What is hypersomnia?
People with hypersomnia do not feel rested when waking up, even after a long sleep. They may have an overwhelming urge to sleep at any time, including at work or while eating. People with a disorder called idiopathic hypersomnia typically sleep more than 11 hours a night and have difficulty waking up. This type of behavior often has a significant impact on social, family and work life. Depending on the type of hypersomnia, it may first appear in adolescence and early adulthood and may require lifelong treatment. Hypersomnia can be either primary or secondary.
Primary hypersomnia
is a condition that affects the central nervous system and directly affects sleep itself. Examples are narcolepsy, idiopathic hypersomnia, and Kleine-Levin syndrome.
Secondary hypersomnia
is a condition in which excessive sleepiness is caused by another condition or disease. Examples include:
- lack of sleep
- a sleep disorder that fragments sleep, such as sleep apnea
- head injury or other neurological disorder such as Parkinson's disease
- medical disorder
- certain medications, including opiates, benzodiazepines, antipsychotics, and antihistamines
Etiology
Factors in the occurrence of this disease can be both internal circumstances and external causes. Thus, hypersomnia manifests itself when:
- prolonged or persistent lack of sleep caused by stress or other conditions;
- severe physical fatigue;
- emotional exhaustion;
- taking certain medications, the side effects of which lead to disturbances in sleep and wakefulness;
- substance abuse;
- injuries and bruises of the skull;
- concussion;
- the occurrence of a malignant neoplasm in the brain in the form of hematomas, oncology or cysts;
- acute infectious diseases;
- lack of oxygen in brain tissue;
- breathing disorders during sleep, for example, with apnea, which is characterized by periodic lack of breathing during sleep;
- mental disorders, including schizophrenia;
- diabetes mellitus;
- dysfunction or complete absence of the thyroid gland;
- heart or kidney failure;
- liver cirrhosis;
- narcolepsy - attacks of falling asleep last from ten to thirty minutes;
- prolonged exposure to stressful situations;
- lifestyle change.
Sleep apnea
Diagnosis of hypersomnia
Patients must continue to have symptoms of hypersomnia for 3 months before doctors can diagnose primary hypersomnia. As part of the diagnosis, doctors will use a multiple sleep latency test. This test measures how quickly a person falls asleep in a quiet environment during the day.
Diagnosing the cause of secondary hypersomnia may involve reviewing medications the patient is taking and ruling out other health conditions or sleep disorders that may cause fatigue. The doctor will also ask the person about their sleep habits.
Diagnostics
The diagnosis is made based on the patient's story and medical history. A comprehensive examination is carried out to identify the form and etiology of the pathology. A neurologist performs special testing. Hypersomnia is diagnosed using the Sleep Latency Test (MSLT) and the Epworth Sleepiness Scale. Basic instrumental methods:
- Polysomnography (study of sleep patterns and disorders).
- Electroencephalography, echoencephalography (study of bioelectrical activity of the brain).
- MRI, CT (study of the state of the brain matter). The study is carried out if there is a suspicion of the presence of primary pathologies (tumors or contusions of the brain, pathologies of elements of the cerebral circulatory system) that provoked hypersomnia.
- Ophthalmoscopy (examination of the fundus of the eye).
To diagnose hypersomnia, generally accepted methods are used, such as polysomnography at night, which is necessary to exclude obstructive sleep apnea or a syndrome manifested by restless legs. Studying the medical history allows us to determine the causes of disorders.
The doctor takes into account the presence of a history of TBI and genetic diseases. According to indications, consultations with a psychiatrist, ophthalmologist, neurosurgeon, and cardiologist are necessary. Differential diagnosis is carried out in relation to conditions that develop due to chronic fatigue, asthenic syndrome, and depression.
Treatment of hypersomnia
Treatment for hypersomnia will depend on associated symptoms and the type of hypersomnia. The treatment plan may include behavioral therapy, medication, or both.
Behavioral therapy
A doctor may refer a patient with hypersomnia to cognitive behavioral therapy (CBT). The goal of therapy is to improve the quality and quantity of sleep and reduce thoughts that interfere with normal sleep patterns. Your doctor may also recommend lifestyle changes, such as avoiding night work and staying away from socializing late at night. It remains unclear whether behavioral treatments are effective for treating hypersomnia.
Medicines
People with primary hypersomnia often use stimulants to prevent excessive sleepiness. This could be a
Amphetamine (Evekeo) or methylphenidate (Ritalin). Other options are non-stimulants that promote wakefulness, such as Modafinil (Provigil).
Your doctor may prescribe treatments for other conditions, such as antidepressants for those who suffer from depression. Sodium oxybate (Xyrem) is another option to reduce daytime sleepiness in patients with narcolepsy. The type of drug the doctor recommends will depend on what medications the person is already taking.
Treatment options
Treatment of idiopathic hypersomnolence is selected individually, since it manifests itself differently in everyone and is provoked by various factors. Doctors try to identify all disorders in the body that could lead to such a sleep disorder. Therefore, you will have to undergo a comprehensive medical examination in order to somehow understand them.
To help the patient, medications such as Dextroamphetamine, Propranolol, Mazindol, etc. are often prescribed. They can relieve drowsiness for a while, but are not a panacea. Under no circumstances should you prescribe or use them yourself!
Some patients benefit greatly from physiotherapeutic procedures: electrosleep, pressure chamber, etc. Muscle and nervous tension can be relieved with the help of physical therapy and massage. Sometimes hypnosis sessions are used if the patient has experienced severe stress or mental trauma.
During treatment, doctors usually advise avoiding heavy mental stress, intense sports training, and driving. It is not recommended to plan moves, weddings, job changes and other major life changes. A change of scenery can be beneficial, but without long journeys and especially flights.
Forecast
The prognosis may depend on the cause of hypersomnia. Primary hypersomnia is treatable, but the condition can last a lifetime and have serious consequences. For example, a patient may refuse to drive if there is a risk that he may fall asleep while driving.
Patients with secondary hypersomnia may receive various forms of treatment for other conditions. When a doctor successfully treats the underlying condition, symptoms of hypersomnia may disappear.
Feeling tired or drowsy during the day is not always a cause for concern. Some people will experience sleepiness due to disrupted sleep patterns or staying up too late. However, those who regularly experience excessive sleepiness for no clear reason should consult a doctor. This consultation is especially important if symptoms interfere with social, work and family life.
Symptoms of the disease
Idiopathic hypersomnia differs from other diseases in which sleep disturbance occurs in that the patient quickly falls asleep and sleeps for 8-10 hours. If possible, a person can lie down to rest during the daytime.
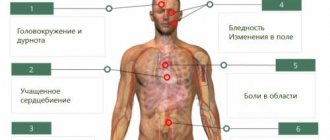
However, a lot of sleep in this case does not cause refreshment and relief: it is difficult for a person to wake up and get out of bed, and during wakefulness he is accompanied by unpleasant symptoms, such as:
- severe fatigue;
- loss of orientation soon after waking up;
- the appearance of apnea during sleep, which is characterized by a temporary cessation of breathing (this causes lethargy and lethargy);
- nervous state of the patient;
- development of hypertension (high blood pressure);
- decreased performance;
- absent-mindedness;
- weakness;
- deterioration in the quality of vision;
- too much sleep (day and night), which is difficult to reduce;
- drowsiness during the day;
- general deterioration in health, which will be bad almost always;
- inability to concentrate on anything for a long time.
If the disease is severe, this can lead to the person at some point beginning to “switch off.” This condition poses a serious threat to life.
Doctors' recommendation: if you identify one or more symptoms characterizing the disease, you need to immediately consult a doctor, otherwise the consequences can be disastrous.
Patients with idiopathic hypersomnia can set a record for the time they sleep and fall asleep. For example, if a healthy person takes 15-20 minutes to fall asleep, then a hypersomniac can do it in just 3-5 minutes.
The sleep record for a person with hypersomnia is 46 hours. And the record for the shortest wakefulness is 15 minutes. However, unfortunately, such records are not worth being proud of.
Diagnostic measures for studying hypersomnia
Since, during the course of the disease described, people are not always able to correctly assess the troubles they have, then to study the disease, doctors resort to the following generally accepted tests:
Stanford scale.- Latency analysis.
- Polysomnographic scanning - capable of detecting a shortened amount of sleep, frequent awakenings at night and the early formation of the REM sleep phase, taking into account the fact that stable REM sleep begins 80 minutes after switching off.
In order to exclude organic pathologies, experts prescribe the following procedures:
- Consultation with an ophthalmologist.
- Carrying out ophthalmoscopy.
- A neurological analysis is prescribed.
- Study of body readings using Echo-EC.
- MRI scanning and computed tomography.
- If somatic problems are identified, it is necessary to visit the offices of a therapist, an expert in endocrinology, a cardiologist, a doctor specializing in gastroenterological research, and a nephrologist.
A conclusion about the presence of hypersomnia can only be made by a neurologist if the symptoms of the disease do not go away within 31 days and are in no way related to lack of sleep for any reason or to the use of pharmacological drugs.
Treatment Options
Successful elimination of the presented deviation is quite closely related to effective therapy of the underlying disease state, since hypersomnia is one of its symptoms. If the main source of the problem cannot be cured in any way, then doctors prescribe all methods to improve the patient’s comfortable life. To do this, you must follow the following instructions from specialists:
The main rule is to stick to your sleep schedule.- a person with such complaints needs to find a suitable workplace so that the operating hours are only during the daytime.
- In addition, you will need to maintain the same bedtime and necessarily add a couple of hours of daytime rest to your daily lifestyle.
- The night period of inactivity should not exceed 9 hours.
- If the patient has an idiopathic form, then rest during the day should not exceed 45 minutes.
- Absolute avoidance of alcoholic beverages and heavy foods.
- The last meal should not be taken before going to bed.
- Taking special medications aimed at stimulating activity.
- For catalepsy, the use of pharmaceutical drugs that have the effects of eliminating depression is prescribed.