The death of a person is unique, however, if it is a gradual decline associated with age or a long-term illness, a number of general signs can be identified that indicate the approach of death.
general information
During a comatose state, the patient completely loses contact with others. A profound impairment of consciousness is determined by the complete absence of mental activity. Even intense stimulation cannot bring the patient out of this state. Coma is different in that the patient is always in a supine position with his eyes closed, which he does not open when exposed to sound stimuli or pain.
Clinical symptoms depend on the cause of occurrence and the severity of suppression of the nervous system - absence or presence of spontaneous movements, extinct or preserved reflexes, spontaneous breathing, dependence on life-supporting equipment.
The origin is due to extensive damage to special brain areas responsible for wakefulness.
Severity of coma in older people
- Prekoma. In this state, elderly people experience slow reaction, weakness, confusion, or, conversely, develop psychomotor agitation. Pathologies occur in the functioning of internal organs according to the characteristics of the disease that caused the onset of coma in an elderly person. Reflex reactions remain.
- Coma I degree. The patient begins to develop deafness, and the reaction to stimuli is inhibited. An elderly person in a coma of this degree is able to swallow liquid food and perform simple movements, but it is already quite difficult to establish contact with the patient. Reflex reactions are inhibited or exaggerated depending on the type of coma.
- Coma II degree. In this state, the patient experiences deep sleep, sometimes uncontrolled movements of the limbs appear, and contact is impossible. An elderly person in a coma experiences pathological noisy breathing, arrhythmia, and involuntary emptying of the bladder and intestines. There are no reflex or pupillary reactions, skin sensitivity does not appear.
- Coma III degree. Patients lack consciousness, pain sensitivity, reflex reactions, and the pupils are dilated. An elderly person in a coma experiences a decrease in body temperature, depressed breathing and a drop in blood pressure.
- Coma IV degree. Patients are diagnosed with complete impairment of consciousness, absence of reflex reactions and muscle tone, decreased body temperature and blood pressure, sudden stops in respiratory movements, which requires connecting the patient to a ventilator.
Read material on the topic: Life after 80 is just beginning
Causes
The occurrence of coma is always caused by damage to the nerve pathways caused by severe pathologies of the central nervous system. A coma cannot be an independent disease.
The reticular formation is a mesh-like structure that runs throughout the brain. All signals from the surrounding reality pass through it, filtered and systematized. When the cells of this unique system are damaged, the nervous system's connection with the outside world is lost.
The causes of damage to the reticular pharmacy system are divided into:
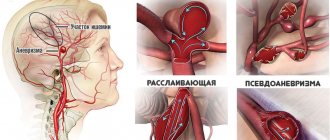
- Physical: cerebral hemorrhages, injuries, bruises, bullet wounds, strokes.
- Chemical, in turn, are divided into external and internal. Poisonous compounds coming from outside can be narcotic substances, sleeping pills, neurotropic poisons, toxic toxins in infectious diseases. Internal chemical compounds are formed as a result of metabolism and diseases of internal organs. These include ammonia (severe liver pathologies), abnormal levels of glucose and acetone (diabetes mellitus), and insufficient oxygen in the blood (hypoxia).
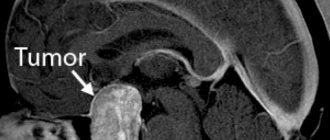
- The most severe is the combination of physical and chemical effects on the reticular formation. The result is a worsening of intracranial pressure indicators. This case occurs with tumors of the central nervous system and traumatic brain injuries.
When is coma possible in older people?
In a comatose state, consciousness is switched off, and reactions to external stimuli are completely absent.
Coma in older people develops as a result of acute circulatory disorders in the brain, which leads to damage to the central nervous system and changes in the functioning of vital body processes. The duration of the coma lasts about 2–4 weeks. The outcome directly depends on the reasons that caused it, the severity and location of the damage. When recovering from a comatose state, older people have a high probability of developing physical, psychological, and intellectual pathologies. After regaining consciousness, tests are performed to help assess the patient's health. The source of coma can be:
- cerebral circulatory disorders;
- diabetes;
- brain injuries and tumors;
- acute renal or liver failure;
- violation of water and electrolyte metabolism in the body;
- stroke;
- intoxication of the body.
Read material on the topic: Diseases of old age: types, causes, symptoms
Classification
Comatose states are classified according to groups of criteria:
- the reason that caused it;
- degree of depression of consciousness.
Depending on the reasons, they are divided into the following types:
- traumatic - as a consequence of cranial and brain injuries;
- epileptic - as a worsening of epilepsy;
- apoplexy - the result of a stroke;
- meningeal - a consequence of meningitis;
- tumor - neoplasms in the skull;
- endocrine - during diabetes mellitus, a decrease in the properties of the thyroid gland;
- toxic - a consequence of renal and liver failure.
Causal classification does not reflect the patient’s actual well-being, and therefore is not used in neurology. Professionals in this field of medicine classify the case according to the severity of the person’s condition - the Glazko scale. The method is based on a general assessment of three indicators: the patient’s speech, the presence of body movements, and the opening of the eyelids. Depending on the severity of their violations, a certain number of points are assigned. The sum of the scores determines the patient’s degree of consciousness:
- 15 points - clear consciousness;
- 14-13 points - moderate stunning;
- 12-10 - deep stun;
- 9-8 - stupor;
- 7 or less - comatose state.
Based on these data, the severity of a person’s situation can be easily calculated, emergency treatment tactics can be quickly developed and the outcome of the disease can be predicted.
In intensive care circles, doctors divide coma into 4 degrees:
- I - stupor of consciousness;
- II - stupor;
- III - atonic;
- IV - beyond.
Clinical symptoms
The main clinical sign is the patient’s absolute lack of consciousness, deprivation of mental activity and contact with the outside world. All other manifestations of the disease are associated with the causes that caused brain damage:
- Body temperature indicators. Hypothermia occurs in case of poisoning with sleeping pills, alcohol (can decrease to 32-34 C⁰). An increase in temperature to 42-43 C⁰ and dry skin accompany a coma caused by general overheating.
- Respiratory frequency. Slow, shallow breathing is a sign of an overdose of morphine-containing drugs, sleeping pills, and a decrease in the level of thyroid hormones. Deep breathing is a distinctive feature against the background of infectious intoxication due to pneumonia. This symptom occurs with kidney failure, brain tumors, uncontrolled sugar levels in diabetes in the form of acidosis.
- Pulse and blood pressure. A decrease in heart rate (bradycardia) signals coma due to heart pathologies. Frequent heartbeat - tachycardia, in combination with significant blood pressure numbers, indicate an increase in intracranial pressure. Hypertension, as a symptom, appears in patients in a coma after a stroke. Low blood pressure occurs in cases of poisoning with sleeping pills, heavy intra-abdominal bleeding, myocardial infarction, and diabetic coma.
- Skin color is also a significant diagnostic symptom. When intoxicated with carbon monoxide, the skin gradually acquires a dark red color. Suffocation is accompanied by a sharp decrease in the level of oxygen in the body’s blood, as a result of which the nail phalanges of the fingers and the nasolabial triangle turn blue. Bleeding from the ears and nose, bruises, bruises around the eyes (“a symptom of glasses”) correspond to a coma that manifested itself as a result of a traumatic brain injury. If the coma is caused by global blood loss, the skin becomes distinctly pale.
- Maintaining contact with others. A favorable encouraging sign is the ability of patients to utter some sounds. This is observed with mild coma or stupor. The more severe the patient's condition becomes, the faster the ability to make sounds is lost. The mild form is also characterized by reflex movements of the limbs in response to pain, possibly causing grimaces.
Types of coma in older people
Coma due to stroke
The most common cause of coma in older people is stroke.
This disease develops due to impaired blood circulation in the brain. There are two types of stroke: ischemic and hemorrhagic. Ischemic stroke. It occurs in the process of blocking the lumen of a blood vessel and limiting the supply of oxygen to brain cells. This form of the disease is less dangerous, since with timely diagnosis and treatment, the development of pathology and the onset of coma in an elderly person can be prevented.
A comatose state after an ischemic stroke occurs only in cases where extensive damage to brain tissue occurs. But with proper and timely treatment, the outcome in most cases is positive.
Hemorrhagic stroke occurs as a result of the destruction of a blood vessel caused by a sharp increase in blood pressure.
With a hemorrhagic stroke, bleeding occurs in the brain, an intracranial hematoma is formed, which puts pressure on the brain structures. In this case, intracranial pressure increases, cerebral edema forms and neurons are destroyed, which entails the development of coma in an elderly person.
- Recommended articles to read:
- Social services for older people
- Diseases of old age
- Valuable tips on how to choose a boarding house
In old age, the body's protective functions are weakened, as a result of which various pathologies are likely.
Based on this, we can conclude that stroke and coma are critical conditions for elderly patients. Also at risk are people with diseases such as atherosclerosis and arterial hypertension. The development of stroke in elderly people over 65 years of age differs significantly from this condition in younger people, and is accompanied by the following symptoms:
- pronounced clinical manifestations of stroke occur in a short time;
- the disease develops quickly and aggressively, with a high rate of damage to brain cells;
- severe consequences of pathology, long rehabilitation;
- Outcome prognosis for older people is much worse than for younger people.
According to statistics, in 45% of cases after a stroke, elderly patients fall into a coma within the first 72 hours.
Diabetic coma
This comatose state can occur in people who have diabetes, regardless of low or high blood glucose levels. In a state of diabetic coma, elderly people are diagnosed with a specific odor of acetone from the mouth. With timely and correct identification of this pathology, the patient can be quickly removed from this condition. If there is any suspicion that coma is likely, a blood sugar test should be performed. If the level is elevated, then inject insulin; if it is low, the person needs to take carbohydrates. You should also contact your doctor as soon as possible to recover and recover from a coma.
Traumatic coma
Traumatic coma in older people occurs when a traumatic brain injury occurs that causes brain damage. A concomitant symptom is vomiting in a precomatose state. When providing first aid, measures should be taken to improve blood circulation in the brain and restore its functions.
Cerebral coma
Cerebral coma in older people develops due to the presence of tumors in the brain. The precomatose state is accompanied by:
- severe headache and vomiting;
- the person has difficulty swallowing food and liquids.
If a patient experiences similar symptoms, immediate first aid is necessary, otherwise coma may develop. Also, these reactions may indicate the presence of a brain abscess, but this disease is accompanied by inflammatory processes such as tonsillitis, sinusitis or otitis media. Only a specialist can diagnose pathology and provide qualified assistance.
Epileptic coma
Epileptic coma in older people can develop as a result of a severe seizure. Symptoms of this disease are manifested in the following: enlarged pupils, pale skin, depressed reflexes of the body, there are bite marks on the tongue, in most cases there is uncontrolled emptying of the bladder and intestines. There is also a decrease in pressure and temperature, and an increased pulse is felt. As the patient's condition worsens, breathing changes and the pulse becomes thready. If you do not immediately provide first aid to a person, then all reflexes will fade, the pressure will decrease, and death will occur.
Hepatic coma
The development of coma in older people can be caused by improper liver function.
Any pathological abnormalities in the functioning of this organ can lead to a coma. Since the liver is a natural filter, disruption of its function leads to intoxication of the body with metabolic products, which entails the development of coma in an elderly person. Also in this case, disturbances in heart rhythm and cerebral edema are diagnosed. If you do not turn to specialists to provide the patient with qualified assistance as soon as possible, then this condition can lead to death. Read material on the topic: Cardiac cough in the elderly: symptoms and treatment
Diagnostics
The diagnosis immediately establishes the causes of the comatose case. The conclusion differentiates the condition from other similar disorders of consciousness. The following diagnostic methods are used:
- Anamnesis collection. They find out from the patient's relatives or witnesses whether the patient took medications, and whether empty jars or blisters of medications were found nearby. You should ask about the presence of chronic diseases of blood vessels, endocrine glands, and heart. Clarify that the patient may have voiced complaints. An important factor is the age of the patient and the speed of development of symptoms. Young people more often fall into this state after poisoning with sleeping pills or narcotic drugs. In elderly patients, the formation of a coma occurs against the background of heart attacks, strokes, and other cardiovascular diseases.
- Inspection. During the examination, the possible root cause of the coma is determined. Respiratory rate, pulse rate, blood pressure, body temperature, injection marks, bad breath, bruises are indicators on the assessment of which the establishment of a correct diagnosis depends.
- The patient's position can also characterize the severity of brain damage. During hemorrhages and meningitis, the patient’s head is thrown back, the neck muscles have a pronounced tone - signs of irritation of the meninges. Convulsive attacks, cramping spasms of individual muscles indicate the patient’s status epilepticus, the condition of eclampsia in pregnant women. Unexpressed paralysis of the limbs indicates a stroke, a complete absence of reflexes indicates deep lesions of the cortex and spinal cord.
- A differential feature distinguishing it from other disorders of consciousness was the study of the patient’s function to open his eyes to irritation in the form of sound or pain. If the response to sound and pain stimulation in the form of involuntary opening of the eyes persists, then this is not a coma. If the eyes remain closed, the case is considered comatose by doctors.
- The doctor carefully evaluates the ability of the pupils to respond to light. Its quality makes it possible to determine the damaged area of the brain, and also indicates the factor that provoked the coma. The clarity of the pupil's reaction to light indicates the future prognosis of the disease.
Pinpoint pupils that do not respond to bright light indicate alcohol or drug poisoning. If the pupils of the left and right eyes have different diameters, this is a sign of increasing intracranial pressure. Excessively wide pupils are a symptom of midbrain pathologies. If, when exposed to bright light, the reaction of the pupils is completely absent, their diameter remains wide, this is a very unfavorable symptom, which indicates imminent brain death.
The development of medicine makes it possible to use hardware methods for diagnostic purposes to examine patients with impaired consciousness immediately upon admission to a medical institution. Performing head computed tomography (CT), magnetic resonance imaging (MRI) makes it possible to detect changes in areas of the brain, lesions, tumor-like neoplasms, and signs of intracranial hypertension. The conclusions obtained as a result of the tomograph study serve as the basis for determining treatment tactics - surgical or conservative.
X-rays of the head and spine in several projections are performed if MRI or CT is not possible.
A biochemical blood test can confirm a metabolic failure. Tests for the level of glucose, urea, acetone, and ammonia in the blood are carried out very quickly. The ratio of the content of electrolytes and blood gases is determined. In addition, the blood is examined for insulin levels, adrenal and thyroid hormones, for the presence of narcotic substances, tranquilizers and other toxic drugs, and bacterial blood cultures are performed to identify a possible infectious agent.
During an electroencephalogram (EEG), electrical impulses from the brain are recorded, which make it possible to determine the type of coma and understand what caused it - hemorrhage, poisoning or a tumor.
Forecast
Bringing a person out of a coma is, of course, not an easy task and can only be done by highly qualified specialists who work in specialized neurological centers. The prognosis depends entirely on the severity of the vegetative state - with mild precoma due to a rise in glucose, recovery occurs in full. Whereas in a coma due to a massive hemorrhagic stroke or a car accident, the person is unlikely to recover. However, doctors in intensive care perform all the required actions.
In addition, relatives are told how to bring the patient out of a coma - talk, read aloud their favorite books, tell important news about the family. This often contributes to the return of consciousness to the person. After a coma, he does not always sensibly assess his well-being and the disorder that happened to him. Therefore, he is under the supervision of doctors.
Avoiding coma allows timely treatment of chronic diseases, as well as compliance with all doctor’s recommendations.
Treatment
Treatment is a complex, comprehensive process that must prevent death, maintain vital body functions, and at the same time combat the root cause of this condition.
The first resuscitation measures aimed at preserving a person’s life are carried out immediately upon the arrival of the ambulance team and during transportation of the patient, before all diagnostic procedures are carried out. First aid consists of fixing the patient's position, ensuring patency of the airway - straightening the tongue, clearing the nose and mouth of vomit, an oxygen mask, tracheotomy with the installation of a breathing tube. It is necessary to normalize blood circulation by administering medications that normalize cardiac activity and blood pressure. If necessary, indirect cardiac massage is performed.
In the intensive care unit, the patient is connected to an artificial respiration apparatus. Medicines are administered aimed at eliminating the pathological symptoms of the disease - anticonvulsants, antipyretics, hemostatics. Intravenous infusions of glucose and saline solutions are required. Measures are necessary to normalize body temperature. In case of hypothermia, the patient is covered and covered with hot water bottles. If there is a suspicion of poisoning with chemical or pharmacological drugs, gastric lavage is performed.
At the second stage, having detailed results of all types of examinations, the cause is eliminated. In case of hyperglycemic coma, measures are taken to normalize blood sugar and insulin levels. In case of renal failure, hemodialysis is performed. If an injury, hematoma or brain tumor is detected, urgent or planned surgical intervention is performed according to indications.
Malfunction of body systems
Before a person begins his final journey “from old age,” disruptions are observed in all body systems:
- the kidneys refuse to work smoothly, so the urine becomes an unhealthy brown or red color;
- constipation or intestinal obstruction appears;
- it is difficult for a person to breathe, and his breathing becomes intermittent;
- the heart begins to work poorly;
- dark spots appear on the feet, and then all over the body;
- the skin becomes pale;
- hands and feet feel icy to the touch.
Prognosis and possible prevention
Predicting the situation while a patient is in a coma is based on the degree of brain damage and the causes of the disease. The more severe the patient’s condition, the more likely an unfavorable outcome is possible. The patient's chances of recovery are assessed according to the following measures:
- precoma, coma I - the prognosis is favorable, complete recovery is possible without residual effects;
- coma II and III - an unreliable position that can lead to both recovery and death of the patient,
- coma IV - in most cases leads to the death of the patient, the prognosis is extremely unfavorable.
Early prevention is focused on timely diagnosis of major disorders of the cardiovascular system, various tumor pathologies and other conditions that can lead to coma.