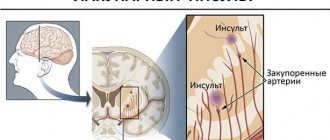
Disruption of the blood supply to certain areas of the brain leads to irreversible damage. A stroke can be ischemic - when tissues are deprived of oxygen for a long time, and hemorrhagic, occurring as a result of rupture of blood vessels with the release of blood into the surrounding space. Both conditions are deadly and require urgent medical attention. The first hours after an attack are decisive.
Briefly about recognizing a pre-stroke condition
The onset of a stroke is indicated by the following symptoms:
- headache;
- nausea;
- vomit;
- dizziness;
- anxiety;
- drowsiness;
- weakness;
- disturbance of consciousness.
Subsequently, convulsions, speech disorders, eye symptoms (double vision, constriction of the pupils, abduction of the eyeballs, narrowing of the visual fields, blindness), muscle weakness, paresis, paralysis, mental disorders, imbalance and movement disorders appear.
What medicine should you take before the ambulance arrives?
Stroke is a dangerous condition. Before the ambulance arrives, it is not recommended to give the patient any medications. Before this, you need to make a preliminary diagnosis and exclude other pathologies (encephalitis, trauma, infections, heart attack, tumors).
Therapeutic tactics for different strokes (hemorrhagic and ischemic) have their own characteristics. Self-medication can harm the patient.
Instead of drug therapy, you need to put the person down, calm him down, exclude him from food and water, clear his airways, provide him with air flow and monitor his vital signs.
Minimally invasive surgery: gentle treatment after ischemic stroke
One of the most common ways to neutralize the consequences of a stroke is treatment using a technology such as thrombolysis. During an angiogram, a drug is injected directly into the area where the blood clot has formed. The blockage disappears and blood circulation is restored.
Additionally, drugs are introduced that improve metabolic processes in the brain, so that after a stroke, treatment is faster and more effective. Delay is unacceptable; a diagnosis such as stroke can be treated in a hospital well with a timely response from doctors, when the brain has not yet received irreversible damage.
Differences in drug therapy for different types of stroke
Hemorrhagic attack
Hemorrhagic stroke is caused by damage to the cerebral arteries, bleeding into the brain or under the membranes and the formation of a hematoma, so treatment should be aimed at draining the blood, eliminating swelling, stopping bleeding and improving brain function.
Unlike cerebral infarction (ischemic stroke), the following medications can be prescribed for this pathology:
- hemostatics (Vikasol);
- antifibrinolytics;
- venotonics;
- saluretics in combination with osmodiuretics;
- calcium channel blockers;
- colloidal solutions;
- low molecular weight dextrans;
- angioprotectors;
- corticosteroids (Dexamethasone);
- calcium preparations.
Additionally, ascorbic acid and rutin are used to strengthen blood vessels.
Drug therapy is often combined with surgical treatment (drainage, decompression, hematoma removal).
In case of hemorrhage, most neuroprotectors, which are widely used to treat cerebral infarction, are contraindicated.
Ischemic stroke of the brain
Drugs against ischemic stroke include:
- Lipid-lowering drugs (statins, fibrates). They help with stroke due to atherosclerotic lesions of the cerebral arteries. This group includes Lovastatin (Cardiostatin), Atorvastatin (Atoris, Caduet, Liprimar, Torvacard), Simvastatin (Simvor, Vasilip, Zocor, Owencor, Zocor Forte), Rosuvastatin (Mertenil, Roxera, Crestor, Rozulip). These drugs have a lipid-lowering effect, reducing the level of atherogenic LDL (low-density lipoprotein) in the blood. Fibrates include fenofibrates Canon and Traikor.
- Antiplatelet agents.
- Anticoagulants.
- Thrombolytics (Streptokinase, Thromboflux). They dissolve fresh blood clots that clog arteries and are effective only in the early stages of the disease.
- Drugs that improve microcirculation.
- Neurotropic agents. This group includes vascular drugs, nootropics, antioxidants and antihypoxants.
Main causes of strokes
An immediate danger to cerebral circulation is posed by spasms, disruption of the integrity of vessel walls, and occlusion processes provoked by blood clots or cholesterol deposits. Most people have several main risk factors for developing pathology:
- physical inactivity: lack of physical activity causes systemic damage to the body;
- endocrine diseases: often lead to increased platelet production and excessive blood thickening;
- obesity: a platform for the development of many cardiovascular and metabolic disorders;
- chronic hypertension: due to increased load, blood vessels quickly wear out and become fragile;
- atherosclerosis: the lumen of the arteries gradually decreases due to plaque deposits in them;
- genetic predisposition: some people inherit a weak vascular system.
In young people, stroke is usually caused by congenital lesions of the cerebral vessels, consequences of traumatic injuries, and some systemic diseases, including severe hypertension.
In women during menopause, the risk of stroke increases due to age-related hormonal changes. Their bodies produce less estrogen, which protects blood vessels from damage. As a result, heart problems develop faster, weight increases, thyroid disorders occur more often, and cholesterol levels rise. One of the characteristic signs of menopause is an increase in the level of platelets in the blood. Combined with other changes and in the absence of a healthy lifestyle, the risk of stroke becomes more real.
Alcohol and tobacco smoking also systematically lead to vascular disorders: they destroy their structure, increase permeability, reduce tone and elasticity. These habits are dangerous for men and women of any age.
Classification of medications
Antidepressants and tranquilizers
One of the consequences of a stroke can be severe depression. In this case, antidepressants are prescribed. The mechanism of action of these drugs is associated with inhibition of the reuptake of serotonin and norepinephrine, as well as blocking MAO (monoamine oxidase). These drugs improve mood, reduce tension and fear, and dysphoria.
Most antidepressants do not cause drowsiness.
The following antidepressants are used to treat depression during stroke:
- Fluoxetine (Prozac, Profluzac). It is a derivative of propylamine. Release form: gelatin capsules. Refers to serotonin reuptake inhibitors. Contraindicated in glaucoma, intolerance, kidney dysfunction, prostate hyperplasia, convulsions, epilepsy, as well as in pregnant and lactating women. The drug is not recommended for use simultaneously with MAO inhibitors.
- Deprim (Neuroplant). Contains dry extract of St. John's wort. Available in tablet form. It has a mild antidepressant, tonic, anxiolytic and sedative effect. Can be used from 12 years of age. Not for pregnant and lactating women. Side effects include allergic reactions.
- Phenazepam. A strong anxiolytic with anticonvulsant effect. Not prescribed for coma, myasthenia gravis, shock, suicidal thoughts, respiratory failure, alcohol poisoning.
- Imipramine. Tricyclic antidepressant. Contains imipramine hydrochloride. The peculiarity of the drug is that it has an analgesic effect and helps with urinary incontinence after a stroke. Prescribed for depression, ideation and motor retardation. Contraindicated in cases of hematopoietic disorders, cardiac, renal and liver failure, acute myocardial infarction, glaucoma, atony of the bladder muscles, prostate hyperplasia and pregnant women.
- Amitriptyline. Tricyclic antidepressant in tablet form. Affects serotonin metabolism and opioid systems. Can be prescribed to adults and children over 6 years of age. Effective for depression, anxiety, agitation (motor restlessness with agitation) and sleep disorders.
- Amixid. Contains amitriptyline and chlordiazepoxide. The indication is depression of various etiologies, including post-stroke. Amixide is not prescribed for decompensated heart disease, stage 3 hypertension, blood diseases, renal pathology, severe liver diseases, bladder atony, glaucoma, muscle weakness, peptic ulcer, children, pregnant and lactating women.
- Fevarin (Rokona). Contains fluvoxamine. Indications are treatment and prevention of depression.
If a patient with a stroke develops symptoms such as fear and anxiety, the following anxiolytics (tranquilizers) are used:
- Relanium and its analogues (Diazepam, Sibazon, Relium). They are used in the form of a solution for intramuscular and intravenous administration. They are benzodiazepine derivatives. The drugs depress the central nervous system and inhibit the transmission of impulses. They have a sedative, anxiolytic, anticonvulsant, hypnotic and muscle relaxant effect. Contraindicated in myasthenia gravis, glaucoma, shock, sleep apnea, obstructive pulmonary pathology.
- Grandaxin. The active ingredient is tofisopam. Release form: tablets. The medicine reduces seizures, has a minimal sedative effect, and calms the person. Prescribed for stroke accompanied by neuroses, depression, anxiety, apathy and myasthenia (muscle weakness). Contraindicated in respiratory failure, severe agitation, aggressiveness, galactose intolerance, sleep apnea, pregnant and lactating women.
- Atarax. Hydroxyzine-based tranquilizer. It has an antiemetic, moderate anxiolytic effect, reduces fear and anxiety. Not prescribed for porphyria.
- Selectra and its analogues (Cipralex, Elitseya, Escitalopram, Escipi). The active substance is escitalopram. Prescribed for depression and panic disorders due to stroke. Contraindicated for children over 15 years of age.
- Adaptol and its analogues (Mebicar, Mebix). Medicines relieve fear, anxiety, restlessness and irritability in people who have had a stroke. A special feature of the drugs is the presence of a nootropic effect. They improve cognitive functions of the brain, which is important in the recovery period after a stroke.
- Afobazol. Contains fabomotizol. Refers to selective anxiolytics with neuroprotective effects. For adults only.
- Anxiolytics with nootropic effects (Phenibut, Tenoten). The drugs improve the functional state of the brain, eliminate anti-anxiety and anxiolytic effects, reduce headaches, normalize sleep and reduce symptoms of asthenia. In conditions of acute tissue hypoxia, the affected areas are reduced.
Blood thinners
Blood thinners include antiplatelet agents and anticoagulants. They are effective for a tendency to thrombosis and increased blood viscosity, and are indicated for ischemic stroke. In case of cerebral infarction (hemorrhage), they are contraindicated.
Antiplatelet agents and anticoagulants
Antiplatelet agents are a group of drugs that thin the blood by disrupting the process of platelet adhesion.
These include:
- Thrombo Ass.
- Aspirin Cardio.
- Cardiomagnyl.
- Trombital.
- Thrombomag.
- Clopidogrel.
- Zilt.
- Plavix.
- Lopirel.
- Aegitromb.
Along with antiplatelet agents, anticoagulants are used for cerebral infarction. These drugs prevent thrombosis by inhibiting the blood coagulation system.
These include:
- Warfarin and its analogues (Warfarex). They are indirect anticoagulants. The drugs suppress the production of blood clotting factors 2, 7, 9 and 10. The action begins in 3-5 days. They are contraindicated in case of bleeding, kidney damage, liver disease, thrombocytopenia, DIC syndrome, hemorrhagic stroke and peptic ulcer.
- Eliquis. Direct acting anticoagulant. Contraindicated in the acute phase of stroke, bleeding, arteriovenous malformation, aneurysm, liver disease, malignant tumors, children and pregnant women.
- Heparin. It is used in the form of an injection solution. Affects antithrombin, which inhibits coagulation factors. Not prescribed for hypersensitivity, thrombocytopenia and bleeding.
Nootropics to improve brain function
- Nootropics are a group of neuroprotective drugs that improve brain activity and metabolic processes. These remedies help restore memory, speech and mental activity. An important property of nootropics is the ability to reduce the need for oxygen by brain cells. The mechanism of action is associated with increased ATP production and protein synthesis, improved utilization of glucose by brain tissue and stabilization of membranes.
- Nootropics include:
- Ceraxon and its analogues (Neypilept, Recognan).
- Lucetam and its analogues (Nootropil, Piracetam, Omaron). The drugs improve cognitive functions of the brain. Release form: tablets. Contraindicated in case of intolerance, severe renal failure, Huntington's chorea, intracerebral hemorrhage, pregnant and lactating women.
- Pantogam. Contains calcium pantothenate and pantogam. Has anticonvulsant effect. Reduces excitability, has a mild sedative effect, improves mental activity and performance. Contraindicated in case of kidney dysfunction, pregnant and lactating women.
- Encephabol. Contains pyritinol. Indicated for memory impairment, deterioration of thinking and brain dysfunction. Contraindicated in rheumatoid arthritis.
- Combined drugs (Fescetam, Combitropil, Piracezin, Phezam, Nookam). Contains piracetam and cinnarizine. These medications improve brain function and have a vasodilator and antihypoxic effect. Prescribed for cerebral infarction and during the recovery period of hemorrhagic stroke.
Blood pressure control drugs
Stroke is often accompanied by arterial hypertension. Elderly people with stroke and hypertension should be treated with antihypertensive drugs. They lower blood pressure by dilating blood vessels, blocking beta receptors, and inhibiting angiotensin-converting enzyme.
The most commonly used:
- ACE inhibitors (Captopril, Enalapril, Diroton, Lisinopril);
- beta-blockers (Metoprolol, Bisoprolol, Concor);
- diuretics (Diuver, Mannitol, Diacarb).
The pressure must be reduced gradually. Normally, it should not exceed 139/89 mm. Hg Art.
Venotonics to strengthen blood vessels
The list of drugs prescribed for stroke includes vasotonics and venotonics. They increase the tone of the cerebral arteries, make them more elastic and resilient, and reduce the permeability of blood vessels. This is important after a hemorrhagic stroke.
Venotonics include:
- Aescusan. Contains chestnut seed extract and thiamine. Release form: oral solution.
- Detralex. Has an angioprotective effect. Not prescribed for breastfeeding women.
- Troxerutin (capsules). Derivative of rutin (vitamin P). Reduces capillary permeability. Reduces tissue swelling.
Muscle relaxants to reduce muscle strain
In the first hours after the onset of a stroke, muscle spasticity (hypertonicity) is possible. Muscle relaxants are used to relax them and reduce tension.
The most commonly used:
- Mydocalm. Central acting drug. Contains tolperisone. The mechanism of action is associated with inhibition of reflex arcs and a decrease in the electrical activity of nerve cells. Contraindicated in myasthenia gravis and hypersensitivity.
- Lidamitol. Contains tolperisone and lidocaine. Relieves spasm of striated muscles. Contraindicated for children.
- Calmirex. Available in the form of a solution for injection. Prescribed for muscle spasms due to stroke.
Anticonvulsants
The first signs of a hemorrhagic stroke often include seizures. These are involuntary muscle contractions. Anticonvulsants are used to eliminate them.
The mechanism of action of these drugs is associated with blockade of sodium channels, suppression of impulse conduction and increase in the seizure threshold.
Anticonvulsants for stroke include Finlepsin, Tegretol, Carbamazepine, Lamotrigine, Convalis, Neurontin and Phenobarbital.
Dietary supplements and vitamins
Patients can take not only medications, but also dietary supplements and vitamins. The list of dietary supplements includes Glycine and Ginkgo Biloba. The latter contains ginkgo plant extract. The drug improves blood supply to the brain, saturates cells with oxygen, dilates blood vessels, and reduces aggregation. It is contraindicated in the acute period of stroke.
Vitamins used include B1, ascorbic acid, riboflavin, nicotinic and pantothenic acids. They improve brain function.
What conditions are necessary for a favorable prognosis?
Patients who were admitted to hospital on time survive. This should happen within 2-5 hours after the third stroke.
The chances of rehabilitation increase sharply if the person is young or the patient does not have concomitant diseases. The prognosis is more favorable for women than for men.
The chance of recovery decreases sharply if a person has been diagnosed with mental disorders. The prognosis will be favorable for people who have had a third apoplexy in the absence of severe neurological symptoms.
When a patient's movements in his arms and legs are restored within 90 days after paralysis and paresis, in some cases doctors are able to completely rehabilitate the health of such a patient. After 6-7 months, 50% of people with such symptoms can switch to full self-care. 30% of patients still need outside care.
If a person who has suffered a third apoplexy is lonely, then he has less chance of recovery than patients living in families.
Treatment with IVs and injections
Medicines used
The following can be administered by injection and infusion for stroke:
- sodium chloride solution maintaining blood pressure;
- thrombolytics (drugs that dissolve blood clots);
- anticoagulants (Warfarin);
- systemic glucocorticosteroids (Dexamethasone);
- colloidal solutions (for hemorrhage).
The use of glucose-containing solutions for stroke is inappropriate.
Catheter placement
Infusion medications are administered after catheterization. Catheters are either peripheral or central. In the first case, small vessels of the forearm, hand or foot are used for catheterization. The most common injection site is the radial vein.
Central access is used for large strokes when a person is in the intensive care unit or intensive care unit. The subclavian, jugular and femoral veins are used. They are located in the collarbone area, on the side of the neck and in the inguinal fold area, respectively.
How to determine the onset of a stroke
It is impossible to distinguish a transient ischemic attack from an irreversible acute circulatory disorder without medical assistance. Both situations require hospitalization. Serious attacks can be identified using a simple test:
- The patient needs to symmetrically extend both arms forward, then alternately touch his nose with each palm. The inability to do this, sudden disturbances in the trajectory of movements, and a distorted body are signs of an attack.
- When looking in the mirror or at your interlocutor, you should smile broadly, stick out your tongue far, and say a few words. A possible stroke is indicated by distorted or paralyzed corners of the mouth, deviation of the tongue to the side, and slurred speech.
- You must try to write on paper or type any text on the keyboard. During a stroke, this is very difficult to do; the result is a meaningless set of letters.
One or more alarming symptoms is a reason to urgently call for medical help or go to the hospital. The first 3 hours after a stroke are most important for restoring blood circulation and preventing irreversible brain damage. A doctor is also necessary in cases where health has recovered on its own.
List of effective drugs after stroke
For ischemic type
For ischemic stroke, the treatment regimen includes:
- antiemetics (Metoclopramide, Cerucal);
- statins;
- antihypertensive drugs;
- neuroprotectors (Semax, Mexidol, Actovegin, Piracetam, Cerebrolysin, Cavinton);
- antiplatelet agents (Clopidogrel, Aspirin);
- anticoagulants (Warfarin);
- thrombolytics;
- fibrinolytics.
Some of them (antiplatelet agents) have to be taken constantly (if there is a tendency to thrombosis).
After a hemorrhagic stroke
After a cerebral hemorrhage, the following can be used:
- decongestants (diuretics);
- some neuroprotectors (Actovegin, Vinpocetine);
- barbiturates;
- antihypertensive drugs;
- hemostatics;
- antifibrinolytics.
Drugs to improve cerebral circulation (Trental, Pentoxifylline) are contraindicated in acute hemorrhagic stroke.
First aid
If a stroke is suspected, the patient needs to wait for an ambulance, because it is the ambulance team that carries out the initial stabilizing measures.
At the Yusupov Hospital you can order an ambulance that will instantly take you to the hospital. When calling an ambulance, the patient's relatives and friends must explain to the dispatcher the symptoms that accompany a stroke. At the Yusupov Hospital, a qualified ambulance team, which specializes specifically in neurological diseases, responds to such calls. She drives a specially equipped vehicle in which emergency resuscitation measures and diagnostic tests can be carried out. Make an appointment
Prescribed drugs according to severity of manifestations
Initial symptoms
The use of medications for a stroke in the first three hours improves the prognosis for life and health and increases a person’s chances of recovery.
If the cause is thrombosis (there is a history of varicose veins, cases of ischemic stroke), then thrombolysis is performed.
Streptokinase or Thromboflux is used. If the cause is thromboembolism, then anticoagulants are effective. Intravenous administration of hypoosmolar agents during this period is contraindicated.
Acute conditions
In the acute period, after hospitalization and clarification of the diagnosis, pathogenetic and symptomatic therapy is carried out. To prevent thrombosis, antiplatelet agents and anticoagulants are prescribed (preference is given to low molecular weight Heparin), and sodium chloride solution is administered (for cerebral infarction). Already at the acute stage, neuroprotectors can be administered in the first hours. In case of hemorrhage, treatment in the acute period involves stopping the bleeding.
To stabilize the body's functioning
Infusions and antihypertensive drugs are used to maintain vital functions. If the cause of the stroke is cardiac pathology, then antiarrhythmic drugs (Amiodarone) and glycosides (Digoxin) can be used.
To increase the body's resistance to hypoxia and ischemia, antioxidants are used (Mexidol, Mexi B6, Medomexi, Metostabil and Mexiprim).
Recovery period
The rehabilitation period is aimed at restoring lost functions and improving the quality of life of patients who have suffered a stroke.
The doctor develops a rehabilitation program individually for each patient, taking into account the scale of the vascular accident, age, comorbid pathology, etc. Rehabilitation is aimed at restoring functions that are impaired due to damage to a certain area of the brain, so the stroke clinic depends on where the accident occurred and what its scale. For example, some patients lose the ability to move independently, others lose vision or hearing, problems with the respiratory system, discharge, etc. may occur. Therefore, in each specific case, a certain degree of recovery is possible. Sometimes it is not possible to rehabilitate the patient and return him to his usual way of life.
Neurologists at the Yusupov Hospital treat post-stroke pain syndrome, restore motor functions and motor skills, restore cognitive functions, etc. If necessary, they prescribe consultations with related specialists - cardiologists, ophthalmologists, etc. They teach relatives and friends about the specifics of caring for the patient. Given the high percentage of depression, it is possible to involve a psychotherapist.
In case of strokes, doctors assign a special role to the prevention of recurrent strokes, which includes proper nutrition, giving up bad habits, eliminating excess weight, and regular monitoring by a doctor.
High-level specialists using modern equipment and specially equipped rooms will be able to conduct a course of treatment and rehabilitation to help patients return to a normal lifestyle. You can make an appointment with a neurologist and rehabilitation specialist by calling the Yusupov Hospital.
What does traditional medicine offer?
Folk remedies for acute cerebrovascular accident are ineffective. After stabilizing the patient’s condition, tincture of Japanese sophora, a mixture based on vegetable oil and bay leaf, mummy with aloe juice (helps with thrombosis), infusion of celandine, tincture of juniper and sage, and tincture based on pine cones can be used to improve brain function. Even the most effective herbs cannot replace drug and surgical treatment.
Effective treatment of stroke: innovative technologies to protect your health
Therefore, the global medical community has developed not only a program whose goal is to prevent stroke, treating the consequences and restoring the body takes a large part in their research. Our specialists take an active part in scientific research and have created their own effective program that literally gets patients back on their feet. Modern treatment makes it possible to restore the functionality of the limbs, relieve dizziness and dysfunction of the speaking apparatus. Of course, once a stroke is diagnosed, hospital treatment becomes mandatory.
We are able to bring an atmosphere of home comfort into a hospital environment and provide psychological comfort to the patient. The stroke treatment center ensures that the patient will be provided with everything necessary, including equipment for rehabilitation and examination, the involvement of outside specialists and studies will not be needed anywhere else.
Stroke treatment is carried out in Moscow; convenient transportation simplifies contact between relatives and patients, and gives them the opportunity to visit the patient as much as possible and necessary.