Brain tumors are neoplasms localized inside the skull, which are characterized by tumor damage to nerves, membranes, cerebral tissues, blood vessels and the endocrine system of the brain. Their differences from other species lie in the location - they are located in a limited intracranial space, which is why their presence inside the skull leads to many negative consequences.
Indications and contraindications for surgery
A brain tumor can be benign or malignant. Not every brain tumor is an indication for instrumental intervention. The feasibility of the operation is decided by a medical council.
After comparing the risk and the chances of a favorable outcome, a planned operation to remove the intracranial formation is prescribed, or conservative therapy is individually selected.
Indications for surgical removal of the tumor:
- Rapidly progressing pathology (rapid tumor growth);
- Impaired brain functionality (complete or partial);
- Tumor pressure on vital centers in the brain;
- Easily accessible localization;
- No concomitant diseases.
Benign tumors are not always removed surgically. If the pathology does not develop and does not disrupt the activity of brain structures, then a waiting tactic and a conservative approach are chosen.
The growth of a benign brain tumor leads to tissue compression and an increase in pathological symptoms. The neoplasm has clear contours, metastasis does not occur, which makes it possible to completely excise the lesion without affecting healthy tissue.
Contraindications for surgery:
- Infectious diseases;
- Very old age;
- Exhaustion of the body;
- Metastasis process;
- Hard to reach localization;
- Multiple lesions;
- Partial excision will not affect the duration or quality of life;
- High risk of death;
- High risk of relapse.
Malignant tissue damage in the brain in the final stages is also a contraindication for surgery. Abnormal cells rapidly attack healthy tissues and spread through the blood to other organs and systems.
What to do to get treatment quickly?
Collect as much information as possible
Having suspected oncology after the ultrasound, I began to call oncologists whose contacts I had and consult. During treatment, I listened to about 20 different opinions on how to act and what to do.
I am a nuclear physicist by training, but my career is related to oncology: I worked on the creation of radioisotopes used in tomography. Therefore, I understood what oncology is, what keywords and sources of information there are in this topic.
The Higher School of Oncology also helped a lot - I gave lectures on oncogenetics there and met many specialists. Then Facebook came to the rescue: my primary network of contacts pulled the secondary one and helped us find people with whom we knew through one handshake.
If possible, do not wait for examinations
Having received recommendations from oncologists, we did not wait for state quotas for special studies. They are not that expensive: in total we spent about 100 thousand rubles on treatment.
When we found out the diagnosis, my father went to the district clinic, where he was given a referral to the oncology clinic for January and was prescribed a chest x-ray, which in his case was completely uninformative. If we had gone down this path, the situation would have been much worse: you are constantly faced with some kind of delays and commissions.
Anton Barchuk Researcher, National Medical Research Center of Oncology named after. N.N. Petrova, expert at the Cancer Prevention Foundation
In the case of examinations, there is no single solution - there is always a choice, an alternative. But if a person decides to undergo treatment somewhere, then it is better to check in the very place where he should undergo additional examination, so as not to do something twice.
If a person plans to be treated at a regional oncology clinic, then in this case it is logical to undergo an examination there or in the place where the oncologist, whom this person trusts, advises.
Interact directly with the cancer center
When the exact diagnosis is known, getting a quota for surgery is not so difficult. If you receive a quota from the bottom up - from the district clinic to the district oncology clinic, then to the city one - treatment can be very delayed. If you go directly to a center specializing in a specific type of cancer, then decisions on issuing quotas are made faster, because it is in their interests to use all the allocated limits by the end of the year.
According to the state quota, we performed an operation and the most expensive study - positron emission tomography.
Coordinate the patient's loved ones
It was very important that within the family no one hid or hid anything; we openly discussed the chances and diagnoses.
All family members participated in my father’s treatment—not only emotionally, but also organizationally. I talked with doctors, my sister called and signed my father up for tests. As a result, the doctors with whom we spoke also made contact: they found out the results earlier than they should have according to the regulations. That is, it was possible to communicate sincerely and adequately, many experts suggested something useful.
Types of surgery
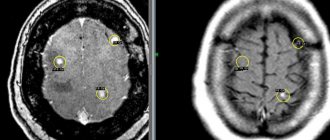
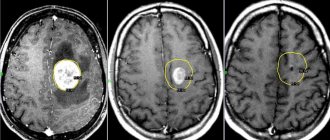
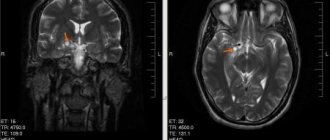
Before surgical intervention, a diagnosis is carried out, on which the choice of the type of excision of the pathological focus largely depends. A study using visualization of the tumor on an image or displaying the image on a computer allows doctors to determine the type of pathology and size.
Types of surgical techniques for removing the lesion:
- Stereotactic radiosurgery – the tumor is removed using high-precision radiation. Radiation therapy is performed without invasive intervention;
- Trepanation of the cranium - access to the lesion is provided through the created hole, after which the tumor is removed;
- Endoscopy is a type of trepanation, but less traumatic. Access to the lesion occurs through a puncture. The progress of the operation is visualized on a computer.
More often, neurosurgeons resort to one of the types of craniotomy. Full access to the pathological focus is provided and it is possible to remove the affected bone part of the skull.
Treatment of brain tumors
Modern oncology has three main methods of treating intracranial tumors:
- surgical intervention;
- radiosurgery and radiation therapy;
- chemotherapy method.
A radical way to get rid of a tumor is brain surgery. Methods such as chemotherapy and radiation therapy are concomitant effects on the site of pathology before or after surgical treatment.
Radiosurgery is a method of radiation therapy that allows you to cope with a tumor without surgery. Advanced equipment such as cyberknife and gamma knife are used to perform radiosurgery.
Preparing the patient
The preparatory stage before removal of the tumor is aimed at reducing the risk of complications during and after the operation.
Standard preparation for surgery:
- Laboratory diagnostics;
- Registration and examination of the heart (ECG);
- CT or MRI of the brain;
- Angiography of cerebral vessels.
If the examination results are satisfactory, decongestant therapy begins. If there is a history of epileptic seizures, then anticonvulsants are prescribed.
Recommendations a few days before surgery:
- Consumption of alcoholic beverages is prohibited;
- Avoid smoking;
- Observe prophylactic anticoagulants.
The day before surgery, the gastrointestinal tract is cleansed and food or liquid intake is stopped.
Progress of the operation
Radical treatment is carried out only with the use of anesthesia. After gaining access to the pathological focus in the brain, the neurosurgeon performs complete or partial excision of the tumor. The affected area of the organ is not removed if this could lead to severe neurological disorders.
The operation is carried out under visual control, which is provided by equipment (ultrasound, MRI or CT). It is possible to remove a tumor in the brain with a scalpel or using a laser beam.
Laser tumor excision is a less traumatic method and reduces the risk of bleeding to a minimum. Laser exposure leads to intense heat generation and excision of soft tissue, without damaging bone. Rays are effectively used for difficult-to-reach tumors in brain structures.
After surgery, radiotherapy is prescribed to prevent secondary formations. Radiation therapy can be used for inoperable cases or partial removal of a pathological focus in the brain. Exposure to radiation is used mainly during the malignant course of the process, in order to stop the division of atypical cells.
Anesthesia
Instrumental intervention is often performed under general anesthesia. Medication-induced sleep is achieved by inhaling nitrous oxide, which is passed through an endotracheal tube into the lungs. The patient is unconscious and as relaxed as possible, the equipment monitors cardiac activity. A ventilator (artificial lung ventilation) supports breathing.
In some cases, the patient is conscious during the operation - this depends on the location of the lesion. The use of local anesthesia is necessary to assess the functionality of vital centers (speech, thinking, vision). This measure allows for the most effective surgical intervention and avoids undesirable consequences.
Stereotactic treatment methods do not always require anesthesia, since there is no tissue trauma to access the lesion. Local anesthesia may be used.
Craniotomy open surgery
During surgery, access to the intracranial formation is obtained by removing a section of bone and periosteum. The neoplasm is excised, the vessels that supplied blood to the formation are sealed (anticoagulation). In most cases, the bone tissue lesion is also excised, and a prosthesis is inserted, which is modeled in advance.
After successful removal of a tumor in the brain, a bone flap is placed over the hole, and fixation is carried out using metal plates or screws.
Endoscopy
A small puncture is made in the skull and an endoscope is placed into the hole. The device is equipped with a mini-camera and various attachments.
All actions are monitored on the monitor, after excision of the tumor in the brain structures, it is removed through the access obtained.
Stereosurgery
The treatment method is not invasive. Atypical cells deep in the brain are exposed to a stream of radioactive rays. The method relates more to conservative therapy, since it does not cause trauma to the tissues of the skull. A device in the form of a helmet is placed on the patient’s head, after which the pathological focus is exposed.
The radioactive beam has a specific wavelength that destroys the pathological focus without affecting healthy tissue. The patient is conscious and does not experience pain.
The method is used to destroy small intracranial formations (up to 3 - 3.5 cm).
Cyber knife system
Radiation beams focused precisely on the lesion are used to remove the tumor. Under visual control (using equipment), the cyber knife is positioned at certain coordinates on the skull, after which the stream of rays is turned on at different angles.
Gamma knife
The procedure is similar to the cyber knife system. A tumor in the brain is exposed to concentrated beams of radioactivity. The patient must be in a motionless position at the time of exposure; a frame is placed on the area of the skull.
The procedure is performed after local anesthesia.
What is a benign tumor?
A tumor is a pathological formation that is formed as a result of differentiation and uncontrolled cell division. Successive mutations lead to neoplastic (tumor) transformation of cells. As a result, healthy tissues lose their specific structure, but more often retain their functions completely or partially. The process of tumor growth can be accompanied by damage to surrounding healthy tissues - the tumor compresses them, disrupting blood circulation, nutrition, regeneration and other natural processes.
Types of benign tumors
Tumor is the general name for many neoplasms that grow from various tissues of the body. For example, according to the type of fabric, the following types are distinguished:
- Flat and columnar epithelium - Epithelioma;
- Glandular epithelium - Adenoma;
- Connective tissue - Fibroma;
- Adipose tissue - Lipoma;
- Smooth muscle tissue - Leiomyoma;
- Bone tissue - Osteoma;
- Cartilage tissue - Chondroma;
- Lymphoid tissue - Lymphoma;
- Striated muscle tissue - Rhabdomyoma;
- Nervous tissue - Neuroma.
Recovery after surgery
Rehabilitation after removal of a brain tumor is quite long and includes an integrated approach. Recovery after tumor removal takes place in several stages:
- In a hospital setting – adaptation, learning lost skills. Condition monitoring, prevention of postoperative complications, passive loads with transition to exercise therapy.
- On an outpatient basis (at home) – taking prescribed medications, physiotherapy and massage. Gradual physical activity (swimming pool, walking).
Rehabilitation occurs within a year. If the recommendations are followed, lost functions are completely restored.
The patient must follow a diet throughout the entire period and avoid drinking alcohol.
Recommendations during the recovery period:
- Avoid heavy physical activity for a year;
- Avoid climate change and high changes in atmospheric pressure (flights) for three months;
- Avoid prolonged exposure to ultraviolet rays (tanning);
- Do not visit the bathhouse or sauna.
The recovery period depends on the type of surgery and may take a shorter period of time.
Classification of the disease
In addition to dividing into benign and malignant, there is a classification into primary and secondary tumors - in the second case, they arise as a result of the spread of malignant processes from other organs.
For treatment, it is important to know in which cells and tissues the neoplasm occurs. Common primary tumors include the following:
- developed directly from brain tissue;
- meningiomas - tumors of the membranes;
- Neuromas are formations in the nerves of the skull;
- pituitary adenoma.
Based on their location, neoplasms can be located in the upper or lower sections, hemispheres, midline structures, or base of the brain.
Prognosis after removal
Life expectancy depends on the type of intracranial formation and the location of the lesion. Timely seeking medical help for pathological symptoms allows you to diagnose tumors at the initial stage and carry out radical treatment.
Removal of a brain tumor with a benign course guarantees a complete cure and has a low risk of disease recurrence. Removal of malignant tumors has a high probability of recurrence within 5 years after radical treatment.
How long they live after neurosurgery depends on the stage of cancer and the age of the patient. The older you get, the lower the body’s compensatory capabilities and immune resistance to atypical cells become.
Detection of a tumor at an early stage has a high percentage of complete cure. Late diagnosis and the presence of metastases are not subject to instrumental intervention and inevitably lead to death.
Severe consequences after surgical removal of a brain tumor with the correct medical tactics are low. Even incomplete removal of the tumor prolongs the patient’s life and improves the quality of life. Refusal to undergo surgery leads to inevitable death.
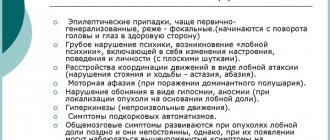
Clinical picture
The totality of manifestations of the disease depends on the location and size of the lesion. It consists of general cerebral and focal symptoms.
General cerebral symptoms
Any of the processes listed below is a consequence of compression of brain structures by a tumor and increased intracranial pressure.
- Dizziness may be accompanied by horizontal nystagmus.
- Headache: intense, constant, not relieved by analgesics. Appears due to increased intracranial pressure.
- Nausea and vomiting, which do not bring relief to the patient, are also a consequence of increased intracranial pressure.
Focal symptoms
It is diverse and depends on the location of the tumor.
Motor disorders are manifested by the appearance of paralysis and paresis up to plegia. Depending on the lesion, either spastic or flaccid paralysis occurs.
Coordination disorders are characteristic of changes in the cerebellum.
Sensory disorders are manifested by a decrease or loss of pain and tactile sensitivity, as well as a change in the perception of the position of one’s own body in space.
Violation of oral and written speech. When the tumor is localized in the area of the brain responsible for speech, the patient’s symptoms gradually increase; those around the patient notice changes in handwriting and speech, which become slurred. Over time, speech becomes slurred, and when writing, only scribbles appear.
Visual and hearing impairment. When the optic nerve is damaged, the patient's visual acuity and ability to recognize text and objects changes. When the auditory nerve is involved in the pathological process, the patient's hearing acuity decreases, and when a certain part of the brain responsible for speech recognition is damaged, the ability to understand words is lost.
Convulsive syndrome. Episyndrome often accompanies brain tumors. This is due to the fact that the neoplasm compresses the structures of the brain, being a constant irritant of the cortex. This is precisely what provokes the development of convulsive syndrome. Convulsions can be tonic, clonic and clonic-tonic. This manifestation of the disease is more common in young patients.
Autonomic disorders are expressed by weakness, fatigue, instability of blood pressure and pulse.
Psycho-emotional instability is manifested by impaired attention and memory. Often, patients' character changes, they become irritable and impulsive.
Hormonal dysfunction appears during a neoplastic process in the hypothalamus and pituitary gland.