused by valvular heart defects, parietal thrombi formed in it, rheumatic or bacterial endocarditis, and atrial fibrillation. The embolic focus of necrosis is predominantly of moderate or large size, located in the middle artery of the brain. The cardioembolic type is characterized by a sudden attack in the daytime with severe neurological symptoms.
- Hemodynamic - formed when pressure decreases, as a result of which metabolic processes in the brain are disrupted. There is no blockage of the arteries. The cause may be a drop in cardiac blood volume due to bradycardia, ischemia, or vascular abnormalities. Localization of lesions is possible in any part of the brain.
- Lacunar - typical for people over 50 years of age. The causes are hypertension and embolism. The disease is provoked by damage to one of the small arteries (up to 10 cm long, up to 0.2 cm in diameter) connecting the large ones. The vessel is compressed by a lacunae, a formation filled with cerebrospinal fluid. The lesion up to 1.5 cm is localized in the subcortical layer. Symptoms increase slowly over several hours.
- Hemorheological microocclusion - the cause is dysfunction of blood clotting, when small vessels are blocked by blood clots.
And also read on our website: Pressure during a stroke - low, high or normal
The ischemic type is dangerous due to the gradual development of pathology. Periods of deterioration are followed by improvements in well-being. The attacks are repeated, resulting in paralysis in the patient.
Hemorrhagic
The pathology is caused by a ruptured vessel in the brain and hemorrhage, which is quite difficult to stop. The causes are predominantly cardiovascular pathologies.
Hemorrhagic and ischemic cerebral stroke - the difference between the concepts lies in the mechanism of development of the pathology. In the first case, the consequences are more severe than in the normal (ischemic) form. The difference between a hemorrhagic stroke is that it involves compression of the brain tissue by a hematoma formed during the flow of blood.
The pathology mainly occurs at the age of 45-65 years, and hypertension is often the cause. Sometimes the provoking factor remains unclear.
The peculiarity of the hemorrhagic type is its rapid development, which occurs when a person is under stress (physical or emotional), often during the daytime.
Hemorrhagic stroke is much less common than ischemic stroke, but the mortality rate is higher. Symptoms manifest themselves sharply: a feeling of a “blow to the head”, severe pain, increased pressure, facial paresis, prolonged loss of consciousness, hoarse breathing, hemorrhage in the eyes, paralysis of the limbs, vomiting.
Transient ischemic attack
The pathology is characterized by a brief disruption of blood circulation in individual areas of the brain, leading to hypoxia and cell death.
The difference between a TIA and a stroke is that during an attack there is no complete cessation of tissue nutrition. A small blood flow to the damaged area remains, the symptoms gradually subside (over the course of a day), and there is no progression of the pathology.
After the transient attack is completed, healthy cells take over the function of dead cells, and foci of necrosis do not increase.
There are types of transient attacks:
- Vertebrobasilar - occurs in 70% of patients. This type develops abruptly, often manifested by a sudden turn of the head to the side. Dysfunctions of vision, speech, and movement disorders occur.
- Hemispheric - this type is characterized by migraines, dizziness, loss of consciousness. The cause is changes in the cervical vertebrae.
- Spinal muscular atrophy (SMA) - damage to the carotid areas of the brain causes motor and sensory dysfunction. With ischemia in the right basin, the MCA develops on the left.
Sometimes, with a mild or moderate attack, the symptoms are mild - then a diagnosis of an unspecified type of TIA is made.
The difference between a stroke and an ischemic attack
Stroke differs from transient ischemia in that during it the symptoms last for a day, and sometimes even more, and the resulting disorder often leads to death.
In children, a type of congenital disorder of blood circulation in the brain occurs. Pediatric neurologists consider this a specific type of stroke, calling it metabolic. The main cause of this pathology is some diseases that occur with metabolic disorders. In this case, the symptoms of the underlying disease come first.
So, let's take a closer look at the types of brain strokes.
Stages of stroke by time
Temporal classification is based on the speed of biochemical reactions that occur in the cell of dead neurons. It is this that guides clinicians in choosing possible diagnostic methods.
The most acute period
This period lasts from the onset of the attack and during the first 6 hours. It is suitable for initiating thrombolysis and other interventional techniques. To determine the lesion, diffusion-weighted modes are used on MRI, MR angiography, and CTA. These studies make it possible to determine the presence of a lesion, the localization of a blood clot in the artery, and the possibilities of interventional therapy.
Acute phase
Lasts at least 24 hours from the moment of the attack. During this phase, a CT examination is performed to exclude hemorrhagic stroke. An ischemic lesion may not be visible on neuroimaging.
Given the late delivery and the impossibility of performing interventional techniques, other extensive examinations are not performed. Recommended MRI over time after 12-24 hours, monitoring of laboratory blood parameters, acid-base balance. The heart is examined to identify arrhythmias, fibrillation, and other cardiogenic complications
Subacute phase
Lasts from the first day to the first 6 weeks from the attack. Stroke can be detected by MRI. After 5 days, the lesion is visible in almost any scanning mode. Examination of brachiocephalic vessels, pressure monitoring, ECG, and general clinical examinations are required.
Chronic phase
At this stage, the focus of necrosis is replaced by connective tissue. Changes will be noticeable on CT and MRI. During this phase, the patient has already been discharged from the hospital and is undergoing rehabilitation. Changes in the visualization picture remain forever. It is important to distinguish them from “fresh” lesions during new attacks.
Ischemic stroke
This pathology is most often observed in elderly people, especially in the presence of certain chronic diseases associated with impaired vascular structure.
The risk group also includes people who have:
- diabetes;
- heart rhythm disturbances;
- bad habits;
- myocardial infarction;
- metabolic disorders;
- ischemic disease;
- rheumatism;
- hypertension;
- atherosclerosis;
- heart disease;
- thrombophlebitis.
Impaired blood circulation in an ischemic type of stroke leads to a cessation of the supply of nutrients and oxygen to brain cells. As a result, irreversible changes begin to occur in the nervous tissue of the brain.
I know almost all types of ischemic cerebral stroke. But there are others. More on this later.
Stages of diagnostics of the acute period
- Stage 1. The victim is urgently hospitalized. The doctor receives basic information from the words of the patient, his relatives or surrounding people. External signs of cerebral circulatory disorders, emotional background, physical stress, and blood pressure levels allow a diagnosis to be made fairly quickly and accurately. The patient's medical history is studied for the presence of other diseases that can provoke the development of ischemic stroke (arrhythmia, atherosclerosis, previous heart attack, etc.). However, the possibility of making an incorrect diagnosis exists in the case of an epileptic seizure, a brain tumor, a head injury, a hypoglycemic state, etc.
- Stage 2. The most important point of this stage is to quickly and accurately determine the nature of the disease. The tactics of first aid and further treatment will depend on this. A computed tomography scan of the brain is performed, since the clinical picture alone cannot provide completely reliable information.
- Stage 3. After a quick history has been collected, the clinical picture has been identified and a CT scan has been performed, the doctor begins to choose treatment tactics. The subtype of stroke is also determined (lacunar, atherothrombotic or cardioembolic, etc.). The correct choice of therapy will help not only provide timely assistance to the victim, including surgery, but also prevent a possible recurrence of a heart attack in the future.
Thrombotic stroke
Disruption of blood flow through the vessels in this variant of the development of pathology occurs due to the development of certain atherosclerotic changes, which are characterized by the appearance of plaque. A stroke develops in a few minutes or hours, and often appears at night.
The thrombotic type of this disease may be preceded by an acute attack of a transient attack. The symptoms of the pathology depend on the extent of the affected areas, and the attack itself depends on the caliber of the occluded vessel.
A condition is identified in which multiple thrombosis of the cerebral arteries is observed as a result of the appearance of disorders of the blood coagulation system. This anomaly is characterized by minimal neurological symptoms in combination with multiple microcirculation disorders.
We continue to analyze the types of brain strokes and their differences.
Consequences of an attack
Ischemic stroke causes behavioral changes and emotional disturbances that are difficult to recover from. Damage to brain tissue depends on the diameter of the vessel that was blocked by the clot and the time the patient spent before treatment.
Hemorrhagic stroke causes a complete imbalance of body functions - both physiological and mental. In most cases, a condition occurs in which a person loses the ability to self-care due to hemiparesis - loss of sensitivity in the muscles of the face and limbs. Characterized by a partial decrease in muscle tone on the opposite side of the body. In especially severe cases, complete paralysis is possible.
Soporous state
Stupor is a borderline state between confusion and coma. If left untreated, a coma may occur. The patient may be conscious, but poorly responsive, or unconscious. Contact with the patient is limited due to damage to the right-sided brain structures responsible for facial recognition.
Speech impairment after stroke
It manifests itself in two variants - lack of speech and impaired diction. Variations are possible - misunderstanding of your own speech, someone else's. Hearing his own speech, a person is not able to analyze what is said.
Brain swelling
May develop 2 days after the acute condition. Symptoms clearly manifest themselves on days 3–5. Requires treatment.
Convulsions
Dangerous manifestations of the disease, as they provoke repeated hemorrhage. May cause coma.
Headache
The nature of the headache varies depending on the type of stroke you suffered. With ischemic pain, the pain is less intense. In case of hemorrhagic, painkillers are required during the recovery period. If several months or years have passed since the attack, it is necessary to do gymnastics and massage to relieve tension headaches.
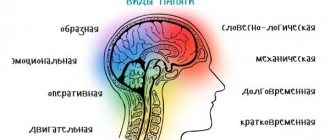
Memory loss
When the vessels of the temporal lobe are damaged, memory lapses or complete loss are observed. Psychiatrists are involved in the rehabilitation of such patients.
Paralysis
A complete lack of motor activity and reflexes occurs with central brain damage. One-sided or partial paralysis is possible, depending on the hemisphere of the brain or its part in which the circulatory disorder occurred. With peripheral paralysis, the overall tone decreases, but is not completely lost.
Coma
There are 4 degrees of coma:
- with the first, patients come to their senses after 2-3 hours;
- with the second, the patient has a chance of recovery if brain functions gradually stabilize
- in the third degree, the person is monitored by a device for artificial stimulation of vital signs;
- in the fourth case, brain disorders do not allow the patient to survive; most often such cases end in death.
Brain hemorrhage
Recurrent hemorrhage occurs in the first year in 1/3 of patients. If you do not follow the recommendations of your doctor and nutritionist, the risks increase. The mortality rate for a second attack is 70%.
Motor impairment
Decreased fine motor skills are observed in 70% of stroke survivors. The strength of the hands, the mobility of the joints, and the sensitivity of the fingertips are subject to restoration.
Aphasia
There are motor, sensory and semantic, in which a person pronounces words poorly, poorly understands other people’s words, speaks independently, but does not perceive what is said. Severe aphasia is a lack of understanding and absence of speech functions at the same time.
Peripheral neuropathy
Symptoms include muscle pain, decreased sensation and weakness. After an acute condition, the nerves are not affected, but lose connection with the brain and are difficult to control. Restore tone with gymnastics, massage, and physiotherapy.
Psychosis
Impaired perception of reality. Psychosis after a stroke progresses slowly. The first signs are aggression, short temper, suicidal thoughts, and lack of logical reasoning.
Visual impairment after stroke
Vision is restored, but not immediately if the area of neuronal damage is insignificant. Blockage of blood vessels leading to the organs of vision is treated in parallel with general therapy.
Central prosoparesis
The degree of damage to the facial nerve after a stroke - prosoparesis - is determined by the movements that a person can perform with the facial muscles. Severe degree is characterized by complete paralysis of facial muscles with the inability to close the eyes.
Cardioembolic stroke
The occurrence of cardioembolic ischemia occurs when the lumen of a vessel is occluded by a thrombus, which can form elsewhere in the body, but enters the cerebral parts with the blood flow. Most often, its formation occurs in the cavity of the heart. The occurrence of a blood clot can be triggered by the presence of valve defects, infective endocarditis, and the development of paroxysmal types of tachyarrhythmia.
This pathology develops sharply and suddenly and is characterized by rapidly occurring neurological disorders while the patient is awake. Lesions may be extensive or moderate.
Brain strokes often occur in older people. What type is it?
Causes of stroke
Strokes occur both due to lack of nutrition in a part of the brain and due to hemorrhage. When the lumen of a vessel is blocked by an atherosclerotic plaque, thrombus, or embolus, an ischemic stroke develops, but if the stroke was a consequence of damage to the vessel and hemorrhage occurs, it is called hemorrhagic. The time of diagnosis and which doctors provided assistance are also important - the earlier and more correct the assistance is provided, the more positive the outcome. To diagnose cerebral blood supply disorders, it is necessary to use stroke recognition techniques:
- When trying to smile, you need to pay attention to the corners of the mouth - in case of a stroke, it can be directed downwards, the smile looks crooked and asymmetrical;
- When trying to speak, it may be difficult to pronounce even the simplest words and sentences;
- When trying to raise both arms, asymmetry is observed;
- The protruding tongue falls to the side.
If at least one of the symptoms is positive, you must immediately call an ambulance.
Under no circumstances should you give him water, feed him, lift him, or take him by handy transport to the nearest hospital, as this can cause harm. In severe cases, there is a need for cardiopulmonary resuscitation on site or in an ambulance. Hospitalization in the event of a stroke is mandatory. As a rule, the patient remains in the intensive care unit until his condition is completely stabilized, with further transfer to the neurological department.
Treatment of stroke consists of a set of emergency actions and a recovery period, which takes quite a long time and is carried out in several stages. Treatment includes medications, physiotherapeutic procedures, and following the recommendations of related specialists. The characteristics of patient care are also important.
Lacunar stroke
This disease manifests itself in the form of a disruption in the functioning of small arteries with the formation of cavities (lacunae) located in the subcortical part of the brain. As a rule, the lesion is small in size and usually does not exceed 2 cm. The formation of a lacuna is accompanied by mild symptoms. The main reason for this condition is increased pressure in the blood vessels.
Among the main types of cerebral strokes, lacunar stroke is considered the most common and occurs in almost every fourth patient with a similar diagnosis.
The main danger of this pathology is the tendency to recur. Recurrence of circulatory disorders occurs in approximately 12% of cases of vascular accidents. This form of stroke is most often diagnosed in older people and in most cases causes death.
What other types of brain strokes are there?
Risk reduction
The diet of people at risk for stroke should be rich in vegetable dishes in order to reduce cholesterol levels in the blood and the possibility of their deposition on the walls of blood vessels. Berries and fruits reduce the likelihood of a recurrent attack by 25% due to the potassium they contain, which is also good for heart function.
It is better to replace meat dishes with fish. Cooking method: stewing or boiling with a little salt.
Do not use white flour, as it is less easily digested by the body. Whole grain bread or steamed bran is an alternative to white bread. You can use corn or oatmeal.
Heavy physical activity after a stroke should be avoided. Hiking and light exercises in the air will be useful.
To treat metabolic diseases, they turn to specialized specialists. The recommendations received will allow you to support other organs and systems that affect the condition of blood vessels and their patency.
Hemodynamic stroke
This type of brain stroke in most cases occurs with loss of consciousness. The mechanism of the pathological process is triggered by a sharp decrease in pressure, which is often observed in people suffering from heart failure. At this point, the supply of nutrition and oxygen to the brain suddenly stops.
Some clinicians refer to this form of pathology as a migraine stroke. It is usually accompanied by focal symptoms, which can disappear and appear again.
With a migraine stroke, blood circulation is disrupted in a certain area of the brain, and the consequences can manifest themselves in the form of the formation of ischemic cysts at the site of the lesion, which are determined even in a period of complete well-being.
What kind of brain stroke occurs in athletes?
What is a stroke
A disruption of blood supply and nutrition to any part of the brain, followed by rupture of a vessel, effusion of blood into neighboring tissues, or death of nerve cells due to hypoxia is called a stroke. The intensity of blood flow may decrease or stop completely. The acute condition develops over a long period of time - from several hours to several days.
In the first case, irreversible consequences can occur quickly, and the patient will not have time to receive medical help. In the second, the symptoms are less acute, but eliminating the consequences will be more difficult.
On average, a person has 5 hours from the moment characteristic symptoms appear to seek help and take a number of measures to improve their well-being.
When a part of the brain dies, a disruption occurs in the functions in the human body for which this area is responsible - speech, movement. The pathology can occur in mild, moderate and severe forms.
Hemorrhagic type of stroke
This type of stroke is much less common than ischemic strokes, and it affects people of a younger age - from 40 years old. The main reasons for the development of such pathology are atherosclerosis, high blood pressure, as well as some diseases associated with changes in the structure of the vascular walls.
A high likelihood of developing this type of stroke is observed in people who abuse alcohol and drugs. Cases of stroke are often diagnosed when using high doses of anticoagulants.
This type of pathology is characterized by a sudden onset with the rapid development of serious disorders. It can be caused by stressful situations and a sharp increase in blood pressure. Brain damage is accompanied by meningeal signs.
With the hemorrhagic form of stroke, in most cases, coma occurs, and among patients with a similar diagnosis, the highest mortality rate is observed.
When hemorrhage is localized in the arachnoid membrane, death occurs in 38% of cases, even when receiving qualified assistance, and patients who survive become disabled.
We looked at what types of brain strokes exist.
Main symptoms
Behavior after a stroke may vary between patients. Some are characterized only by changes in physical and practical skills, others note a weakening of mental functions. And in some cases, a combination of both manifestations is possible, when the physical capabilities of the patient are impaired, and there is a gradual fading of the main psycho-emotional factors, on which the quality of everyday life largely depends - both for the victim after a stroke and his immediate environment.
Symptoms that characterize physical disorders when dementia occurs include:
- change in gait - the patient feels unsure of his movements, as a result of which the gait loses confidence, may seem unsteady, and the direction of movement changes sharply;
- deterioration in the process of controlling one half of the body (which is most common);
- urinary incontinence (about 30% of cases after a stroke with the development of dementia).
With psycho-emotional problems in the process of worsening dementia, the manifestation of such lesions as mood lability, a tendency to depressive states, and possibly a pronounced deterioration in speech, writing, and reading are likely to occur. There may be changes in the perception of the surrounding world and reality. Impairments in thinking and assessment of ongoing phenomena are all manifestations of the consequences of the development of dementia after a stroke.
There is a certain relationship between the manifestations of dementia that occurs after a stroke and the intellectual level of development of the patient before the disease. With a high level of intellectual development, manifestations are revealed to a slightly lesser extent; with a low level of intellectual development, manifestations of senile dementia are observed to a greater extent.
Clinical signs of all types of strokes
All symptoms of this pathology are divided into three main groups. In this case, they differ:
- Meningeal symptoms similar to those that develop with inflammation of the meninges. The patient cannot tilt his head due to strong tension in the muscles of the back of the head. When lying down, the leg may not extend at the knee (Kernig's sign).
- General cerebral symptoms, which include headache, vomiting and severe nausea, disturbances of consciousness (from mild fog to deep coma). In 15% of patients, a convulsive seizure occurs, which is similar to an epileptic attack.
- Focal symptoms manifesting themselves in the form of hyperkinesis and paresis of varying degrees. In this case, speech is impaired, temperature, pain and tactile sensitivity changes. Hallucinations, loss of coordination, and amnesia may occur.
Symptoms of a stroke
The symptoms and causes of stroke are varied. However, in order to recognize a stroke, you need to ask the person to perform three simple steps:
- smile. A stroke can cause paralysis of the facial muscles. The smile and face should normally be symmetrical;
- raise both hands, they should not involuntarily drop;
- say a simple phrase or repeat your own name. Confused and slurred speech indicates a stroke.
During an attack, the patient may experience sudden headaches, blurred vision, speech impairment and muscle paralysis, mainly on one side. Symptoms of a stroke can appear quickly, so if even one is detected, it is necessary to urgently take the patient to the hospital or call an ambulance.
Neurologists at the Yusupov Hospital provide emergency care to patients of any severity. A stroke, the causes of which a doctor can determine, depending on the type, requires measures to eliminate bleeding or dissolve blood clots.
Difference between ischemic and hemorrhagic type
With ischemic strokes, focal symptoms come first. At the same time, symptoms of cerebral abnormalities are not expressed significantly, and meningeal abnormalities are almost always absent.
With the hemorrhagic type of hemorrhage, it is the general cerebral disorders that become more significant. The meningeal complex is observed primarily during subarachnoid hemorrhages.
Both types of stroke are accompanied by specific symptoms characteristic of each of them, from which a specialist can immediately determine what type of stroke is occurring in a particular case.
How to prevent a cerebral stroke? To do this, you need to be able to recognize symptoms in a timely manner.
Differential diagnosis of strokes
Differential diagnosis of the two types of stroke is extremely important for prescribing treatment. They differ not only in clinical manifestations. Instrumental studies also show different data. To diagnose any stroke use:
- computed tomography, it is necessary to determine the type of stroke and the amount of hemorrhage;
- MRI gives a more accurate picture, but due to the duration of the procedure it is used less frequently;
- diffusion-weighted tomography, which shows the area of the brain with impaired blood circulation, diagnosis takes only a few minutes;
- cerebral angiography is an invasive method that provides a complete picture of the condition of the vessels, the presence and localization of blood clots and aneurysms.
In addition, a heart examination is required to identify pathologies that contribute to the formation of embolic thrombi. The study includes:
- Ultrasound of the heart;
- daily ECG monitoring;
- ECG;
- ECHO KG.
Features of clinical manifestations of ischemic and hemorrhagic stroke
Difference in symptoms:
| Signs | Ischemic form | Hemorrhagic form |
| Speed of disease development | Gradual onset with morning or night onset | Abrupt onset during physical activity or mental stress |
| Appearance | Ordinary | severe redness of the face; |
| involuntary twitching of the eyelids or their closing; | ||
| increased sweating | ||
| Headache accompanied by nausea and vomiting | Sometimes | Common, especially with subarachnoid hemorrhage (SAH) |
| Damage to one side of the body, numbness, focal changes in muscle tone | Explicitly expressed | Expressed in cerebral hemorrhage, absent in SAH |
| State of consciousness | Gradual increase in impairment of consciousness | Coma may quickly set in |
| Loss of consciousness | Possible short-term | Often long lasting |
| High blood pressure | Yes | Sometimes |
| Partial paralysis or weakening of muscles | Most often from the very beginning of stroke development | Rarely |
| Seizures and increased motor activity | Rarely | Yes |
| Speech problems | Yes | Sometimes |
| Retina | Clean | There is hemorrhage |
One type of assessment of a patient's neurological status is a test for meningeal syndrome. For hemorrhagic stroke (especially SAH), it is sometimes the only diagnostic clinical sign:
- severe tension in the neck muscles (the patient cannot press his chin to his chest);
- in a lying position, the patient cannot straighten the leg at the knee, which is bent at the hip at a right angle;
- when he tries to raise his head while lying down, his legs involuntarily bend at the hips and knees;
- passive flexion of one leg at the hip joint causes involuntary flexion of the other leg.
Difference in analyzes
Also, for the differential diagnosis of ischemic and hemorrhagic stroke, cerebrospinal fluid (CSF) puncture is used. During ischemia, the cerebrospinal fluid is colorless; during hemorrhage, it contains an admixture of blood.
A coagulogram is required - a blood test for clotting. In acute ischemic stroke, the blood's ability to dissolve blood clots increases. During hemorrhagic the following changes are characteristic:
- blood clotting increases;
- resistance to heparin increases;
- fibrinogen formation increases;
- the ability of platelets to glue and attach to the walls of blood vessels increases;
- red blood cell membranes lose elasticity.
In this way, the body responds to “unauthorized” bleeding. In the general blood test, changes are also observed that make it possible to recognize ischemic and hemorrhagic stroke.
In the first case, changes concern the leukocyte formula, hemoglobin and the number of red blood cells are increased. In the second, there is only slight leukocytosis and a decrease in the number of lymphocytes.
Differential instrumental diagnostics
Diagnosis of stroke using instrumental methods allows you to accurately make a diagnosis - ischemic or hemorrhagic stroke.
The research methods are the same, but record different results:
| Research method | Results in ischemic stroke | Results in hemorrhagic stroke |
| Electrocardiography | Myocardial ischemia, presence of arrhythmia | Enlargement of the heart |
| Fundus examination | Atherosclerotic changes in blood vessels | Hemorrhages |
| ECHO-encephalography | Median echo without offset | the median echo is shifted towards the healthy hemisphere; |
| signs of increased intracranial pressure and cerebral edema | ||
| Computed tomography (in the first hours of stroke development) | Effective in approximately 60% of cases | 100% diagnostics |
| MRI | gives an image of the necrosis zone; | |
| allows you to establish a violation of liquor dynamics | ||
| gives a picture of the site of hemorrhage and hematoma; | ||
| detects cerebral edema; | ||
| shows blood entering the cerebrospinal fluid |
Ultrasound scanning of cerebral vessels is also informative for diagnosing ischemic stroke. Doppler ultrasound shows the presence of plaque and the hemodynamic significance of vasoconstriction. You can also determine the speed and direction of blood flow.
In general, it helps to diagnose a stroke of any form:
- electroencephalography;
- angiography with contrast under X-ray control (mainly performed before neurosurgery).
Clinical picture of widespread brain damage
When disturbances affect a large part of the brain cells, a particularly severe degree of pathology develops. The patient, regardless of the type of cerebral stroke, may experience:
- paralysis;
- loss of consciousness;
- convulsions;
- hypertonicity of the muscles of the legs and arms;
- signs of cerebral edema;
- speech deviations;
- mental disorders, strange behavior;
- trophic failures;
- violation of pupil accommodation;
- autonomic disorders;
- strabismus.
Cerebellar lesion
In cases where local damage to the cerebellum is observed, such a condition is considered no less dangerous than that which occurs with a major stroke. The pathological symptoms are similar, but there are some specific manifestations of this pathology:
- disturbance of gait and coordination;
- nausea;
- changes in speech and swallowing;
- deterioration in health when moving the body;
- loss of sensation;
- sunken eyelids;
- loss of consciousness.
Primary prevention of stroke
Primary prevention of stroke is a system of measures aimed at preventing the first cardiovascular catastrophe. Doctors at the Yusupov Hospital recommend that patients use all methods of influencing areas of their lives that reduce the negative impact of traditional risk factors. The axiom is the formula: weight loss + quitting smoking nicotine + physical activity is more effective than medications. Lifestyle changes combined with regular, evidence-based preventive drug therapy can prevent stroke and add an additional 8-10 years to life.
Brainstem lesion
This type of stroke, which affects the stem part of the brain, is very difficult and in most cases ends in death. In this area of the central nervous system there are special centers that are responsible for the most important functions that support the vital functions of the body. As a rule, with this type of pathology the following symptoms are noted:
- difficulty swallowing, asphyxia;
- violation of speech functions;
- inability to move independently due to severe lack of coordination of movements.
Not everyone knows what types of brain strokes there are and how they differ from each other.
First aid
Before doctors arrive, a person with signs of a stroke can be helped in the following ways:
- lay on a flat surface so that the head is raised at an angle of 30°;
- provide a flow of fresh air;
- unfasten the belt and the top button on the clothes;
- if a person has been vomiting, you need to turn him on his side and clear his mouth of any remaining vomit;
- in the absence of heartbeat and pulse, indirect cardiac massage is performed;
- If possible, measure blood pressure and record the readings.
You can't give a person something to drink. If swallowing is impaired, asphyxia may occur. Blood pressure-lowering medications should not be given until doctors arrive.
Features of strokes in childhood
Currently, this pathology is increasingly observed in children. The following subtypes of stroke are distinguished:
- fertile (during intrauterine life);
- perinatal (in newborns);
- in children from one to 18 years of age.
Hemorrhage, which leads to cerebral ischemia, is fatal in 90% of cases. Children with rheumatism or congenital heart defects are at high risk of developing an ischemic type of stroke.
The ischemic type of stroke in childhood is very rare. Of primary importance is the hemorrhagic form of this pathology, the cause of which is the increased activity and mobility of the child against the background of insufficiently formed vascular walls.
The main signs of the development of this pathology in childhood are the same as in adults. Difficulties in diagnosis arise in newborns, when some brain disorders appear against the background of immature neurological reactions.
The consequences depend on the type of brain stroke.
Features of therapeutic effects
Since after a stroke the brain suffers to a greater extent, the therapeutic effect should be aimed primarily at restoring the normal functioning of its tissues. In this case, various techniques can be used to provide the most comprehensive approach to obtain the most pronounced positive result.
The most effective measures in the treatment of senile dementia after a stroke include the following measures:
- medicinal effects, which is expressed in taking nootropic drugs. They stimulate brain activity and provide improved nutrition to its tissues. With their help, the protective potential of the brain increases. Such drugs include Piracetam and Nootropin;
- tranquilizers and antidepressants that stabilize the patient’s psychological state. However, their use should be carried out under the strict supervision of the attending physician and taking into account the pronounced positive dynamics of the treatment process;
- vitamin complexes, which also help to quickly eliminate the consequences of brain disorders and stimulate the rapid restoration of lost brain functions;
- drugs to improve blood supply to brain tissue - Tavegil, Cavinton;
- complex use of medications to stabilize thought processes and improve memory - Memantine;
- conducting physical therapy and massage sessions that eliminate muscle tightness, stimulate blood circulation processes, which allows you to gradually return the body to normal physical condition;
- psychotherapy providing psychological assistance to a patient who has suffered a stroke.
To prevent recurrence of stroke and aggravate the current manifestations of senile dementia (dementia), one should first of all eliminate bad habits, stabilize the patient’s daily life, organize a healthy diet, and give regular physical activity to his body, which should be normalized in accordance with his general condition.
Danger of strokes
The consequences of a stroke are very serious and they consist in the fact that after prolonged ischemia, irreversible damage occurs in the brain cells, which include cerebral edema, pulmonary artery damage, and heart failure.
The consequences of a stroke on the left side of the brain (it directly depends on the type) can be different:
- Impaired motor activity due to paralysis.
- The degree of sensitivity of the hands, feet, and face decreases.
- Deviations of a cognitive nature.
- Disorientation in space.
- Psychical deviations.
- Difficulty in eating due to swallowing disorders.
- The appearance of epileptic seizures.
- Decreased vision, development of hearing loss, impaired speech functions.
- Involuntary defecation, enuresis.
We looked at the types of brain strokes and how they differ.
Life expectancy after stroke
The neurology clinic accepts patients over 18 years of age. In the modern world, experts note a decrease in the age of development of the disease, this is explained by the fact that the causes of stroke are varied, including due to bad habits.
For people who have suffered a stroke, the relevant question is how many years they live after a stroke. Doctors cannot give a definite answer to this question, since after a stroke, death can occur in the first minutes. However, with proper rehabilitation, life expectancy increases and people return to their normal lifestyle. The prognosis of a stroke is determined by many factors:
- patient's age;
- general health before the stroke;
- the presence of stress factors;
- complete elimination of causes;
- quality of life before illness and after stroke;
- correctness and adequacy of rehabilitation measures;
- the presence of other chronic diseases.
The risk of an unfavorable course of the disease increases when several factors combine. The exact prognosis can be determined by the neurologist treating the patient. At the Neurology Clinic of the Yusupov Hospital, doctors pay close attention to each patient and also provide a wide range of medical services: diagnostics, preventive measures, inpatient and outpatient treatment, and rehabilitation measures. You can contact a neurologist to determine the causes of the stroke, perform a diagnosis and begin treatment. Make an appointment by phone.