Vascular formations, especially in such an important location as cerebral structures, are relatively common. According to statistics, this kind of disorder is present in almost 3% of the world's population.
There are even more cases when the pathological condition is just developing, taking shape, but the prerequisites already exist. As a rule, diagnosis is greatly delayed, since the disease hardly makes itself felt until the critical moment.
It turns out that the patient understands what is happening so late that the treatment itself becomes dangerous.
A cerebral aneurysm is a wall protrusion of large arteries of cerebral structures, which is accompanied by a decrease in the elasticity of the internal walls of the vessel, a change in the density and strength of tissue at the local level.
The condition is dangerous and has its own code I67.1 according to ICD-10. If nothing is done, death from aneurysm rupture and massive hemorrhage cannot be avoided. The only question is how soon this will happen.
Unfortunately, the pathological process either does not produce any symptoms, or the signs are so scant that it is impossible to discern such a dangerous condition right away.
The prospects for recovery directly depend on the stage of the disorder and the moment of initiation of therapy. There is absolutely no time to hesitate. It's a matter of life and death.
general information
When studying only cases associated with clinically manifested pathologies, the prevalence reaches 0.01%. However, when conducting non-invasive techniques for examining cerebral vessels, the detection rate of cerebral artery aneurysms reaches 3% among people over 50 years of age. If the patient has risk factors, then the figure can reach 20-30%. In a small number of cases, the disease is congenital and can be detected in childhood.
Normally, the wall of an arterial vessel consists of 3 layers: internal, muscular and external. If any of them is damaged as a result of increased blood pressure inside the artery, a gradual stretching of the layers occurs, which leads to the formation of a protrusion of the wall. Most often, pathological changes are observed in the area of branching arteries, which is associated with the presence of turbulent blood flow in these areas. In this regard, protrusions form in the vertebrobasilar region and the origins of the anterior and middle cerebral vessels.
An aneurysm is usually divided into three parts: dome, body and neck. The cervix is the site of protrusion formation and consists of 3 layers, similar to a vessel. The dome has only an inner layer, making it thin and susceptible to tearing.
Probable forecast
Depending on the location of the affected vessel, the probable prognosis also differs. In addition, the specialist has to take into account the size of the aneurysm and the presence of concomitant pathologies that contribute to degenerative changes in the vascular walls.
- In the absence of aggravating factors, an intracranial aneurysm can exist without clinical changes throughout the patient's life.
- Aneurysm rupture leads to disability in 25-35% of cases, and death in 30-50%;
- The probability of recurrent hemorrhage is high at 20-25%, and in seventy cases the patient dies.
Formation of pathology
The causes of cerebral artery aneurysms are well known. Doctors divide all factors into 2 groups: modifiable and non-modifiable. The latter include:
- genetic predisposition - there are hereditary variants of the disease, the occurrence of which is associated with a defect in connective tissue proteins;
- concomitant hereditary diseases: autosomal dominant polycystic kidney disease, Marfan syndrome, neurofibromatosis type 1, Klinefelter syndrome, etc.;
- age and gender of a person, the maximum frequency of detection of such formations in the vessels of the brain is 50-65 years old, the incidence in women is higher than in men.
The group of modifiable factors includes:
- smoking and drinking alcohol;
- arterial hypertension, including hypertension;
- the use of drugs that increase the activity of the sympathetic nervous system;
- long-term uncontrolled use of oral contraceptives.
During the treatment process, modifiable factors in the development of pathology must be eliminated. This reduces the risk of relapse of the disease and the development of severe complications such as hemorrhagic stroke or coma.
Types of aneurysms
Depending on the time of occurrence, congenital and acquired cerebral aneurysms are distinguished. The congenital form of pathology is formed in utero and is associated with some kind of developmental defect or negative impact of environmental factors. As a rule, it is small in size and does not tend to grow further. Acquired variants include all cases that are identified in adulthood and are associated with pathologies of the body and modifiable risk factors.
Protrusions of the vascular wall can have different shapes: saccular or fusiform. Saccular formations can have several chambers, which is associated with multiple dissection of the vascular wall and are 50 times more common.
Aneurysms can be localized on any artery: the anterior or middle cerebral, internal carotid and vessels of the vertebrobasilar region. In 10-20% of patients, MRI or CT scans reveal multiple aneurysms located on one or more arteries.
The sizes of the formations are different:
- miliary - up to 3 mm;
- small - from 4 to 10 mm;
- medium - from 11 to 15 mm;
- large - from 16 to 25 mm;
- giant - more than 25 mm.
Without treatment, any type of cerebral aneurysm can grow larger. This is accompanied by thinning of their walls and an increased risk of rupture.
Classification of the disease
>The disease can be classified according to its location. Aneurysms occur:
- Internal carotid artery;
- Anterior cerebral artery;
- Vertebro-basilar system;
- Middle cerebral artery;
- Multiple aneurysms affecting several vessels at the same time.
The latter type of disorder occurs in approximately 13% of patients.
In addition, aneurysms are distinguished by shape:
- Fusiform;
- Saccular, occurs fifty times more often. It can be multi-chamber or single-chamber.
By size they are distinguished:
- Giant - more than 25 millimeters;
- Large – 16-25 millimeters;
- Medium – 11-15 millimeters;
- Small – up to 10 millimeters;
- Miliary - up to 3 millimeters.
Clinical manifestations
Symptoms of cerebral aneurysm differ depending on the type of course: tumor-like or apoplexy.
A tumor-like variant is noted in cases where the size of the protrusion of the vascular wall increases gradually and reaches gigantic sizes. All clinical manifestations are associated with the pressure of the aneurysm on the brain structures. Most often, compression of the cavernous sinus and the area of the optic chiasm occurs.
The patient experiences a gradual decrease in visual acuity and loss of individual fields. With long-term pathology, atrophy of the optic nerve is possible. Without treatment, blindness develops. Damage to structures in the cavernous sinus area manifests itself in three clinical variants:
- Pathology of the trigeminal nerve, characterized by pain along its branches. This nerve innervates the facial area, dividing into three separate branches - orbital, maxillary and mandibular. With large tumor sizes, the pain may be diffuse, but one-sided.
- Paresis of the III, IV and VI pairs of cranial nerves, which are oculomotor. The patient experiences strabismus, double vision, and gaze convergence disorders.
- A combination of the two previous syndromes.
Most often, an aneurysm manifests itself as apoplexy—rupture of its wall. Before this, there are no clinical signs. Sometimes, patients may complain of pain in the forehead and transient visual disturbances.
Signs of a ruptured aneurysm
When an aneurysm ruptures, a severe headache occurs. The pain syndrome can be local or diffuse, depending on the size of the ruptured protrusion. Simultaneously with the headache, nausea occurs with repeated vomiting, which does not bring relief. When examining the patient, meningeal symptoms are revealed: increased sensitivity to any irritants (light, sounds and touching the skin), stiff neck, etc. After a short period of time, the person loses consciousness, up to the development of coma. The patient may experience epileptic seizures and mental disorders, including psychosis. In subarachnoid hemorrhage, the accumulation of blood leads to compression of the cerebral arteries, causing ischemia of the nervous tissue. Stroke and aneurysm are closely related - when a vascular protrusion ruptures, ischemic or hemorrhagic brain damage, or a combination of both, is possible.
Aneurysm rupture
Hemorrhage into the brain tissue occurs in 40% of patients. Patients have severe general cerebral symptoms (headache, vomiting, meningeal symptoms), to which are added focal neurological deficits in the form of disturbances in sensitivity, motor functions, vision, etc. With hemorrhage in the ventricles, intracranial pressure increases, possible displacement of the brain and death.
The nature and severity of focal neurological symptoms depends on the location of formation. If the protrusion is located at the site of the branching of the carotid artery, visual impairment mainly occurs. When the anterior cerebral artery is damaged, the patient exhibits disturbances in movements in the legs and mental deviations from personality disorientation to psychosis. Rupture of an aneurysm of the middle cerebral artery is accompanied by paresis or paralysis of the arm and leg, which is accompanied by speech impairment.
Damage to the vertebrobasilar region is accompanied by impaired swallowing, speech and changes in gait. In addition, there is paresis of the facial muscles and disturbances in its sensitivity, due to damage to the nuclei of the facial and trigeminal nerves, respectively. If the aneurysm is located in the arteries outside the dura mater, then hemorrhages into the cranial cavity are not observed.
Possible consequences of cerebral aneurysm
Complications of cerebral aneurysm include almost any symptoms of this pathology, since they all lead to certain disorders. Thus, it is difficult not to call loss of vision or hearing a complication, which is provoked by compression of the nervous tissue by dilated blood vessels.
In addition, an aneurysm can cause other dangerous consequences for human health, for example, what happens when it ruptures. Other complications occur somewhat less frequently, but are no less dangerous.
Complications that may occur due to the presence of a cerebral aneurysm:
- Coma.
If an aneurysm forms in those parts of the brain that are responsible for a person’s vital functions, then he can fall into a coma. The duration of coma can vary, and often lifelong. Moreover, despite high-quality and timely medical care, many patients never recover from this life-threatening condition.
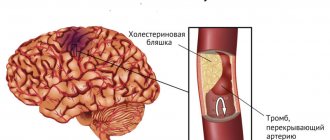
- Blood clot formation.
In the cavity of the resulting aneurysm, a slowdown and disruption of blood flow may occur, which leads to the appearance of a blood clot. Most often, such a complication develops against the background of the presence of a large aneurysm. The location of the thrombus may vary: sometimes it occurs in the cavity of the aneurysm itself, and sometimes it breaks off and blocks the flow of blood in smaller vessels. The more massive the blood clot, the more serious the threat to a person’s life, since in such a development of events he always suffers an ischemic stroke. However, with the provision of timely medical care, the patient’s life can be saved. Often, a blood clot can be dissolved with the help of medications.
- Formation of AVM.
An AVM is an arteriovenous malformation, which is essentially a defect in the vascular wall. This disruption leads to partial adhesion of the vein and artery. The pressure in the artery cavity begins to drop, and some of the blood passes into the vein. This leads to an increase in pressure in the vein, and those areas of the brain that were fed from the artery begin to experience hypoxia. An AVM is indicated by the same signs that occur against the background of an ischemic stroke. Sometimes the symptoms of an AVM are difficult to distinguish from the symptoms of a cerebral aneurysm. The larger the aneurysm, the more the vessel stretches, which means the higher the risk of AVM formation. If this complication develops, surgical intervention is required.
Due to the fact that an aneurysm can provoke serious complications that pose a threat to human life, doctors, when it is detected, insist on performing an operation. Moreover, the need for surgical intervention is also determined by the severity of the symptoms of the aneurysm itself.
Diagnostic measures
Aneurysms of the aorta and cerebral vessels are often asymptomatic and are diagnosed during examinations for another reason. At the beginning of the diagnosis, the doctor collects complaints, anamnesis of the disease and identifies modifiable and non-modifiable risk factors. Neurological symptoms are detected during examination of the patient.
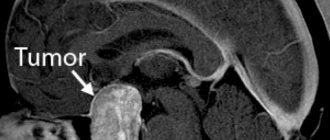
How to diagnose pathology in asymptomatic cases? To identify vascular protrusion, imaging methods are used: magnetic resonance imaging and computed tomography with angiography. These methods have a number of features:
- Magnetic resonance imaging with angiography is performed most often. Used as a screening tool for aneurysms in people with risk factors. Important advantages are its non-invasiveness and the absence of X-ray exposure to the patient.
- Computed tomography angiography has high sensitivity and specificity, which makes the risk of false results minimal. The procedure, despite its high accuracy, is not recommended for identifying miliary protrusions.
- Digital subtraction angiography (DSA) is the “gold standard” for detecting aneurysms smaller than 3 mm in diameter. Due to the invasiveness of the procedure, the use of contrast agents and a wide range of contraindications, it is not used for screening.
If a vascular aneurysm or its rupture is suspected, but there are no changes on CT and MRI, the patient can undergo a lumbar puncture. Using laboratory diagnostic methods, free blood is detected in the cerebrospinal fluid.
Differential diagnosis is carried out with various diseases. In case of apoplexy, it is necessary to exclude an epileptic attack, transient ischemic attack and ischemic stroke, as well as infectious meningitis. In the case of tumor-like symptoms, the differential diagnosis includes intracranial tumors, cystic formations, and intracerebral abscesses.
Medical imaging
This method of examining a patient can obtain a complete picture of a person’s internal organs without surgical intervention. The data obtained will complement the picture of the disease and make it possible to establish a diagnosis of the patient.
| Name | Principle of implementation | What determines |
| Computed tomography (CT) | X-ray radiation is used, thanks to which it is possible to obtain an image in a section of the required depth. | recognizes the smallest formations and their location; |
| symptoms of intracranial bleeding; | ||
| existing thrombus formations in the aneurysm cavity. | ||
| Magnetic resonance imaging (MRI) | It makes it possible to obtain layer-by-layer images with high resolution, images of the vessels of the head in detail, which are often not visible on CT. | expansion of vascular walls; |
| signs of cerebral hemorrhage; | ||
| compression of nerve fibers and cells. | ||
| Angiography | During this procedure, a contrast agent, visible by X-rays, is injected into the patient’s vascular bed; it is absolutely harmless to humans. | accurately determines the presence and location of an aneurysm; |
| reveals the degree of arterial blockage. | ||
| Doppler ultrasound (US) | A sensor is applied to individual areas of the head, which examines the condition of the blood vessels in the head. | area with impaired blood flow; |
| sudden dilatation of the arteries. |
Surgery
Effective treatment of cerebral aneurysm is possible only with the help of surgery. Patients with unruptured arterial protrusions are operated on in cases where there is a risk of their rupture:
- the diameter of the formation is more than 7 mm;
- the presence of diverticula in the protrusion or its irregular shape;
- lateral location;
- twofold predominance of the height of the dome in relation to the diameter of the artery;
- the formation departs from the vessel at an obtuse angle;
- within six months, the size of the aneurysm increased by more than 0.75 mm;
- the appearance of new neurological symptoms;
- tight contact between the wall of the aneurysm with the dura mater, bone structures and other vessels;
- multiple nature of aneurysms;
- a history of ruptures of vascular protrusions, etc.
In cases where the size of the aneurysm does not exceed 3 mm and there is no risk of rupture, the patient is monitored dynamically. At the same time, control studies are carried out after 6, 12 months and every 2 years in the future. If the patient refuses surgical intervention, then observation is carried out according to a similar scheme.
The issue of hospitalization followed by neurosurgical operation is decided individually. In addition to the size of the vascular formation, the patient’s age, gender, concomitant diseases and bad habits are taken into account.
Medicines are indicated in the period before surgery, during surgery, and also after surgery. The main task of medications is to prevent complications after treatment.
Types of operations
Elimination of a cerebral aneurysm is possible using two surgical interventions: clipping and endovascular embolization. Each method has its own indications.
Types of surgeries to repair cerebral aneurysms
Endovascular embolization is performed in the following cases:
- the patient's age is over 60 years;
- localization of the formation in the arteries of the vertebrobasilar region or in the cavernous region;
- concomitant severe somatic pathology.
Cerebral aneurysm clipping is indicated in the following cases:
- age up to 60 years;
- the aneurysm can be reached using conventional surgical access;
- large size of formations;
- the presence of thrombotic masses inside the protrusion of the vascular wall;
- the need to perform combined surgical interventions.
Embolization of an aneurysm involves the intravascular introduction of a special stent that blocks its lumen. This ensures the cessation of blood flow in the pathological area of the vessel and helps prevent its rupture or the formation of blood clots.
Clipping is carried out through a small microsurgical access in the skull, through which a metal clip is inserted into the area of the altered vessel, with the help of which the aneurysm is clamped. It is important to note that after clipping the patient is given a disability, and the chance of relapse remains. In this regard, the recommended method of therapy is endovascular surgery of cerebral artery aneurysms using embolization.
Clinical symptoms, course and tactics of management of patients with cerebral artery aneurysm
Neurological symptoms in a patient may indicate the location of an unruptured aneurysm, and sometimes indicate its progressive increase in size. The occurrence of paralysis of the muscles innervated by the oculomotor III cranial nerve, especially combined with pupil dilation (mydriasis), loss of its reaction to light and local pain under the eyeball and behind it, indicates expansion of the aneurysm. It may be located at the junction of the posterior communicating and internal carotid arteries. In order for paralysis of the muscles innervated by the third oculomotor nerve to develop, the length of the aneurysm from its exit point in the posterior communicating artery must be 7 mm or more and increase. In such a clinical situation, the patient is advised to immediately resolve the issue of surgical intervention.
Paralysis of the external rectus oculi muscle (abducts the eyeball outward) innervated by the abducens VI nerve may be a sign of a cavernous sinus aneurysm. Visual field defects in patients are often noted with an enlarging supracuneiform carotid artery aneurysm. Pain in the occipital and lower neck in a patient may indicate an aneurysm of the posterior/inferior cerebellar artery (PICA) or anterior/inferior cerebellar artery (IACA). Pain inside or behind the eyeball and at the bottom of the temple is usually noted with an expanding aneurysm of the middle cerebral artery.
An unruptured cerebral artery aneurysm may not produce clinical symptoms and may not bother the patient.
The question of whether an aneurysm can cause small, intermittent leaks of blood into the subarachnoid space (“spiking”) remains unclear. However, the significance of documenting the clinical associations of even the smallest aneurysm ruptures and bleeding is beyond doubt.
Sudden unexplained headache of any location should raise suspicion of subarachnoid hemorrhage in the patient. In this case, magnetic resonance imaging (MRI) or computed tomography (CT) of the brain is necessary to detect blood in the basal cisterns. Often minor subarachnoid hemorrhages are not detected on computed tomography () of the brain, therefore, to determine the presence of blood in the subarachnoid space, a lumbar puncture is indicated for such patients.
Conservative treatment
The patient is also treated without surgery. It includes adherence to the general regime and therapeutic diet No. 10. Nutrition should be rich in proteins, vitamins and microelements. Fried, smoked, and fatty foods are removed from the diet. Increase the amount of vegetables, fruits, nuts, dairy products, lean meats and fish consumed.
The following medications are used:
- Clopidogrel is an antiplatelet agent. Prescribed a week before surgery and used for 3 months after it. Allows you to prevent the development of thrombosis on the installed stent. Doctors recommend using it simultaneously with acetylsalicylic acid.
- Ticagrelor is an analogue of Clopidogrel. Used half an hour before surgery and for 3 months after it. Used for intolerance and contraindications to Clopidogrel.
- Heparin and nadroparin can be used for 3-5 days after surgery in the form of subcutaneous injections. Prevents the development of thrombosis.
- After endovascular interventions, patients are prescribed Nimodipine in tablet form. The drug is used to prevent spasm of arterial vessels in the brain after the development of subarachnoid hemorrhage.
- Vancomycin, Cefuroxime and Cefazolin can prevent antibacterial infections during clipping. Prescribed before surgery.
- In the postoperative period, non-steroidal anti-inflammatory drugs are prescribed - Ketoprofen, Nimesulide, Diclofenac, etc. They reduce the severity of pain and alleviate the patient’s condition.
Any medications can be used only as prescribed by the attending physician. All of them have certain contraindications for use, non-compliance with which can lead to side effects.
Complications of pathology
The consequences of a ruptured cerebral aneurysm are divided into two main groups: those associated with its rupture and those arising in connection with the treatment. If the integrity of the wall of the vascular protrusion is violated, the following complications may develop:
- Hemorrhagic stroke, characterized by a predominance of cerebral symptoms in the form of headache, nausea and vomiting, as well as meningeal symptoms. Treatment is surgery to remove free blood.
- Subarachnoid hemorrhage, leading to compression of brain tissue and its displacement into the area of the foramen magnum of the skull. This can lead to damage to the nerve centers in the brain stem, which can lead to the death of the patient.
- Hemorrhage into the ventricular cavity leads to a sharp increase in intracranial pressure and can cause cerebral edema. In this case, the patient is indicated for emergency surgery to drain the ventricular system and install a shunt. Blood coagulated in the ventricles forms multiple blood clots, making it difficult to carry out therapeutic measures.
- Ischemic stroke resulting from spasm or compression of cerebral vessels. In this case, the patient has pronounced focal neurological symptoms in the form of paresis, paralysis of the limbs, disorders of skin sensitivity, speech disorders, etc.
Consequences of aneurysm rupture
Negative complications of the treatment are manifested by the following conditions:
- Allergic reactions to radiopaque contrast agents and other medications used. The severity of allergies ranges from hives and difficulty breathing to angioedema and anaphylactic shock.
- Ischemic changes in the nervous tissue of the central nervous system associated with compression of the arterial bed.
- The development of thrombosis of the branches of cerebral vessels, which can cause a stroke and increase the severity of symptoms.
- Swelling of brain tissue with its displacement and compression of vital structures.
- Infectious complications that developed as a result of the addition of a bacterial infection when sterility was violated during surgery.
- Impairments of sensitivity, hearing and speech due to damage to parts of the brain.
To prevent complications associated with aneurysm rupture and treatment, diagnosis and therapy should be carried out with appropriate clinical guidelines.
Dimensions
- Miliary (less than 0.3 cm). They are characterized by scanty or absent symptoms. The operations performed are clipping; in case of damage to the vertebral vessels, endovascular intervention is performed. The outcome is favorable;
- Small (0.4-1.5 cm). The course is chronic. Nonspecific symptoms predominate (dizziness, headache, lethargy). The clinic may not be available. Operations – clipping, resection. The prognosis is relatively favorable;
- Large (1.6-2.5 cm). As a rule, the branches of the carotid artery are affected and are characterized by rapid growth and complications. The clinic corresponds to the zone of ischemia of the involved lobe. Treatment – resection, shunting. The prognosis is relatively poor;
- Giant (more than 2.5 cm). They are characterized by rapid growth and the addition of potentially lethal complications. The first manifestation of a giant cerebral aneurysm is often a stroke. The operation is open removal. The outcome is unfavorable.
For patients diagnosed with an aneurysm, it is very important to be under the supervision of a doctor who will talk in detail about this serious vascular damage and about the lifestyle with this disease. For our part, we also want to share important and necessary information on this topic:
- What is an aneurysm of the brain, carotid artery and neck vessels?
- What diagnostic methods are used?
- Modern surgical approaches to treatment and is it possible to do without surgery?
Rehabilitation activities
Rehabilitation after a rupture of an aneurysm of the arteries supplying the brain requires long-term training. The most commonly used are physical therapy, massage, as well as sessions with a psychologist and speech therapist. Restorative measures are indicated for all patients.
Therapeutic exercise is aimed at eliminating neurological deficits in the form of paresis and paralysis. If the mobility of the limbs is severely limited or completely absent, passive flexion of the arms and legs is performed with the help of a physical therapy specialist. Such exercises allow you to restore neuromuscular connections and ensure the gradual return of control over movements. If the patient has paresis, that is, a partial decrease in muscle strength, he can perform active movements. At first, the exercises are carried out without weights, however, in a later rehabilitation period, the patient works with exercise equipment. With regular exercise over several months, partial or complete restoration of movements is possible. An additional positive effect is observed with therapeutic massage, which relieves muscle spasms and improves blood circulation in them.
In case of speech disorders due to damage to brain structures, sessions with a speech therapist come first. The specialist works with the patient on sound pronunciation, starting with simple exercises and gradually complicating them. Additionally, speech therapy massage is performed, aimed at normalizing the tone of the muscles involved in the formation of sounds. All patients are advised to visit a psychologist or psychotherapist.
Relatives of a patient are often concerned about how long he can stay in a medical facility? During the rehabilitation process, the patient often requires constant medical supervision. In mild cases of the disease, with timely treatment, the patient can be discharged after 3-4 weeks. In this case, rehabilitation measures are carried out on an outpatient basis and at home. If the patient had severe complications in the form of hemiparesis and dysfunction of internal organs, hospitalization can last up to 6 months or more.
Prevention options
In this regard, experts highlight a number of recommendations that can prevent the development of pathology:
- Eliminate bad habits: smoking, drinking alcohol and drugs.
- It is necessary to treat arterial hypertension and constantly monitor blood pressure levels.
- Nutrition should be rational with reduced consumption of table salt. Anything fatty, salty, smoked, or with a lot of herbs and spices should be excluded from foods.
- Regular exercise, primarily cardio training, allows you to maintain a high level of health.
- If you have diabetes mellitus and other somatic diseases, it is necessary to monitor their course and follow the prescription of your doctor.
If you experience a headache or neurological symptoms, you should immediately seek medical help. Unpleasant sensations may hide the likelihood of developing intracerebral hemorrhage, stroke, etc.
Laboratory blood test
General and biochemical analyzes make it possible to determine closely related pathologies and the degree of risk if surgery is required. To determine an aneurysm, the patient should undergo basic blood tests in the laboratory:
- common with platelet count to determine the presence of infections in the body, the degree of anemia;
- to determine the prothrombin index, which shows the state of blood clotting, and the level of electrolytes.