Spinal stroke is an acute circulatory disorder in the spinal cord. This pathology is much less common than circulatory disorders in the brain, but this does not make it any less dangerous. Spinal stroke can be ischemic or hemorrhagic. This is a serious disease that requires mandatory and prompt hospitalization and fairly long-term treatment. In the absence of medical care, a spinal stroke can lead to loss of ability to work and disability.
In order to consult a specialist in time and begin timely treatment of spinal stroke, it is extremely important to know the symptoms of the disease and imagine the reasons for the development of this pathology.
General information about the blood supply to the spinal cord
The blood supply to the spinal cord comes from two pools: the vertebral-subclavian and the aortic. The spinal subclavian basin supplies the spinal cord in the upper sections: cervical and thoracic segments to Th3 (third thoracic segment). The aortic blood supply supplies the thoracic segments from Th4 and below, the lumbar, sacrococcygeal segments. From the vertebral artery, the subclavian artery and the aorta, the radicular arteries arise, which form the anterior spinal artery and two posterior spinal arteries that run along the entire spinal cord.
The blood supply to the spinal cord is very variable, the number of radicular-spinal arteries ranges from 5 to 16. The largest anterior radicular-spinal artery (up to 2 mm in diameter) is called the artery of the lumbar enlargement, or the artery of Adamkiewicz. Turning it off leads to the development of a characteristic clinical picture with severe symptoms. In a third of cases, one Adamkiewicz artery supplies the entire lower part of the spinal cord, starting from the 8-10th thoracic segment. In some cases, in addition to the artery of the lumbar enlargement, the following are found: a small artery entering with one of the lower thoracic roots, and an artery entering with the V lumbar or I sacral root, supplying the conus and epiconus of the spinal cord - the Deproge-Gotteron artery.
The anterior spinal artery system vascularizes 4/5 of the diameter of the spinal cord: the anterior and lateral horns, the bases of the dorsal horns, Clarke's columns, the lateral and anterior columns and the ventral sections of the dorsal columns. The posterior spinal arteries supply the posterior columns and the apex of the dorsal horns. There are anastomoses (natural connections of organs) between the systems.
Knowledge of the angioarchitecture (structure) of the spinal cord is necessary to understand the mechanisms of circulatory disorders and clinical diagnosis.
Key signs of stroke
With cervical osteochondrosis, doctors identify a number of signs that may indicate the development of a stroke:
- dizziness;
- constant headaches with increasing intensity;
- profuse sweating;
- chills;
- facial asymmetry;
- the appearance of dark spots before the eyes;
- problems with coordination of movements;
- loss of consciousness;
- feeling of lack of air;
- speech disorder;
- numbness of the limbs.
As the disease progresses, the signs of the disease become more pronounced.
Causes
There are many reasons leading to disruption of spinal blood flow. Most patients develop ischemic brain lesions (myeloischemia) and only occasionally hemorrhages (hematomyelia).
All reasons can be classified as follows. Primary vascular lesions: when the underlying pathology of the vessel itself.
- General somatic diseases – atherosclerosis, hypertension, acute heart failure, myocardial infarction, etc.;
- Vascular pathology and vascular malformations - aneurysms, stenoses, thrombosis, embolism, kinks and looping of blood vessels, varicose veins;
- Vasculitis – infectious-allergic, with syphilis, HIV infection.
Secondary vascular lesions: when the vessels are damaged by an external process.
- Spinal diseases – osteochondrosis, spondylolisthesis, tuberculous spondylitis, congenital synostosis;
- Diseases of the spinal cord membranes – arachnoiditis, leptopachymeningitis;
- Tumors of the spinal cord and spine.
Other reasons.
- Injuries (including during surgical interventions - radiculotomy with intersection of the radicular-spinal artery, aortic plastic surgery);
- Blood diseases;
- Endocrine diseases.
Of course, many patients experience several factors simultaneously in the development of the disease, which increases the risk of its occurrence. Whatever the cause of the circulatory disorder, the brain tissue that is not nourished or destroyed as a result of impregnation (compression) with blood ultimately suffers. Clinically, this is manifested by dysfunction of the affected area, which is what neurological diagnosis is based on.
Diagnosis of spinal stroke
Timely diagnosis of spinal stroke allows you to avoid negative consequences in the form of persistent paralysis, loss of ability to work and the ability to self-care. To carry out diagnostic measures, the following are used:
- X-ray image of the spine at the suspected site of a vascular accident - allows you to see stenosis of the spinal canal, affected areas of the spinal cord;
- puncture of the cerebrospinal fluid and analysis of the cerebrospinal fluid gives an idea of the pathological processes occurring in the structures of the spinal cord;
- Ultrasound and scanning of blood vessels allows you to find the area of rupture or ischemia;
- intravascular bypass surgery and stenting are performed simultaneously for diagnostic and therapeutic purposes in a specialized hospital.
Primary diagnosis is always based on a visual examination of the patient, medical history, and functional diagnostic tests.
Symptoms
Spinal stroke can be of two types:
- ischemic – spinal cord infarction;
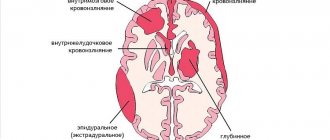
- hemorrhagic - hemorrhage into the thickness of the brain is called hematomyelia, hemorrhage under the membranes of the brain is hematorahis, epidural hematoma.
Ischemic spinal cord stroke
It develops equally often in men and women. More often, this disease affects people over 50 years of age, since the main cause is spinal pathology.
There are several stages during the course:
- Stage of distant and close precursors - a few days, weeks before the development of a heart attack, the patient begins to be bothered by motor disturbances in the form of short-term and transient weakness in the legs or arms (this depends on which vessel is affected - from the vertebral-subclavian or from the aortic basin). Sensory disorders are also detected in these same limbs: numbness, a crawling sensation, chilliness, burning, and simply unpleasant sensations in the muscles. Sometimes there may be an urgent urge to urinate, retention or increased frequency of urination. Pain in the spine may be bothersome, spreading to the upper or lower extremities, associated with impaired nutrition of the sensitive roots and membranes of the spinal cord. With the development of a stroke, the pain goes away, which is associated with a break in the passage of pain impulses in the affected area. Predisposing factors are often identified: alcohol consumption, physical stress, overheating, sudden movements in the spine.
- Stage of development of a heart attack - within a few minutes or hours, severe muscle weakness (paresis) develops in the limbs, sensitivity in the same limbs is lost, and pronounced dysfunction of the pelvic organs appears. The pain syndrome stops (the reasons are described above). At the time of stroke development, symptoms of brain damage (reflex) are also possible: headache, dizziness, fainting, nausea, general weakness. The clinical picture of damage to a particular part of the brain depends on the location of the affected vessel.
- Stage of stabilization and reverse development - symptoms stop increasing and regress against the background of adequate treatment.
- The stage of residual effects is the residual effects of a stroke.
Depending on which part of the brain is affected, the following clinical syndromes are distinguished:
- with damage to the anterior spinal artery in the uppermost sections - tetraparesis (all 4 limbs) of a spastic type, impaired pain and temperature sensitivity in all limbs, signs of damage to the 5th and 12th pairs of cranial nerves;
- with damage to the anterior spinal artery in the area of the upper cervical segments - the same as in the previous paragraph, but without damage to the cranial nerves;
- with damage to the anterior spinal artery in the area of the pyramidal decussation - cruciate hemiplegia: paresis of the arm on the side of the lesion and the leg on the opposite side;
- subbulbar Opalski syndrome - on the side of the lesion, paresis of the limbs, impaired sensitivity on the face, ataxia, sometimes Claude-Bernard-Horner syndrome (ptosis, miosis, enophthalmos). On the opposite side there is a violation of superficial sensitivity on the limbs and trunk;
- amyotrophic lateral sclerosis type syndrome - peripheral or mixed paresis of the upper extremities, spastic lower extremities, possible involuntary twitching of the muscles of the shoulder girdle;
- Personage-Turner syndrome - severe pain in the upper arms, followed by paralysis. With the development of paralysis, the pain goes away;
- anterior ischemic poliomyelopathy syndrome - peripheral paresis of one or both arms;
- ischemic pseudosyringomyelia syndrome - segmental disorders of surface sensitivity and mild muscle paresis;
- ischemia syndrome of the marginal zone of the anterior and lateral cords - spastic paresis of the limbs, cerebellar ataxia, slight decrease in sensitivity;
- syndrome of damage to the superior accessory radicular-spinal artery (middle thoracic segments) - spastic paresis of the legs, impaired pain and temperature sensitivity from the level of the nipples and below, impaired urination by type of retention;
- Brown-Séquard syndrome - paresis in one limb or on one half of the body (i.e., for example, in the right arm and leg), impaired pain and temperature sensitivity on the other side;
- pathology of the Adamkiewicz artery - paresis of both legs, disturbance of all types of sensitivity from the lower thoracic segments, dysfunction of the pelvic organs. Bedsores develop quickly;
- paralyzing sciatica syndrome - with damage to the inferior accessory radicular spinal artery (Deproge-Gotteron artery). Usually develops against the background of long-term lumbosacral radiculitis. Manifests itself in the form of paralysis of the lower leg muscles with foot drop. The pain syndrome disappears with the development of paresis. Sensory disturbances from the level of the lumbar or sacral segments are also observed. On examination, Achilles reflexes are not detected;
- conus syndrome (lower sacral segments) – paralysis does not occur. There are disorders of the pelvic organs – urinary and fecal incontinence. Patients do not feel the urge, do not feel the passage of urine and feces;
- pathology of the posterior spinal artery (Williamson syndrome) - a violation of deep sensitivity in the limbs develops (with sensitive ataxia) and moderate paresis in the same limbs.
Great variability in the structure of the vascular system of the spinal cord creates difficulties in diagnosing the lesion, but a competent specialist will always be able to make the correct diagnosis.
Hemorrhagic stroke of the spinal cord
When hemorrhaging into the substance of the spinal cord (hematomyelia), acute girdling pain occurs in the torso with the simultaneous development of paralysis in one or more limbs. Paralysis is often peripheral (flaccid) in nature. In these same limbs there is a violation of pain and temperature sensitivity. With massive hemorrhages, the development of tetraparesis with disturbances in the sensitivity and functions of the pelvic organs is possible. Combinations of clinical symptoms can be very different, as with ischemic stroke. The size of the hematoma plays a big role: small ones can resolve without leaving any signs behind during treatment; large ones always have residual effects.
Hematorahis is another type of hemorrhagic stroke, which is quite rare. In this case, hemorrhage occurs in the subarachnoid space of the spinal cord. More often the cause is a rupture of an abnormal vessel (aneurysm, malformation), spinal cord or spine injury. After the provoking factor, a pronounced pain syndrome develops along the spine or encircling nature. The pain can be shooting, throbbing, “dagger-like”, and lasts for several days or even weeks. At the time of hemorrhage, general cerebral symptoms may be observed: headache, nausea, vomiting, dizziness, impaired consciousness such as stunning. Some symptoms of irritation of the meninges appear: Kernig's sign is more clearly expressed, but there is no stiff neck at all. Symptoms of damage to the substance of the spinal cord are either absent altogether or appear later and are moderate in nature.
Epidural hematoma is characterized by sharp local pain in the spine combined with radicular pain and slowly increasing symptoms of spinal cord compression. Local pain is of the same type, prone to recurrence, remission from several days to several weeks.
Diagnostics
Diagnostic measures begin with collecting anamnesis. What matters is the presence of the precursor stage, acute/subacute onset, and the sequence of development of symptoms. A motor/sensory deficit identified during a neurological examination allows the neurologist to suggest a topical diagnosis, however, the variety of individual variants of the spinal blood supply makes it difficult to determine the location of vascular occlusion or rupture. In order to clarify the diagnosis, instrumental studies are carried out:
- Tomography of the spine
. Computed tomography allows you to determine displacement, damage to the vertebrae, the presence of fragments, osteophytes, and narrowing of the intervertebral space. MRI of the spine better visualizes the spinal cord and makes it possible to diagnose intervertebral hernia, compression of the spinal canal, spinal tumor, and hematoma. - Lumbar puncture
. In 30% of patients, cerebrospinal fluid examination does not reveal any abnormalities. In most patients at the stage of development of the pathology, an increase in protein concentration to 3 g/l is observed, pleocytosis is 30-150 cells in 1 μl. The hemorrhagic variant is accompanied by the appearance of red blood cells in the cerebrospinal fluid. - Spinal angiography.
It is carried out to identify aneurysms, malformations, thrombosis, and external compression of the vessel. A simpler, but less informative study of spinal circulation in the thoracic and lumbar regions is an ultrasound scan of the aorta and its branches. - Electroneuromyography
. Necessary for detecting a clinically undiagnosed disorder of the innervation of individual muscles.
To determine the causative background pathology, according to indications, consultations are held with a therapist, cardiologist, endocrinologist, hematologist, blood is examined for sugar, lipoprotein levels, cholesterol, and a coagulogram is performed. Differential diagnosis is carried out with acute myelitis, spinal cord tumor, infectious myelopathy, syringomyelia, epidural abscess. Important for determining treatment tactics is the differentiation of hemorrhagic and ischemic stroke.
Treatment
Treatment tactics are determined individually after an accurate diagnosis of the nature and localization of the process. For example, if the cause of a stroke is severe osteochondrosis with a disc herniation, vascular anomaly or tumor, then it is worth considering the possibility of surgical treatment.
For the treatment of ischemic stroke of the spinal cord, the following is used:
- anticoagulants and antiplatelet agents – heparin, fraxiparin, aspirin, Plavix, clopidogrel, chimes (dipyridamole), trental;
- vasoactive drugs - Cavinton, pentoxifylline, oxybral, nicergoline, instenon, enelbin, xanthinol nicotinate;
- venotonics – troxevasin, aescusan, cyclo-3-fort
- neuroprotectors – actovegin, tanakan, cerebrolysin, cytochrome C, nootropil, riboxin;
- angioprotectors – ascorutin, calcium dobesilate, troxerutin;
- hemodilution – fresh frozen plasma, low molecular weight dextrans (reopliglucin, reomacrodex);
- decongestants – diuretics (furosemide, Lasix), L-lysine escinate;
- non-steroidal anti-inflammatory drugs – diclofenac, Celebrex, nimesulide, ibuprofen;
- agents that improve neuromuscular conduction – neuromidin;
- to reduce muscle tone - mydocalm, baclofen;
- B vitamins – neurorubin, milgamma.
Additionally used (depending on the cause of the stroke): immobilization of the affected spinal segment, traction, drug blockades, massage, exercise therapy, and physical therapy methods.
Conservative treatment of hemorrhagic stroke involves the use of:
- drugs that strengthen the vascular wall, helping to prevent recurrent hemorrhage - dicinone (sodium etamsylate), contrical, gordox, aminocaproic acid;
- drugs for the prevention of vasospasm - nimotop, verapamil;
- neuroprotectors and angioprotectors.
If conservative treatment is ineffective and in cases of spinal cord injuries or tumor formations compressing the brain, surgical treatment by a neurosurgeon is indicated.
A special role in the treatment of spinal strokes is played by the prevention of bedsores, pneumonia and urogenital infections, which often complicate this disease with insufficient patient care.
To avoid bedsores, it is necessary to monitor the cleanliness of underwear, wipe the body with camphor alcohol, dust the folds of the skin with talcum powder, and turn the patient over every 1-1.5 hours. You can use special devices for the prevention of bedsores - a rubber circle, rings.
If it is impossible to urinate on your own, bladder catheterization is performed; in case of incontinence, urinals are used. The genitals must be kept clean to prevent ascending infection.
To avoid the development of pneumonia, it is necessary to perform breathing exercises every hour for 5 minutes (while bed rest is maintained). In the future, when expanding the regime, dosed physical activity is necessary.
Consequences
The consequences of a spinal stroke can be very different. If the lesion is small in size and timely drug therapy or surgical treatment is possible, a 100% recovery is possible, but the patient must undergo clinical observation and preventive treatment courses. A less favorable outcome is also possible when, despite treatment, the patient remains with motor, sensory and pelvic disorders. Such disorders can lead to disability:
- paresis of the limbs (one or more) – weakness in the muscles persists, which makes independent movement and self-care difficult;
- areas of hypoesthesia or anesthesia - on the trunk or limbs there is reduced or absent sensitivity. This can be pain, temperature, tactile sensitivity, as well as more complex types of sensitivity, such as a sense of localization, stereognosis (recognition of objects by touch with eyes closed), two-dimensional spatial sense (the ability to recognize letters and numbers drawn on the body with eyes closed). ) etc. For some patients, this may cause loss of ability to work - a seamstress or musician cannot perform professional skills if there is no sensitivity in the hands;
- disorders of urination and defecation - this problem is especially painful for patients, as it affects the intimate sphere of a person. Variations in the degree and nature of the disorder are possible: urinary incontinence, constant dribbling of urine, periodic uncontrolled urination, the need to strain to urinate, fecal incontinence.
Diagnostics
Diagnosing a spinal stroke, especially the ischemic form, can be quite difficult, since it has common symptoms with poliomyelitis, the spinal type of multiple sclerosis, and cerebellar dysfunction.
Knowing which part of the spinal column is responsible for sensitivity and muscle contraction in a particular area of the body, the neurologist can establish a preliminary localization of the ischemic focus.
To confirm the diagnosis, the patient is prescribed instrumental studies:
A general blood test and spinal puncture with further study of the biomaterial are mandatory.
Recovery
Recovery from a spinal stroke can be lengthy. It is most active in the first 6 months. First of all, such patients need psychosocial adaptation, since a spinal stroke dramatically changes their usual way of life. Recovery after a spinal stroke is a long and laborious process; sometimes it takes years to restore lost functions. However, high-quality rehabilitation measures after hospital treatment allow most patients to return to a full life.