Multiple sclerosis is a pathology of the nervous system, which was previously considered incurable, but is now recognized as completely conquerable. A stem cell transplant for multiple sclerosis offers a chance for recovery. This innovative technique is not recognized in all countries.
However, it has already proven itself to be excellent - after the operation, people’s quality of life improves significantly. In the future, the issue of widespread introduction of this method of treating multiple sclerosis is being considered.
Causes and provoking factors
For a more complete understanding of how to choose the optimal treatment regimen for multiple sclerosis - whether it will be possible to perform a stem cell transplant, the doctor initially finds out the reason why the disease developed.
Experts have not reliably established why people develop multiple sclerosis. Most often the following provoking factors are indicated:
- genetic predisposition - if relatives have already had cases of multiple sclerosis, then the child may well develop the disease;
- excessive intellectual stress – work activity associated with the risk of psychological instability and severe stress;
- weakened immune system – frequent infections, especially those affecting brain structures;
- autoimmune diseases - the body perceives its own tissues as foreign, and produces protective cells against them, so there is a chronic inflammatory process that undermines the nervous system;
- bad habits – multiple sclerosis is observed in people whose experience of abusing alcohol and tobacco products exceeds 20-30 years.
Some experts consider a person’s residence in the northern regions and his attitude towards the white race to be provoking factors for multiple sclerosis.
Pros and cons of the method
This treatment method is highly effective in treating multiple sclerosis that is resistant to standard drug treatment.
This provides a higher standard of living for patients suffering from this disease.
Multiple sclerosis is a pathology prone to gradual progression and deterioration in the standard of living of patients. For the purpose of treatment, it is possible to use a bone marrow stem cell transplant, but this procedure can only be performed in specialized centers.
Symptoms and signs
To begin treating a disease, you first need to recognize it. Since the pathology is based on damage to the nerve fibers along which impulses travel from the brain to the internal organs, the clinical picture will depend on in which part of the body the pathological focus has formed.
Manifestations of multiple sclerosis:
- trembling of the limbs - at first barely noticeable and periodic, it intensifies as the disease progresses, becoming widespread and prolonged;
- disturbance of the perception of the body in space - when moving, the feet seem to lose the feeling of solid ground, “walking on wobbly legs”;
- coordination of movements loses its clarity - from the outside a person may seem drunk;
- loss of control over the facial nerves - part of the face shifts to one side;
- tingling in certain areas of the skin - a feeling of numbness;
- pathological strengthening or weakening of muscle tone;
- failure in the process of urination - most often due to incontinence.
Neurological symptoms will be expressed in changes in the patient’s mood, tearfulness or euphoria, attacks of depression and decreased self-esteem.
Before deciding whether a stem cell transplant is permissible, the doctor must conduct a thorough neurological examination and instrumental studies of the nervous system.
Traditional treatments for multiple sclerosis
Unfortunately, until recently, multiple sclerosis was considered an incurable disease. Traditional methods were aimed at alleviating the symptoms of the disease; they could slow down its development and delay the onset of a new relapse. Drugs - such as interferon, Copaxone or immunosuppressants - suppressed the immune response, inhibited the process of demyelination, but did not restore existing damage to nerve fibers. In other words, they were powerless to restore lost functions to the patient.
Description of the transplantation technique
The uniqueness of stem cells is that they are already present in the human body and have the ability to differentiate into those areas of the body where they are located. In Russia, the transplantation technique for multiple sclerosis is standardized and officially approved.
Stem cell therapy for the disease leads to the restoration of the myelin sheath of the brain nerve fibers, which was damaged by foci of fibrous tissue. The transplantation technique also has a positive effect on the immune system, the state of which is important for the course of the disease.
Multiple sclerosis is treated with stem cells if previously carried out therapeutic measures - taking medications, physiotherapy, sanatorium-resort treatment - have not brought a significant improvement in the person’s condition. In this case, the collection of biomaterial for transplantation is carried out directly from the patient himself.
In this case, the risk is reduced:
- introduction of infections;
- provoking mutations in cells - the appearance of oncology;
- immunological mismatch.
In general, stem cell transplantation is a proven method that has previously been used to get rid of other diseases. It turned out to be promising for stopping pathological processes characteristic of multiple sclerosis.
When is this method used?
At the current time, there are no methods of therapy that would lead to a cure for the disease. But the diagnosis of multiple sclerosis is treatable and responds quite well to therapy.
The goal of therapeutic intervention is to stabilize the course of the patient’s pathology, as well as to prevent recurrent exacerbations.
During exacerbations, medications from the group of glucocorticosteroid hormones (suppression of the immune response to the cellular structures of one’s own body), as well as plasmapheresis, aimed at removing autoantibodies from the patient’s body, are widely used.
Interferons and monoclonal antibodies are also used for treatment, but their use is expensive.
Therefore, in order to treat this pathological process, a new therapeutic method is increasingly being used - high-dose chemotherapy with further bone marrow (stem cell) transplantation.
Stem cells are cellular structures that undergo differentiation to form different types of cells. These structures, localized in the red bone marrow, are called hematopoietic (hematopoietic).
The drugs used in polychemotherapy ensure the destruction of antibodies directed against the body's own structures (in the disease in question - the myelin sheath of the nerves), and subsequent transplantation provides a functional restructuring of the immune system, the result is a stable course of the pathology in patients and a decrease in the frequency of exacerbations.
A bone marrow donor can be a person in the age range from 18 to 45 years, who does not have any mental disorders or contraindications to the collection of stem cell structures.
Persons with:
- infectious pathologies: HIV infection, syphilis, viral hepatitis, tuberculosis, brucellosis, typhus, tularemia, leprosy;
- parasitic pathologies: toxoplasmosis, echinococcosis, filariasis, leishmaniasis;
- malignant neoplasms;
- hematological pathologies;
- diseases of the cardiovascular system: high-grade arterial hypertension, coronary heart disease, atherosclerotic lesions, obliterating arteritis, thrombophlebitis, heart defects, inflammatory diseases of heart tissue;
- diseases of the respiratory tract: bronchial asthma, obstructive bronchitis, emphysema, severe diffuse sclerosis;
- pathologies of the gastrointestinal tract: gastric and duodenal ulcers, Achilles gastritis;
- diseases of the biliary tract: cholelithiasis, chronic liver pathologies of various origins, cirrhosis of the liver;
- pathologies of the urinary system: damage to the renal tissue, nephrolithiasis;
- connective tissue diseases;
- pathological conditions of the endocrine system;
- pathologies of the ENT organs: severe purulent-inflammatory diseases, acute or during an exacerbation of the chronic type of course, ozena;
- diseases of the organ of vision: high myopia (myopia), trachoma;
- diseases of the skin: fungal infections, psoriasis, pustular diseases.
Hematopoietic stem cells can be collected in one of the following ways:
- From the bone marrow: under general anesthesia in a hospital setting, a puncture of the pelvic bone is performed using a special syringe. The duration of the operation does not exceed half an hour.
- From venous blood: a special medication is taken that promotes the release of hematopoietic cells into the systemic circulation, blood is taken from the vein, and it is processed with a special device that retains these cells. The rest of the blood is then transfused to the donor through a vein on the other limb.
Stages of transplantation
The procedure for restoring the myelin sheath of a nerve fiber by transplantation is the main goal of therapy for multiple sclerosis, and is carried out in three stages. As a rule, specialists first assess the initial state of a person’s health and determine the stage at which the disease is located.
Then you need to obtain biomaterial for transplantation - stem cells. To do this, blood is taken from a person - through a standard intravenous system it enters a specially designed device. It is he who helps differentiate the necessary ones from hundreds of thousands of blood cells.
There may be a small number of them in the peripheral bed. Sometimes, to obtain the required volume, 3–4 procedures are performed. The cells are then frozen and stored until transplantation.
At the second stage of transplantation, it is necessary to destroy immune cells already damaged by the pathological process. In order to solve this problem, the following is introduced into the human body:
- immunosuppressive medications - suppress unhealthy immune system activity that damages the myelin fiber of nerve endings;
- anti-inflammatory drugs - reduce the severity and extent of inflammatory foci in both the brain and spinal cord.
The complex effect allows you to prepare the human body for further stem cell transplantation. They are defrosted in a special mode and then enter the bloodstream through the intravenous system. All stages of transplantation are carried out in specialized hospital clinics.
Expected result - video
Stem cell therapy for multiple sclerosis is a huge step in the treatment of pathology. The results of transplantation in people are usually observed by the end of the second or third month.
Effects of transplantation:
- chronic fatigue is eliminated;
- trembling in the limbs decreases;
- the mental state is normalized;
- confidence in future health appears;
- symptoms of urinary incontinence disappear;
- speech gains coherence and clarity;
- gait becomes more confident.
With early diagnosis of multiple sclerosis and timely administration of stem cells, complete recovery is possible - the disappearance of foci without myelin in the nerve fiber.
- The Almazov Center performed a rare bone marrow transplantation for children
- Russia's first rehabilitation department for patients with MS opened at the hospital on Krestovsky
- In St. Petersburg you can get tested for antibodies to the SARS-CoV-2 coronavirus
First Honey is reviving the method of treating severe autoimmune diseases using the transplantation of one’s own stem cells. It is currently being used for patients with multiple sclerosis as part of a clinical trial. Although the method already has its own history.
— Alexey Yurievich, stem cell transplantation for patients with such an autoimmune disease as multiple sclerosis began in the world at the very beginning of this century. And they abandoned it very quickly. Why did you return to this method?
That is, at the beginning of the century, problems remained, and even today little has changed. Since transplantation was perceived as a therapy of despair, it was prescribed to those who did not respond to drug therapy. And these are years. As a result, the effectiveness of the transplant looked, to put it mildly, low, especially taking into account the expectations of patients who thought that after it they would start running.
Multiple sclerosis (MS) is an autoimmune disease that affects the myelin sheath of the nerve fibers of the brain and spinal cord, which leads to severe motor and other disorders, including profound disability.
— What do you know about the fates of those patients who underwent transplantation then?
— The experience of using hematopoietic stem cell transplantation for patients with multiple sclerosis has approximately the same history as that of DMTs (drugs that modify the course of multiple sclerosis). A total of 45 people received treatment with its use at our university. I talk and meet people who had transplants more than 15 years ago. Among those who underwent treatment in the 2000s, there are several people who received the method on time. In the spring, a woman came to me who had undergone HSCT at the age of 37. Now she is 51 years old - she came running in heels, she now has no limitations in function, only minimal symptoms detected during a neurological examination, which corresponds to 1 point on the EDSS scale (this scale is used to assess the degree of disability of the patient, in which up to 4.5 points - fully preserved mobility, above 7 - deep disability - Ed.). That is, everything, including HSCT, must be done on time and according to indications, and then there will be success, because with multiple sclerosis there is a simple formula - the fewer foci in the brain, that is, the lower the degree of disability, the more effective the treatment, if prescribed timely and targeted.
In those patients who were transplanted at the Research Institute named after. Gorbacheva with 6-7 points on the EDSS scale, over this long period the neurological status increased from 0 to 1.5 points. This suggests that anti-inflammatory therapy still played a role, and the progression of the disease in most of them was at least slowed down. Therefore, in addition to the hematological service, the determination of the neurologists who participated in the fate of the patients and recommended this method of treatment to them also requires great respect.
— If previously patients with multiple sclerosis were referred for HSCT when drug therapy was no longer effective, how does this happen now?
Of course, when communicating with a patient, we first try to explain that the existing principles of care for patients with multiple sclerosis in our country are completely justified, and sometimes patients are on DMT for a long time without relapse of the disease. If the patient insists, additional diagnostics and scrupulous work by specialists are required to determine the indications for using the method and to exclude other diseases similar to multiple sclerosis.
— What is the point of transfusing your cells in case of autoimmune diseases? The body will produce the same ones.
— What should a patient who would like to undergo a transplant do?
— Still, I would like the motivation to carry it out to come from the attending physician. If at all previous stages of treatment the possibilities have been exhausted and the neurologist makes a decision to perform HSCT for neurological indications, then readiness for treatment in a hematological transplant hospital (and nothing else) consists of the absence of active inflammatory and severe concomitant pathology.
— What is the transplantation process? Sounds scary.
While the resulting cells are being prepared for transplantation, the patient's bone marrow function is restored. At the next stage, high-dose immunosuppression (administration of a chemotherapy drug) is carried out, and then the patient’s own, previously prepared, cells are transfused into a vein. Thus, this is not a surgical operation in the classical sense, but a complex therapeutic operation. Then begins the stage of restoring blood parameters that change as a result of chemotherapy. Hospitalization lasts no more than 30 days in total.
— There are quite a lot of autoimmune diseases, this is not only multiple sclerosis, systemic lupus erythematosus, scleroderma, rheumatoid arthritis, vasculitis, antiphospholipid syndrome, etc. Are there attempts to treat them in the same way?
The first HSCT for autoimmune diseases in our country was performed at the Research Institute of Physical Culture in Novosibirsk in 1998. St. Petersburg professors Andrei Novik and Boris Afanasyev were also at the origins of HSCT for multiple sclerosis. The first dissertation in Russia on this topic was defended in 2006 at PSPbSMU named after. Pavlova. In St. Petersburg, treatment of patients with multiple sclerosis was initially carried out in collaboration with neurologists at the Research Institute of Children's Oncology, Hematology and Transplantology named after. R.M. Gorbachev, as a member of the European Society for Blood and Marrow Transplantation (EBMT).
Multiple sclerosis is a pathological process with a chronic course that affects the central nervous system and is characterized by demyelinating processes of autoimmune origin.
There is standard therapy for multiple sclerosis, carried out according to clinical guidelines. There are also new methods of treating this pathology.
We will talk about the treatment of multiple sclerosis using stem cell transplantation and its effectiveness in the article.
What affects the outcome of treatment
In order for the treatment of multiple sclerosis with stem cells to produce a significant result - increasing the quality of life and improving the functioning of internal organs, a number of conditions must be met.
Even a 20-30% chance of transplant success is always better than nothing at all, which was a reality at the end of the 20th century in patients with multiple sclerosis.
Obtaining high transplant results is influenced by:
- stage of the disease;
- rate of disease progression;
- patient's age;
- tissue susceptibility to therapy;
- the presence of concomitant severe diseases.
Thus, people with the initial stage of multiple sclerosis have every chance of recovery if a stem cell transplant is performed in a timely manner. Regeneration of the myelin sheath of the nerve fiber after transplantation occurs much faster. The disease completely recedes.
Excellent results were demonstrated by people who had multiple sclerosis for no more than 7-8 years. After several transplantation sessions, even those areas whose damage was about 70-80% were restored.
If multiple sclerosis has a severe progressive course, then transplantation allows one to achieve a stage of long-term remission of the disease - mental activity improves, and movement disorders become less pronounced.
Research results and procedure
Bone marrow transplantation is a recognized method in the treatment of many diseases.
Especially in oncology, in some cases it turns out to be the only way to save the patient’s life. Bone marrow is found inside the pelvic bones and the extended ends of the long bones and is responsible for the formation of blood cells. Red blood cells, erythrocytes, carry oxygen to all organs and tissues, white blood cells, leukocytes, provide immunity against infections, and platelets are involved in blood clotting. As a result of certain diseases and certain influences, the bone marrow loses its ability to form blood and needs to be replaced or transplanted.
To date, more than 50,000 bone marrow transplant procedures have been performed worldwide, with up to 5,000 new procedures performed every year.
Here are some diseases for which transplantation is performed: severe aplastic anemia (blood formation disorders), thalassemia, congenital immunodeficiencies, storage diseases (Gaucher disease, mucopolysaccharidosis), leukemia, malignant non-Hodgkin lymphoma, Hodgkin disease, multiple myeloma. Transplantation is also performed after radiation or chemotherapy, which is necessary for a wide range of malignant diseases. Intensive immune suppression in severe autoimmune diseases such as systemic lupus erythematosus, scleroderma or multiple sclerosis also requires bone marrow transplantation.
Multiple sclerosis (MS) is a chronic demyelinating, autoimmune disease of the nervous system, which is based on increased permeability of the blood-brain barrier to activated peripheral blood T-lymphocytes with subsequent damage to myelin in the central nervous system, leading to a progressive increase in neurological deficit and disability of patients. The disease mainly affects young, working-age people and most often occurs between the ages of 20-40 years.
Multiple sclerosis is a common disease, occurring with a frequency of 10-60 per 100 thousand population per year. Currently, the European Bone Marrow Transplantation Group has registered 320 patients with multiple sclerosis who have undergone high-dose therapy with hematopoietic stem cell transplantation. In Russia, data on hematopoietic stem cell transplantation for multiple sclerosis are registered in the database of the Russian Cooperative Group of Cell Therapy, whose central office is located in the National Medical and Surgical Center named after. N.I. Pirogov.
Unlike many commercial centers offering dubious methods for treating multiple sclerosis with stem cells that do not comply with the protocol of the European Bone Marrow Transplantation Group, clinical centers included in the Russian Cooperative Cell Therapy Group carry out transplantation in full accordance with the requirements of the protocol. Currently, the registry of the Russian Cooperative Cell Therapy Group includes 465 patients with various forms of multiple sclerosis who have undergone hematopoietic stem cell transplantation.
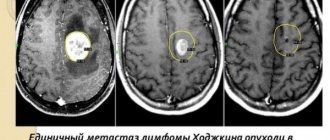
The effectiveness of this type of transplantation for multiple sclerosis is very high. In patients who have already received various types of treatment (prednisolone, metipred, betaferon, Avonex, Rebif, Copaxone, immunoglobulins, cyclophosphamide, mitoxantrone, plasmapheresis, etc.) without significant effect, stem cell transplantation leads to long-term remission during the disease more than in 80% of patients. Moreover, in a number of patients, remission (sustained improvement in condition in the absence of signs of disease progression according to magnetic resonance imaging) after stem cell transplantation persists for 10 years. This phenomenal result of stem cell transplantation for multiple sclerosis is not achievable today using other treatment methods.
Research on this topic continues to this day. Specialists from a number of medical centers in Canada conducted a study of the reasons for the effectiveness of bone marrow transplantation in the treatment of particularly aggressive forms of multiple sclerosis. The transplant itself, a procedure fraught with serious risks, was carried out as part of a clinical trial. First, chemotherapy is performed, followed by a transplant of the patient's own stem cells.
As shown by the results of MRI scans of the brain, such treatment can reduce relapses of the disease to almost nothing. The study made it possible to determine how the immune system changes as a result of this operation. It has been established that as a result of transplantation, the activity of T-helper 17, immune cells that enhance the adaptive immune response, is significantly weakened.
In people with multiple sclerosis, the researchers note, Th17 is able to cross the blood-brain barrier, allowing other immune cells, such as Th1, which are also thought to be involved in damaging neurons, to invade the brain. According to scientists, it is Th17 that is responsible for relapses of aggressive forms of the disease.
When bone marrow cells removed from the bone are transplanted into a patient, it is called a bone marrow transplant. If hematopoietic stem cells taken from peripheral blood are transplanted, then we are talking about blood stem cell transplantation. Before transplantation, so-called conditioning (preparation) of the patient is performed, which consists of removing possible residual tumor cells and suppressing one’s own immunity to prevent rejection. Such preparation depends on the underlying disease and includes chemotherapy or chemotherapy in combination with radiation therapy. If your own cells are obtained before chemotherapy or radiation therapy, they are frozen at -195°C and stored until the appropriate moment.
For transplantation, it is not the bone marrow itself that is valuable, but the hematopoietic blood stem cells (precursor cells of hematopoiesis) contained in it. These cells are also present in small numbers in the peripheral blood. Therefore, these cells can be collected in two ways - directly from the bone marrow or from peripheral blood. In the first case, a bone marrow puncture from the iliac crest is required under general or local anesthesia. The operation lasts about 30 minutes. But in recent years, a second, more advanced method has gained popularity - collecting hematopoietic cells from the blood. To increase the number of hematopoietic cells in the blood, the donor takes a special drug the day before.
Stem cells are an effective treatment for multiple sclerosis, eliminating autoimmune attacks on nerve cells and restoring all body functions. The best doctors in Europe and the world!
Multiple sclerosis is a pathology of the nervous system, which was previously considered incurable, but is now recognized as completely conquerable. A stem cell transplant for multiple sclerosis offers a chance for recovery. This innovative technique is not recognized in all countries.
However, it has already proven itself to be excellent - after the operation, people’s quality of life improves significantly. In the future, the issue of widespread introduction of this method of treating multiple sclerosis is being considered.
Cost of treatment
Of course, prices for transplant procedures can vary significantly from one region to another. The final cost of the transplant will be influenced by:
- level of medical institution;
- the need for an expensive preliminary examination;
- number of stem cell collection sessions;
- conducting additional consultations with other doctors.
Thus, Moscow centers offer similar services at the highest prices - up to 700-800 thousand rubles for transplant courses. While in other regions the cost may be lower. In foreign clinics, such treatment for multiple sclerosis is even more expensive.
The final cost of the transplant will be affected by the price of each stage of treatment - stem cell collection, the use of immunosuppressive medications, as well as the transplant itself. Such treatment should be trusted to truly trusted clinics with extensive experience in the treatment of multiple sclerosis.
Transplantation of hematopoietic cell structures
Transplantation of hematopoietic stem structures can be:
- autologous – material is collected and subsequently transplanted from the patient himself;
- allologous – stem cells are collected from a donor and subsequently transplanted into the patient.
Indications for transplantation of hematopoietic structures are:
- diagnosis of multiple sclerosis with progressive neurological symptoms over the past 12 months confirmed by clinical data and MRI results by more than 1 point on the EDSS scale;
- lack of effectiveness from previous combination treatment;
- age range from 18 to 45 years;
- age-sex and clinical-laboratory results corresponding to the norm;
- ability for self-care and independent movement.
Transplantation is not performed if:
- pregnancy period in MS;
- lactation period;
- severe concomitant pathology;
- pronounced deviations from age, sex and clinical laboratory results;
- life-threatening bleeding;
- mental status changes;
- presence of oncopathology;
- acute course of the inflammatory process localized in the oral cavity or in the paranasal sinuses.
The treatment program through transplantation of autologous structures includes:
Possible side effects include:
- the occurrence of infectious and inflammatory diseases;
- the formation of thrombosis;
- dyspeptic disorders;
- impaired renal function.
Hematopoietic progenitor and stem cells in the treatment of multiple sclerosis:
Risk of complications and rejection
When a patient’s own stem cells are introduced into the patient’s body—autologous transplantation—the risk that rejection will occur is extremely low. After all, the immune system will perceive them as “family.”
An exception may be people with autoimmune pathologies - for example, systemic lupus erythematosus. In this case, additional immunosuppressive medications will be required.
Complications during transplantation are possible:
- if the amount of biomaterial is incorrectly selected;
- proper sterility was not observed during the procedure;
- the body was not previously prepared - a high concentration of already damaged immune cells in the bloodstream;
- the interval between the stages of introducing stem cells is not maintained.
However, the highest risk occurs if the patient receives stem cells from another person . Even death is possible. Therefore, many medical centers do not practice such stem cell transplantation at any stage of multiple sclerosis.
Mesenchymal cell transfer technique
Mesenchymal cells are a population of cellular structures that can be isolated from various tissues of the body.
These cellular structures have greater plasticity than, for example, hematopoietic ones, and are capable of differentiating cells such as neurons.
The introduction of mesenchymal cells provides immunomodulatory and neuroprotective effects. Similar to transplantation of hematopoietic structures, this procedure can be either auto- or allologous.
Indications and contraindications, as well as possible adverse effects, are similar to those for transplantation of hematopoietic stem cell structures.
Mesenchymal stem cells are collected from the bone marrow by puncturing the sternum or iliac crest on both sides.
The resulting cell culture is processed using a separator. After this, the cells are cultured and the necessary tests are performed. The technique has not yet found such wide application as transplantation of bone marrow hematopoietic stem cell cultures.