Multiple sclerosis is characterized by slow progression.
The majority of patients are people with relapsing-remitting MS. It is typically characterized by alternating periods of exacerbation and subsidence of symptoms with partial/complete recovery.
Secondary progressive multiple sclerosis is diagnosed in approximately 80% of patients with a similar pattern of pathological development. The person's condition slowly deteriorates, although periods of exacerbation are either very rare or completely absent.
Secondary progressive multiple sclerosis is a rather difficult condition to diagnose, since specialized techniques to distinguish between primary progressive and secondary MS do not exist. The transition is determined by doctors based on clinical observations of the patient’s condition.
Classification
Manifestations of the disease are very individual. Therefore, the generally accepted classification is based on the nature of the pathological process.
The following types of sclerosis are distinguished:
- Remitting. The most common type of multiple sclerosis. It affects approximately 80% of all patients. It is characterized by the presence of clearly defined exacerbations and remissions.
- Secondary progressive. Develops after remitting. On average, the transition to this form takes about 10 years. Characterized by short periods of remission, the disease gradually becomes chronic.
- Primary progressive - characterized by gradual but steady development. Every day the disease progresses, the health of patients becomes worse. Exacerbations are absent or occur very rarely. This form affects every tenth patient.
- Progressive-relapsing is the least common type and combines the features of primary progressive and remitting.
The disease is most easily treated in a remitting form. The main goal of therapy is to avoid further development of the disease.
What therapy is used?
20 years ago, drugs appeared that changed the course of multiple sclerosis—DMTs—which radically changed the prognosis of the disease. Now, with the correct selection of therapy, the life of patients with MS does not differ from the lives of other people, either in quality or in duration. They give birth, travel, set sports records, etc.
Question answer
What is the life expectancy of people with multiple sclerosis? However, simply writing a prescription for MS is not enough. There are no standard treatments for multiple sclerosis. The disease progresses differently for everyone, and the medicine only works if it accurately hits the pathological process that occurs in the body.
The correct selection of therapy is also important because the more effective the drug, the more side effects it has. If medications are prescribed without indications, serious consequences are possible (infections, somatic problems, etc.). Each drug has its own “risk management plan.” If it is performed, the likelihood of side effects is minimal.
In our country, more than 60 thousand patients receive these expensive medications free of charge.
Causes and risk factors
Multiple sclerosis has several causes and many risk factors. Difficulties with treatment and prevention are largely due to the fact that it is not always possible to establish a specific cause. At the moment, multiple sclerosis is considered a polyetiological disease.
The following risk factors for the development of sclerosis are identified:
- Infectious diseases - as a rule, the disease is provoked by a combination of several infectious chronic diseases.
- The presence of a genetic predisposition - the hereditary factor is considered the most important.
- Presence of injuries.
- Prolonged stress, psychological and mental dysfunction.
- Environmental factors – environmental, territorial, economic. Multiple sclerosis is more common in cool climates in developed countries. Lower incidence in countries located on the equator.
To date, doctors have been able to identify specific provoking biological, environmental and chemical causes:
- Chronic lack of sunlight, resulting in a lack of vitamin D.
- Lack of iodine, manganese and zinc. In some regions they are obtained from soil and water - the necessary microelements are contained in locally produced products. In regions with insufficient amounts of these substances, it is necessary to further fortify products.
- Features of nutrition and lifestyle - poor ecology due to urbanization, the predominance of animal fats in the daily diet.
- Exposure to radiation.
Symptoms and manifestations
The development of the disease can be slow or rapid - it depends on the form. In the case of the second option, the patient has a better chance of seeking help in a timely manner. If sclerosis progresses slowly, patients do not pay attention to the deterioration of their health for a long time.
The most characteristic symptoms of multiple sclerosis:
- Increased fatigue, loss of muscle strength. As the disease progresses, paresis appears. As a rule, symptoms are more pronounced in the lower extremities. Neurological examination revealed reflex disturbances. Dystonia, hypotension.
- Loss of coordination. It manifests itself individually - one person experiences dizziness, handwriting becomes worse, and hand tremors appear. Some people have problems with gait. As the disease progresses, the symptoms intensify and motor function is severely impaired.
- Speech disturbances arise with the development of the disease - at first, chanting of speech is clearly manifested.
- Optic nerve disorders – double vision, nystagmus, strabismus. Disorders of the trigeminal and facial nerves may be observed.
- Loss of sensation is a symptom that, along with motor dysfunction, strongly suggests multiple sclerosis. Parts of the face and limbs go numb. There may be tingling sensations in the muscles.
- Frequent or infrequent urination, frequent or decreased urge to defecate.
- Impotence, decreased libido.
- Changes in the intellectual sphere - decreased memory, concentration, ability to analyze. The patient quickly gets tired when solving intellectual problems and has difficulty switching.
- Psychological disorders – depression, anxiety, nervousness, euphoria.
Symptoms may manifest differently, depending on where the plaques are located in the central nervous system. If you observe several of the listed factors in yourself and or in one of your loved ones, be sure to consult with an experienced neurologist!
Diagnostics and examination
CT scan of the brain
- Cost: 6,000 rub.
More details
Modern medicine makes it possible to reliably diagnose this disease. Usually one examination is enough for this. The remaining appointments are needed to assess the course of the disease, to monitor the effectiveness of therapy, and to obtain additional data on the course of the pathological process.
In the treatment of this disease, early diagnosis is extremely important and even critical - it is much more amenable to correction in the early stages.
Diagnosis begins with a neurological examination and medical history. If the disease is advanced, the doctor also interviews the patient’s relatives to get a correct picture of the disease.
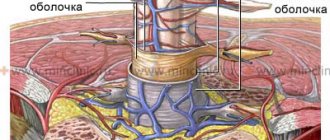
In addition, MRI of both the brain and spinal cord is prescribed to determine the presence and location of demyelinated lesions. Evoked potential studies are used in the later stages of the disease to assess the degree of damage to the central nervous system. The most commonly used laboratory test is cerebrospinal fluid. Deviations from the norm are one of the criteria for multiple sclerosis (but not decisive).
Multiple sclerosis (MS) is a widespread, chronic demyelinating disease of the central nervous system (CNS), affecting mainly young people, although childhood forms of this disease are also found, as well as its late onset. It is now known that in parallel with autoimmune inflammation in MS, neurodegenerative processes also occur, which begin to prevail over time. This leads to the accumulation of irreversible neurological deficits and, as a consequence, disability of patients.
In 1996, the International Classification of MS was approved, which was based on the types of its course [1]. Relapsing-remitting MS (RRMS) and chronic progressive forms were distinguished - primary progressive MS (PPMS), secondary progressive MS (SPMS), and relapsing-remitting progressive MS. SPMS usually results from transition from MS after 10–15 years of disease progression. But in some patients, immediately after the first clinical episode, there is a slow increase in neurological deficit without episodes of remission, which indicates a possible primary progressive type of disease (PPMS). As was evident from the above, PPMS itself was also divided into PPMS without exacerbations and with exacerbations (remitting-progressive MS).
Epidemiology and genetics of PPMS
The incidence of PPMS, according to various literature data, ranges from 7.9 to 21.7% of the total population of MS patients [2, 3]. At the onset of PPMS, patients are on average 10 years older than patients with RRMS; the average age of onset ranges between 37.3 and 42.7 years [3]. There is also an equal frequency of debuts in women and men and their rarity in childhood.
In 2005, the results of observation of the natural course of MS in 2837 patients conducted in the UK, Colombia and Canada were published [4]. In 12.4% of cases (352 patients), PPMS was diagnosed with an average age of onset of 40 years, with an almost equal ratio of men and women and an average disease duration of 17 years; in 75% of cases, after 7-8 years of the disease, a pronounced neurological deficit with EDSS=6.0 points was noted.
A comparative study of 1844 patients with PPMS and SPMS was conducted by French researchers [5]. During the study, it was revealed that the age of patients at the time of transition from RMS to SPMS is on average 40 years, and the onset of PPMS on average is 40 years. Despite the clinical differences in individual groups of patients, there was a similarity in the rate of disease progression and an increase in neurological deficit mainly due to damage in one functional system.
When studying the genetic aspects of the occurrence of PPMS, it was found that both PPMS and RRMS can occur in identical twins. Immunogenetic studies have shown that the risk of developing one or another type of MS is associated with the major histocompatibility complex class 2, namely the DR2 haplotype DRB1*1501 of the major histocompatibility complex class 2 on chromosome 6 [6–8]. A more detailed study of the genetic markers of PPMS revealed [9] that there is a violation of the expression of the T-cell proliferation gene (IL7R) in patients with PPMS.
Some features of the pathogenesis of PPMS
One review of studies on the natural history of MS [10] revealed that the rate and pattern of progression in PPMS and SPMS are similar, based on which it was suggested that the leading mechanism in the pathogenesis of PPMS may be axonal degeneration leading to neurological deficits. In connection with this, neuromorphological studies began to attract great attention.
A group of researchers led by T. Revesz [11] conducted a histological study of the demyelination focus of a patient with PPMS, during which a significantly lower content of inflammatory cells was revealed in comparison with the demyelination focus of a patient with SPMS. These data, combined with a previous MRI study, showed that PPMS has less focal white matter involvement.
Demyelination lesions in PPMS showed [12, 13] loss of oligodendrocytes and less severe axonal damage than lesions in RRMS [14]. Some researchers [15] drew attention to the fact that in the externally unchanged white matter of patients with both PPMS and SPMS, pronounced demyelination and diffuse changes with activation of microglia and axonal damage are observed, which once again indicates the similarity of the processes occurring in the brain tissue with these types of MS. Signs of demyelination were also noted in the cortical gray matter, although more significant changes were seen in the white matter, especially in MS patients, with a clear delineation of affected and unaffected areas.
Summarizing the above, there are clear differences between RRMS and PPMS: with PPMS, more pronounced pathological changes are noted in the form of diffuse axonal damage in the white matter and cortical demyelination, in contrast to RRMS, we are talking about local tissue damage in the focus of demyelination.
There is now sufficient convincing evidence to support the assumption that axonal loss underlies the irreversible and progressive nature of disability in MS. in vivo biomarkers of axonal injury.
.
The most widely used marker of axonal degeneration is the detection of increased concentrations of amyloid protein in axons in areas of demyelination. Another immunohistochemical marker of axonal damage is SMI32, an antibody that labels nonphosphorylated axonal neurofilaments. Normally, maturation of the axonal cytoskeleton is usually accompanied by an increase in phosphorylated neurofilaments. This process is induced by glial cells during myelination and leads to an increase in axon diameter. During the process of demyelination, axonal neurofilaments are dephosphorylated, resulting in structural changes within the axon itself. Other changes in the axon cytoskeleton are also noted - phosphorylation and release of the Tau protein, which is the main protein of axonal microtubules. It is the increase in the concentration of this protein that is detected in the cerebrospinal fluid of patients at the onset of the disease, both with RMS and with progressive forms [16]. All this indicates that the axon cytoskeleton is very vulnerable, and functional disorders over time, with chronic exposure to destructive factors, turn into structural lesions with disruption of synaptic transmission of nerve impulses.
To the above, we can add that in RRMS and PPMS, antibodies to myelin were detected in the serum and cerebrospinal fluid. This became the basis for the statement [17] that PPMS is a disease with antibody-mediated pathogenesis mechanisms.
To objectify atrophic processes in the central nervous system as a manifestation of neurodegeneration, MRI is currently widely used. Atrophic processes in patients with PPMS and SPMS using MRI are detected both in the brain and in the spinal cord already at the initial stages of the disease, and a connection between atrophic processes and the increase in disability of patients has been established.
The use of another new method, MR spectroscopy, and analysis of changes in the content of N-acetylaspartate (NAA) made it possible to detect neuronal loss in MS even in the apparently unchanged white and gray matter of the brain. One possible explanation for neuronal loss may be secondary Wallerian degeneration as a consequence of focal axonal damage.
The data obtained from studying the blood-brain barrier (BBB) in MS patients deserve special attention. In 2007, the results of a study of the state of the BBB in patients with PPMS and SPMS were published [18]. Signs of BBB failure were identified not only in active lesions, but also in chronic inactive lesions, as well as in externally unchanged white and cortical gray matter of the brain in both PPMS and SPMS.
MRI criteria for diagnosing PPMS
In all diagnostic systems, PPMS is identified as a separate form of MS. Due to the fact that there was previously no evidence that the neuroimaging characteristics of patients with relapsing-remitting forms of MS are significantly different from those of patients with PPMS, the MAGNIMS expert group concluded that the use of uniform criteria will significantly facilitate the diagnostic evaluation of patients with PPMS [19]. In 2009, MRI criteria characterizing the dissemination of the pathological process in space and time were proposed for the diagnosis of both PPMS and RRMS and were more clearly stated in the form of modified McDonald criteria (2010) [20, 21]. According to these criteria, dissemination of the pathological process in space in PPMS is determined by the presence of 2 of the following 3 criteria: the presence of one lesion or more in the brain in T2 modes, in at least one of the three localizations typical for MS (periventricular, subcortical, subtentorial); the presence of two or more foci in T2 modes in the spinal cord; positive examination of the cerebrospinal fluid for oligoclonal IgG antibodies.
The sensitivity of using the spinal cord criteria and testing the cerebrospinal fluid for oligoclonal IgG antibodies was analyzed retrospectively in a cohort of 95 patients with PPMS [22]. As a result of this study, the criterion for dissemination of the pathological process in space for the spinal cord was changed from 2 foci or more to 1 foci or more (it does not matter whether these foci are clinically significant or not), which significantly simplified this criterion and increased its sensitivity ( see table, see figure). But despite this, a more detailed verification of its specificity is required.
MAGNIMS (2016) MRI criteria for PPMS
MRI of the brain and cervical spinal cord of a patient with PPMS in PD (a, c) and T2 (b, d) modes. In the periventricular white matter of both hemispheres of the cerebrum, as well as in the spinal cord at the level of the C6 vertebra, foci of demyelination are detected (indicated by arrows).
As a result, the MAGNIMS expert group came to the conclusion [19] that the criterion of dissemination of the pathological process in space should be used for both RMS and PPMS, with an additional study of the cerebrospinal fluid for oligoclonal IgG antibodies in doubtful cases.
Main clinical features, course and prognosis
One of the main differences between PPMS and RRMS (besides the age of the patient at the onset of the disease) is the period during which the corresponding symptoms develop and the nature of their development. With RMS, relapses of the disease are observed, occurring quite rapidly (from several hours to several days), with signs of increasing neurological deficit and alternating with periods of remission. In PPMS, functional impairment initially develops slowly over several months and sometimes years, and is rarely characterized by any fluctuations.
A number of studies have shown that the most common symptoms at the onset of PPMS are caused directly by damage to the spinal cord and are manifested by motor disorders [23]. The frequency of onsets with signs of spinal cord damage in PPMS averages 38.9–88.7%. Involvement of other functional systems, for example, sensory disorders, constitutes an average of 15-32.5% of cases; signs of involvement of the brainstem or cerebellar structures are even less - 10.8-16% of cases. But the most obvious difference between the onset of RRMS and PPMS is the frequency of involvement of the optic nerves (in PPMS, less than 5% of cases) [24].
Previous studies of the natural history of MS clearly demonstrate that progressive forms of MS have a less favorable prognosis compared to RRMS. However, cases of fairly long periods of stabilization have also been described in PPMS. To date, for PPMS, as for MS in general, there are 2 main negative prognostic factors: the rate at which the patient reaches an EDSS score of 3.0 from the onset of the disease and the involvement of 3 or more functional systems at the onset of the disease [25].
Problems in treating patients with PPMS
Since the late 90s of the last century, drugs have been used quite actively and successfully to modify the course of MS, making it possible to reduce the activity of the disease both clinically and according to MRI data, which, of course, leads to a slowdown in the progression of disability in patients. A clear division into the types of course of MS helps to determine the prognosis of the disease already at the stage of diagnosis, as well as to choose the most correct tactics for managing the patient, since drugs that change the course of MS are effective mainly in relapsing-remitting course. As for PPMS, for example, in 2000, data were published regarding the ineffectiveness of therapy obtained during a clinical trial of the use of the drug interferon beta-1a (at a dosage of 30 and 60 μg intramuscularly) in patients with PPMS in comparison with placebo [26 ]. Later, in 2009, a group of authors [27] published similar information regarding interferon beta-1b. Attempts have been made to use the drug glatiramer acetate in patients with PPMS: no significant differences with the placebo group were found in any of the efficacy criteria [28]. Subsequently, hopes were placed on the drug fingolimod, due to the fact that a slowdown of atrophic processes in the central nervous system was recorded when used in patients with RRMS. However, the INFORMS study [29] noted the lack of therapeutic effect of this drug in the treatment of patients with PPMS.
One of the modern and very successful trends in the treatment of patients with MS is currently the use of monoclonal antibody drugs. This concerns primarily the drug rituximab (a chimeric anti-CD20 monoclonal antibody). An attempt to use it in patients with PPMS was made as part of the OLYMPUS clinical trial [30]. It was found that in younger patients, with a shorter duration of the disease and the presence of active lesions according to MRI at the beginning of therapy, positive dynamics were observed in the form of a decrease in the severity of inflammatory reactions (it is assumed that this may be associated with B-cell depletion).
In September 2015, encouraging data were published regarding another monoclonal antibody, the drug ocrelizumab (a humanized anti-CD20 monoclonal antibody) [31]. In the ORATORIO study, ocrelizumab showed its good tolerability and high efficacy in the form of a significant reduction in the risk of progression of disability compared to placebo.
The results obtained regarding the effectiveness of monoclonal antibodies give hope to a fairly large group of patients with PPMS for changing a previously negative prognosis to a relatively positive one. But, despite the positive trends in the pathogenetic therapy of MS, it remains obvious to everyone that, as with RRMS, treatment of patients with PPMS should begin in the early stages of disease development.
There is no conflict of interest.
Treatment and prognosis
Multiple sclerosis requires complex treatment. The most important task is to slow down the progression of the disease, stop exacerbations in a timely manner and improve the patient’s quality of life. Symptomatic therapy allows you to maintain normal health and psychological well-being of the patient. Various groups of drugs, as well as physiotherapy, are used in treatment.
The prognosis depends on the course of the disease. With the benign variant (every fifth patient), exacerbations occur rarely, and during remission the condition improves significantly. Unfortunately, with a malignant course, treatment does not bring a significant effect, the condition worsens.
For competent and professional treatment of multiple sclerosis, contact the neurologists of the CELT clinic. Attention to each patient is the key to recovery.
Make an appointment through the application or by calling +7 +7 We work every day:
- Monday—Friday: 8.00—20.00
- Saturday: 8.00–18.00
- Sunday is a day off
The nearest metro and MCC stations to the clinic:
- Highway of Enthusiasts or Perovo
- Partisan
- Enthusiast Highway
Driving directions
Treatment of primary progressive multiple sclerosis
Treatment of the disease begins after determining the type of course of the disease - this allows you to make a diagnosis, determine the prognosis of the course of the disease, choose the appropriate tactics and the most effective drugs for this type of course of the disease. Monoclonal antibody preparations are used as effective therapy for the primary progressive form of multiple sclerosis (PPMS). The effectiveness of drugs in this group has been noted in young people who have suffered from multiple sclerosis for a short time. The drugs were well tolerated by patients; the researchers noted a decrease in the severity of inflammatory reactions in previously active lesions. Also, drugs in this group have shown effectiveness in reducing the risk of progression of disability in patients. Research continues and gives hope for a change in the prognosis of the disease in a positive direction; it is noted that the most pronounced effect occurs when treatment is started at an early stage of the disease. Also, for the treatment of PPMS, restorative and symptomatic treatment is used to improve the patient’s quality of life.
Yusupov Hospital is one of the best clinics for the treatment of multiple sclerosis in Moscow.