Causes of the anomaly
The causes of the pathology are caused by changes related to the production and movement of cerebrospinal fluid.
The diagnosis of encephalia in newborns is associated with infections that the pregnant woman had. For example, its cytomegalovirus variety contributes to the defective functioning of the ventricles of the fetal brain. Depending on the location of the pathology, doctors distinguish between internal, external and mixed types of the disease.
In addition to the congenital form, infants can also develop acquired hydrocephalus as a complication after meningitis, intoxication, or head injuries. Most types of this disease are a consequence of obstructed outflow of cerebrospinal fluid that accumulates in the ventricles of the brain.
Diagnosis of pathologies
Currently, there are several methods for diagnosing liquorodynamic disorders. The basis in this case is complaints and the clinical picture. In order for the doctor to make a more accurate diagnosis, it is necessary to initially talk with the patient, ask him about the complaints, the time of their appearance, duration, as well as the conditions against which they appear.
The accuracy of the diagnosis and the reduction of possible examinations are reduced after examining the patient; it is preferable to do this not during a period of calm and absence of a clinic, but at the moment of manifestation of the disease.
An examination is carried out, great attention is paid to checking nystagmus and palpation of muscles, especially the occipital muscles. After this, instrumental and laboratory diagnostic methods begin
Laboratory
The most common and economically less expensive is a general blood test. It indirectly determines the presence of an inflammatory process. This is necessary to confirm or, conversely, exclude a possible cause of the disease.
Cerebrospinal fluid examination. The method is less common and requires highly trained specialists for this manipulation. With its help, the nature of the contents contained in the cavity of the brain and spinal cord is clarified. In case of liquorodynamic disorders, an increase in protein content may be detected. A mandatory point is the complete absence of an inflammatory component.
- Ultrasonography. It allows you to evaluate not only the structures of soft tissues, but also possible mechanical causes that create a violation of the outflow of fluid.
- Angiography is a method for determining the condition of the vascular component of the body. In cases of liquorodynamic disorders, examination of the vessels of the head and neck is of great importance. With its help, you can identify even small disorders that give a clinical picture of the disease.
- Echoencephalography. This is a non-invasive way to detect pathological changes in the transmission of nerve impulses at the level of the brain substance.
- Computer or magnetic resonance imaging. These are ways to assess the state of brain structures, the volume of cavities and the sizes of component parts. Recently, the technique has become very popular due to the high accuracy of the resulting image compared to the previously common method of x-ray examination. Its significant disadvantage is high economic costs, as well as in some regions inaccessibility.
It is after a correctly developed diagnostic plan and the data obtained that the issue of selecting treatment is decided. It is useless to treat only symptoms, as this can lead to more rapid development of complications.
Causes
Liquorodynamic disorders can be congenital or acquired.
Congenital abnormalities that provoke the development of changes in the circulation of cerebrospinal fluid include the following brain anomalies:
- Arnold-Chiari malformation;
- Dandy-Walker malformation;
- primary or secondary stenosis of the cerebral aqueduct;
- agenesis of the corpus callosum;
- genetic disorders in the X chromosome;
- encephalocele;
- porencephalic cysts;
- trisomy on chromosomes 13, 18, 9.
The list of causes of acquired triggers includes the following anomalies:
- Intrauterine hypoxia leading to intracranial hemorrhage in the first 48 hours after birth.
- Brain and spinal cord injuries.
- Brain tumors and cysts that block the cerebrospinal fluid pathways.
- Infectious and parasitic diseases affecting the nervous system.
- Thrombosis of veins and sinuses.
- Choroid plexus papilomas.
During pregnancy, a screening ultrasound of the fetus is performed at 18-20 weeks. During this period, it is already possible to examine the brain and liquor system of the unborn child. This makes it possible to draw a conclusion about the presence or absence of brain pathology in the fetus.
Symptoms and signs of hydrocephalus
There are external, internal and mixed types of dropsy. Moreover, the latter is considered the most dangerous. Mixed hydrocephalus involves a reduction in the brain, in which fluid accumulates both in the ventricular and subarachnoid spaces. If it is moderate, then the patient has practically no complaints and can live with it for a very long time. In more serious cases, the manifestations of hydroencephalopathy in adults are as follows:
- Headache. It hardly goes away, but in the morning it is stronger than in other periods.
- Nausea. Like a headache, it is especially acute in the morning.
- Drowsiness. This symptom signals that hydrocephalus is accompanied by other neurological disorders.
- Speech disorders, memory problems.
This is non-occlusive replacement hydrocephalus. The subarachnoid space is expanded, and fluid accumulates in it. An adult with this disease will experience the following symptoms:
- constant feeling of fatigue;
- nausea, vomiting;
- minor visual impairment;
- sweating;
- double vision;
- changes in sexual behavior;
- walking disorders.
Internal
If an adult has triventricular occlusive hydrocephalus, in which cerebrospinal fluid fills the spaces of the ventricles, he may suffer from:
- increased intracranial pressure;
- nausea, vomiting;
- severe headaches;
- problems with vision and hearing.
Diagnosis of vascular types of headaches
When examining a patient with a headache, the following patterns can be identified. With the arteriodilatatory variant, dilation of small arteries and capillaries on the face and a pink blush are noticeable. In the arteriolospastic variant, on the contrary, the skin is pale, marbled, the nasal mucosa is also pale, and patients do not tolerate cold well. In the venous variant, there is cyanosis of the nasal mucosa, pastiness of the face, especially the lower eyelids.
The simplest diagnosis of vascular variants of headaches is examination of the fundus. So, with the arteriodilatatory variant, you can see the expansion and tortuosity of small arteries. In the arteriolospastic variant, on the contrary, the fundus is lighter due to spasmodic arteries. With the venous variant, dilated veins are revealed, the fundus of the eye has a more intense color due to venous stasis.
However, the most diagnostically accurate is to conduct REG (rheoencephalography) to objectify vascular pathology. As a rule, it is necessary to perform two studies - during a headache attack and during its absence, in order to better see the changes occurring in the vessels of the head during an attack. Sometimes, to clarify vascular changes, pharmacological tests with nitroglycerin are performed.
The vascular type of headache occurs with migraine, vegetative-vascular dystonia, arterial hypertension, and systemic vasculitis. The effectiveness of pathogenetic treatment of vascular headache increases with adequate treatment of the underlying disease.
Treatment and specialists
Only a qualified specialist should treat cerebrospinal fluid dynamics disorders in newborns. Only a doctor can tell you how to treat hypertension in a baby, how to get rid of complications from impaired liquor flow and prevent its occurrence in the baby in the future.
Treatment of cerebrospinal fluid dynamics disorders in newborns is prescribed based on the factors that provoked the onset of the symptom. The doctor prescribes medications that correspond to the stage of development of the underlying disease and the form of manifestation of hypertension syndrome.
Arm yourself with knowledge and read a useful informative article about the disease liquorodynamic disorder in newborns. After all, being parents means studying everything that will help maintain a degree of health in the family on the island.
Find out what can cause the disease, liquorodynamic disturbance in newborns, and how to recognize it in a timely manner. Find information about the signs that can help you identify illness. And what tests will help identify the disease and make a correct diagnosis.
In the article you will read everything about methods of treating a disease such as liquorodynamic disorder in newborns. Find out what effective first aid should be. How to treat: choose medications or traditional methods?
You will also learn how untimely treatment of a disease with liquorodynamic disorders in newborns can be dangerous, and why it is so important to avoid the consequences. Everything about how to prevent liquorodynamic disturbances in newborns and prevent complications
Be healthy!
Treatment of intracranial pressure
Intracranial pressure needs to be normalized and treated. An integrated approach to the problem, even after the first courses of treatment, even in severely ill patients, gives positive dynamics, speech and psychomotor development in children improves. The earlier treatment is started, the faster the impaired functions are restored and intracranial pressure is normalized. At the first consultation, the doctor will tell you about the main factors and symptoms of the disease: what is hypertension syndrome in newborns, infants, infants, children, children, adults, what is mild, moderate, severe cerebral hypertensive syndrome , hypertensive syndrome , cerebrospinal fluid hypertensive syndrome , how the army and residual encephalopathy are related to hypertensive hydrocephalic syndrome, what intracranial pressure should be normal, how to measure, determine, check, and how to reduce, lower, relieve, treat intracranial pressure. On the website sarclinic.ru you can see a doctor online for free.
Sign up for a consultation. There are contraindications. Specialist consultation is required. Photo: Sergiyn | Dreamstime.com\Dreamstock.ru. The people depicted in the photo are models, do not suffer from the diseases described and/or all similarities are excluded.
Related posts:
Encopresis in children, neurotic encopresis, treatment of encopresis
Depression in adolescents, children, treatment of depression in Saratov
Paresis of the facial nerve in newborns, neuritis of the facial nerve in children, damage during childbirth
Sound, vocal tics in children: treatment, symptoms; adult tics
Speech aphasia in children, afrasia in children and adults
Comments ()
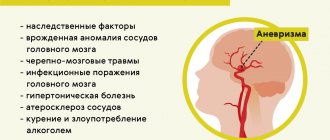
Causes of hydrocephalus in adults
A huge number of factors can provoke dropsy of the brain. The disease occurs due to:
- suffered a stroke;
- infectious diseases of the brain and membranes (meningitis, encephalitis, ventriculitis, tuberculosis);
- tumors;
- vascular pathologies, including aneurysm ruptures;
- head injuries and post-traumatic conditions (normotensive hydrocephalus);
- neurodevelopmental disorders;
- disturbances in the production, circulation, and absorption of cerebrospinal fluid;
- low brain matter density.
Hydrocephalus of the brain in an adult is diagnosed using the following methods:
- MRI. It helps not only to verify the correctness of the diagnosis, but also to determine its causes.
- CT scan.
- Cisternography. Diagnostics is used to determine the type of hydrocephalus.
- Neuropsychological examination.
- X-ray with contrast agent.
If, as a result of one or more of these studies, the prognosis is confirmed, the following treatment methods are used:
- Drug therapy. The option is suitable if hydrocephalus is moderate. An adult patient is prescribed medications that lower intracranial pressure (Lasix, Mannitol), diuretics. Light therapeutic massage is also used during the therapy. All this will help stabilize the adult patient’s condition, but not cure him, but achieve a subcompensated stage.
- Brain shunt. It is not used for chronic hydroencephalia, inflammation, or vision problems, but is effective for asymmetrical forms. An adult patient is given a drainage through which excess cerebrospinal fluid goes to other spaces of the body. The operation in the vast majority of cases gives a positive result. After some time, the adult completely returns to his normal life. Periodically, secondary shunt installation is necessary.
- Endoscopy. Effective for mixed, replacement, symmetric hydrocephalus. Endoscopic surgery is performed using micro-instruments. With their help, fluid and the cause that disrupts its circulation, for example, a tumor, are removed.
- Folk remedies. They are effective solely to suppress the symptoms that manifest hydrocephalic syndrome. It is recommended to use diuretic herbal decoctions (oregano, bearberry, parsley), juniper berries, and an alcohol solution of calamus root.
- Diet. In the case of hydrocephalus of the brain in an adult, it is necessary to follow nutritional rules aimed at improving the exchange of water-salt balance. You need to categorically avoid foods that cause fluid to accumulate in the body. This includes fresh bread, fatty meat and poultry, smoked meats, sausages, and sweets. Instead, you need to eat more fresh vegetables and fruits, cereals. Dishes are best cooked steamed.
General information
Cerebrospinal fluid or cerebrospinal fluid is contained in the ventricles of the brain and the spinal cord canal in an amount of 125 to 150 ml. It is a kind of derivative of blood plasma and performs a number of important functions:
- Protects the brain from concussions and impacts (shock absorption).
- Nourishes surrounding tissues (trophism).
- Participation in water-salt and protein metabolism (osmotic and oncotic balance).
- Antibody accumulation (immune defense).
- Regulation of intracranial and spinal circulation (hemocirculation).
Liquor is produced by the choroid plexuses located in the lateral and at the bottom of the fourth ventricle of the brain. From the latter, through special openings (Lyushka and Magendie), the liquid penetrates into the subarachnoid space and accumulates in its extensions (cisterns). Washing the cerebral hemispheres, cerebrospinal fluid is absorbed into the venous system through Pachionian granulations and arachnoid cells. The movement of cerebrospinal fluid is also influenced by blood flow, breathing and muscle contractions.
Liquor is extremely important for the normal functioning of the organs of the central nervous system, and its quantity is limited to strict limits.
The origin of cerebral hydrocephalus in an adult is somewhat different from the mechanisms of hydrocephalus in a child. Basically we are talking about disruption of three processes in the liquor circulation chain:
- Increased production (vascular papilloma).
- Blockage or compression of pathways (tumor, blood clot, adhesions).
- Insufficient absorption (inflammatory process).
Based on the foregoing, hypersecretory, occlusive (closed) and disresorptive (open) hydrocephalus are distinguished, respectively. These are the main factors of acquired hydrocele of the brain. Previously, mixed replacement hydrocephalus was additionally identified, when the expansion of the ventricles and subarachnoid space was combined with atrophic processes in the surrounding structures. However, now it is not considered as true dropsy, because the mechanisms of formation, circulation and absorption of cerebrospinal fluid are not impaired, and the increase in internal cavities occurs due to thinning of the brain tissue.
Thanks to the expansion of the diagnostic capabilities of modern medicine, it has become known that hydrocephalus can accompany almost any disease of the central nervous system. In many cases, it becomes a complication of the following pathology:
- Infectious and inflammatory diseases (meningitis, encephalitis).
- Intracranial hemorrhages (post-traumatic hematomas, ruptures of aneurysms and vascular malformations).
- Strokes (ischemic and hemorrhagic).
- Tumor processes.
- Encephalopathies (toxic, posthypoxic, etc.).
Therefore, a complete and timely examination is extremely important for subsequent treatment tactics. And if any symptoms of hydrocephalus appear, you should immediately consult a doctor
The cause of hydrocephalus may be hidden at any stage of the cerebrospinal fluid circulation, causing a disruption in the production, excretion or absorption of cerebrospinal fluid.
Anatomical and physiological features of liquor dynamics
Liquor or cerebrospinal fluid is a liquid medium formed in the choroid plexuses of the brain and spinal cord. It circulates in the same-named pathways, subarachnoid space and ventricles of the brain. Its main functions are:
- metabolic maintenance and regulation of neuronal activity in the structures of the central nervous system;
- ensuring relative constancy of the internal environment in brain tissue;
- protective function;
- level control and compensatory balance of intracranial pressure,
- control of both osmotic and oncotic pressure;
- ensuring cellular and humoral immunity, production of specific immunoglobulins.
From the choroid plexuses in the direction of the lateral ventricles, the cerebrospinal fluid enters the third ventricle through the foramen of Monro. Passing through the aqueduct of Sylvius, the cerebrospinal fluid enters the fourth ventricle. Bypassing the median and lateral foramina, it is directed to the cisterns of the cerebellum, optic chiasm, pons and other structures. Having reached the Sylvian fissure, it moves in a vertical direction into the subarachnoid space.
It is possible for cerebrospinal fluid to enter through the ependymal space in a diffuse manner.
Symptoms
Painful symptoms during liquorodynamic headaches are bursting and dull in nature, intensifying with overexertion, movement, and taking a vertical position. Any uncomfortable position of the body can provoke painful sensations, which are accompanied by vomiting and loss of consciousness. The course of pain is monotonous.
Symptoms of hypertension
Pain syndromes in the head with high blood pressure are intense. The appearance of pain in the depths of the head is characteristic. In such a condition, the rate of increase in liquorodynamic disorder is important: acute hydrocephalus always causes intense attacks. The following symptoms may appear:
- increased pain when sneezing and coughing;
- dizziness;
- decreased heart rate;
- loss of appetite.
Symptoms of hypotension
In conditions caused by a decrease in cerebrospinal fluid pressure, the pain is localized in the crown area, has moderate strength, but a long duration. The patient finds relief in lying down with his head down. It is also possible that:
- attacks of pain when coughing and sharp turns of the head;
- pulsating sensations in the intracranial arteries.
Consequences of liquorodynamic disorders
If you do not treat this disease in time, then after a short time after the onset of symptoms, adverse consequences may appear:
- Among them, the most common are cognitive impairment and memory impairment. A person may forget about events that happened to him recently. The ability to perceive information and remember gradually decreases.
- Children who have liquorodynamic disorders begin to develop worse than their peers, both mentally and physically.
- Constantly disturbing headaches prevent a person from performing his work duties normally. In many ways, the changes described above occur due to impaired nutrition of the brain substance. All brain cells, and in particular the cortex, are very sensitive to a lack of oxygen, and with prolonged or constant deficiency, their atrophy begins to occur. That is why adult children with severe manifestations of liquorodynamic disorders are forced to receive a disability group.
Preventive actions
It is very important to prevent the development of hydrocephalus and other disorders of cerebrospinal fluid dynamics in the intrauterine period.
Consultation with a geneticist is necessary for future parents who have a family history and have relatives with impaired cerebrospinal fluid circulation.
The main preventive measures in older age are:
- prevention and timely treatment of infectious pathologies;
- monitoring the performance of coagulation and anticoagulation systems;
- preventing the development of osteochondrosis and scoliosis.
The syndrome of liquorodynamic disturbances can be caused and provoked by many reasons. The importance of early diagnosis and treatment should be remembered in order to avoid severe clinical manifestations and consequences of the disease.
Treatment
The initial stages of hydrocephalus can be treated with medication. The following medications are used for this:
- to reduce intracranial pressure and remove excess fluid (provided that the outflow of cerebrospinal fluid is preserved) - diacarb (acetazolamide), mannitol and mannitol in combination with furosemide or lasix. Mandatory for this treatment is the correction of potassium levels in the body, for this they use asparkam (panangin);
- To improve the nutrition of brain tissue, Cavinton (vinpocetine), Actovegin (solcoseryl), gliatilin, choline, cortexin, Cerebrolysin, Semax, Memoplant, etc. are indicated.
Clinically advanced hydrocephalus is subject to surgical treatment; medication methods improve the condition for a short time.
Acute hydrocephalus, as a life-threatening condition, requires immediate neurosurgical treatment. It consists of craniotomy and the application of external drainages to ensure the outflow of excess fluid. This is called external ventricular drainage. In addition, through the drainage system it is possible to administer drugs that dilute blood clots (since intraventricular hemorrhage is one of the most common causes of acute hydrocephalus).
Chronic hydrocephalus requires cerebrospinal fluid shunting operations. This type of surgical treatment involves the removal of excess cerebrospinal fluid into the natural cavities of the human body using a complex system of catheters and valves (abdominal cavity, pelvic cavity, atrium, etc.): ventriculoperitoneal, ventriculoatrial, cystoperitoneal shunting. Unimpeded absorption of excess cerebrospinal fluid occurs in the body cavities. These operations are quite traumatic, but when performed correctly, they allow patients to recover and achieve their labor and social rehabilitation.
Today, the less traumatic neuroendoscopic technique has taken first place among invasive treatment methods. It is still more often performed abroad due to the high cost of the operation itself. This method is called: endoscopic ventriculocisternostomy of the bottom of the third ventricle. The operation lasts only 20 minutes. With this method of treatment, a surgical instrument with a neuroendoscope (camera) at the end is inserted into the ventricles of the brain. The camera allows you to display an image using a projector and accurately control all manipulations. An additional hole is created at the bottom of the third ventricle, connecting to the cisterns of the base of the brain, which eliminates the cause of hydrocephalus. Thus, the physiological fluid flow between the ventricles and cisterns is restored.
Symptoms of cerebrospinal fluid dynamics disorders
Intracranial hypertension syndrome
Intracranial hypertension syndrome develops as a result of a persistent increase in intracranial pressure above 200 mm of water column. Synonyms for intracranial hypertension syndrome are hypertensive syndrome, hypertensive syndrome.
Intracranial hypotension syndrome
Intracranial hypotension syndrome develops with a persistent decrease in cerebrospinal fluid pressure below 100 mm H2O. Art. Synonyms for intracranial hypotension syndrome are hypotensive syndrome, hypotensive syndrome.
Primary intracranial hypotension is quite rare. More often it develops as a result of liquorrhea (loss of cerebrospinal fluid), which can be observed after therapeutic and diagnostic interventions on the cerebrospinal fluid tract, as well as with arterial hypotension or an overdose of dehydrating drugs. The main symptom of intracranial hypotension is a headache, often of a squeezing nature (squeezing pain), which is relieved by lying down with the head down or by pressing the jugular veins. With intracranial hypotension syndrome, general weakness, dizziness, nausea, vomiting, and tachycardia are also observed. With a pronounced decrease in intracranial pressure, disorders of consciousness are observed from mild to stupor and coma.
CSF dystonia syndrome
CSF dystonia syndrome is characterized by instability of intracranial pressure and frequent changes. The symptoms of cerebrospinal fluid dystonia are the same as those of hypertension syndrome and hypotension syndrome.
Occlusive syndromes, Brunx attack
Occlusive syndromes develop as a result of blockade of the cerebrospinal fluid pathways at any level of the ventricular system. Clinically, occlusive syndromes are characterized by intracranial hypertension in combination with symptoms of damage to parts of the brain lying above the level of occlusion and the underlying disease. They are accompanied by Bruns' attacks. Bruns' attack has a number of symptoms - vomiting, rapidly increasing headache, impaired consciousness, forced head position, signs of brain stem dislocation. Obstruction to the outflow of cerebrospinal fluid can occur at any level of the ventricular system.
Vascular type of headache
The arteriodilatatory variant of the vascular type of pain is associated with a decrease in the tone of the craniocerebral arteries, which occurs when the blood vessels are excessively stretched by the pulse volume of blood. Excessive pulse stretching of the hypotonic arterial wall sometimes occurs at normal levels of systemic blood pressure, but more often when it increases. If the artery of the soft integument of the head (superficial, temporal artery) is subjected to excessive pulse stretching, then compression of the adductor trunk of the artery in the temporomygomatic region with a finger, as a rule, reduces pain.
Clinic: throbbing headache. When permeability is impaired and plasma impregnation of the arterial wall develops perivascular edema. In these cases, the amplitude of the pulsation decreases and the headache loses its pulsating character, becomes dull, then aching or bursting.
Therapy: anti-migraine drugs containing ergotamine, dihydroergotamine, sumatriptan are used to relieve pain. Ergotamine drugs relieve pain due to a powerful vasoconstrictor effect and prevent neurogenic inflammation. Ergotamine in combination with caffeine or with caffeine and dimenhydrinate is prescribed as monotherapy or in combination with analgesics, antiemetics and sedatives.
For vegetative-vascular dystonia, xanthine-type drugs are prescribed: aminophylline, pentoxifylline, xanthinol nicotinate, which are usually prescribed in a course 1-2 times a year. This group of drugs acts on smooth muscles, relaxing them, relieves spasm of blood vessels, reduces pressure in the pulmonary artery system, has a diuretic effect, and also inhibits platelet aggregation.
The arteriospastic variant occurs with spasm of the craniocerebral arteries and with an increase in arterial tone, which entails ischemic dyscirculation and ischemic hypoxia.
Clinic: the pain is aching and dull in nature, and is perceived as a feeling of compression. Pain, as a rule, is accompanied by nausea, unsystematic dizziness, darkening and flickering of “black spots” in the eyes.
Therapy: antispasmodic drugs are prescribed: phosphodiesterase inhibitors (papaverine, drotaverine), α-adrenergic blockers (dihydroergotoxin, nicergoline), calcium antagonists (nifedipine, nimodipine). For hypertension associated with impaired blood supply to the brain, drugs that improve cerebral circulation are used. Among the prescription drugs of this series, the most famous are the cerebrovasodilator vinpocetine, BMCA cinnarizine, piracetam, nicotinoyl gamma-aminobutyric acid. It must be remembered that these drugs are contraindicated in patients with acute cerebrovascular accidents, gastric and duodenal ulcers.
The venous variant is caused by excessive blood filling of the venous vessels and difficulty in venous outflow.
Clinic: a feeling of heaviness in the head and a feeling of dull distension. It occurs or worsens when lying down, as well as when working with your head low, as well as when straining or coughing. Morning headache is typical. Sometimes the pain is limited only to the back of the head.
Therapy: drugs of choice are also xanthine drugs, due to their venotonic effect and ability to reduce platelet aggregation, as well as mild venotonics, for example diosmin + hesperidin.
PATHOGENESIS OF POST-TRAUMATIC cerebrospinal fluid rhea
Anterior craniobasal and frontobasal injuries involve the paranasal sinuses; with lateral craniobasal and laterobasal - pyramids of the temporal bones and paranasal sinuses of the ear. The nature of the fracture depends on the applied force, its direction, structural features of the skull, and each type of skull deformation corresponds to a characteristic fracture of its base. Shifting bone fragments can damage the meninges.
H.Powiertowski identified three mechanisms of these injuries: entrapment by bone fragments, violation of the integrity of the membranes by free bone fragments, and extensive ruptures and defects without signs of regeneration at the edges of the defect. The meninges prolapse into the bone defect formed as a result of the injury, preventing its healing and, in fact, can lead to the formation of a hernia at the fracture site, consisting of dura mater, arachnoid membrane and medulla.
Symptoms in infants
With increasing pressure inside the skull, infants experience: bulging of the fontanel, enlargement of the head, a bright venous pattern under the skin, divergence of the cranial sutures.
In infants, liquorodynamic disorders are manifested by the following symptoms:
- frequent, profuse regurgitation;
- unexplained crying;
- prolonged overgrowth of the parietal fontanel;
- lethargy, drowsiness;
- sleep disturbance.
With muscle excitement and hysterical crying, the subcutaneous network of vessels near the nose, chest and neck is clearly visible.
When examined by a pediatrician, deviations in the structure of the skull are detected: excess growth in volume, elongated shape, divergence of cranial sutures, swelling, protrusion of a pulsating fontanelle.
These are noticeable signs of liquorodynamic disorders and progressive hydrocephalus.
A neurologist may find:
- hemiplegia;
- meningeal manifestations;
- paresis;
- extensor hypertonicity;
- Graefe's symptom (sign of the “setting sun”), which should disappear in newborns in 2-3 weeks, if it is not a sign of pathology;
- horizontal nystagmus (high-frequency oscillatory eye movements);
- developmental delay.
Symptoms of liquorodynamic disorders
With disorders that cause high blood pressure, patients usually suffer from severe headaches, which may be accompanied by a lack of appetite and even vomiting. Headaches tend to get worse when you sneeze or cough. Dizziness and bradycardia may also occur.
With liquor hypotension, a person also has a symptom such as headache, but it manifests itself mainly in the crown area. A sudden coughing attack or sudden movements can increase the pain. In such conditions, the patient experiences relief by being in a supine position, with his head down.
Neuralgic headache
This type of pain is classified into a separate group - facial pain (prosopalgia). In the pathogenesis of this type of headache, a key role is played by dysfunction of the central antinociceptive system of the brain with the formation of an irritative focus of pathological activity.
In most cases, the cause of facial pain is a focus of pathological activity in the central structures of nociception related to the trigeminal nerve system and its central projections. In some cases, neuralgia occurs when the sensory nerve is compressed through the mechanism of tunnel syndrome. It is this mechanism that is the main one in neuralgia of the occipital nerve, which is not included in the group of prosopalgia, but is cranial neuralgia.
Exacerbation of prosopalgia is also facilitated by circulatory disorders, hypothermia, infectious and allergic diseases, endogenous and exogenous intoxications, metabolic disorders, and vitamin deficiencies.
Clinic: the first distinctive feature of this type is their paroxysmal nature. In this case, short paroxysms, as a rule, follow one after another, often causing the patient to suffer from neuralgia for hours or days. The pain is usually piercing, shooting, “like lightning” or “electric current.” The second distinctive feature is the presence of trigger, or trigger, zones (dense, painful compactions along the nerves, the so-called myofascial syndrome, etc.), irritation of which provokes an attack. The third characteristic sign is the irradiation of pain to neighboring or distant areas.
Therapy: for neuralgia of central origin, treatment with antiepileptic drugs, such as carbamazepine, is most effective. The analgesic effect of the drug is associated with inhibition of synaptic transmission of stimuli in the spinal nucleus of the trigeminal nerve due to blockade of sodium channels in the membranes of hyperactive nerve cells, reducing the influence of excitatory neurotransmitters and enhancing inhibitory processes. In cases of compression of the sensory nerve endings, in addition to antiepileptic drugs, drugs with local effects are prescribed: lidocaine blockades, physiotherapy, acupuncture.
Classification
The diagnosis of hydrocephalus is made solely on the basis of the generally accepted clinical classification. In addition to the already mentioned forms of pathology, based on the peculiarities of the development mechanism (pathogenesis), it is necessary to mention other types of dropsy of the brain. According to the rate of development in adults, it is:
- Acute – decompensation for 3 days.
- Subacute – develops over 1 month.
- Chronic – formed over a period of 3 weeks to 6 months.
Hydrocephalus is also divided into groups based on cerebrospinal fluid pressure: hyper-, normo- or hypotensive. These features are important from a clinical perspective, since they largely determine the symptoms of the pathology.
The clinical picture of hydrocephalus is quite varied. The rate of manifestation and increase in symptoms depends on the severity of the pathological process in the central nervous system. With occlusive forms of hydrocephalus of the brain in an adult, the first signs of increased intracranial pressure are:
- Headache.
- Nausea, vomiting.
- Congestion in the fundus.
- Dislocation of brain structures.
The headache is bursting in nature, mainly localized in the frontoparietal region and is combined with a feeling of “squeezing out” the eyeballs. It intensifies in the morning, as well as when bending over, coughing, sneezing, and straining.
With severe hydrocephalus, signs of dislocation of brain structures are observed. Various degrees of disturbance of consciousness are observed - from drowsiness to coma. Oculomotor disorders occur in the form of nystagmus, displacement of the apples downward and outward (the “setting sun” symptom), and strabismus. With an intracranial hematoma on the side of the injury, pupil dilation (anisocoria) is noted. If compression of the medulla oblongata occurs (herniation into the foramen magnum), then respiratory and cardiovascular disorders are observed, which can lead to death.
Acute hydrocephalus in adults is associated not only with disruption of the central nervous system, but also with a high risk to life.
Chronic accumulation of cerebrospinal fluid, in particular replacement hydrocephalus of the brain, has a fundamentally different clinical picture. The first symptoms, as a rule, appear a month after the injury or neurological disease (stroke, meningitis, etc.) and gradually intensify. The main features are psycho-emotional, mental disorders and conduction disorders, manifested by the following conditions:
- Dementia.
- Apraxia of walking - an unsteady gait with legs widely spaced.
- Paresis and paralysis.
- Urinary incontinence.
At first, patients experience daytime drowsiness and nighttime insomnia (the sleep-wake cycle is disrupted). Then the memory for current events gradually deteriorates, the person becomes indifferent, depressed, and answers questions in monosyllables. Over time, intellectual-mnestic disorders worsen, leading to the impossibility of social life and self-care.
Chronic hydrocephalus in adults is accompanied by a complex of psychoneurological disorders that develop after a brain injury or disease.
Muscle tension headache (TTN)
This is the predominant form of primary headache, and its prevalence in the population, according to various studies, ranges from 30 to 78%. HDN leads to the most significant socio-economic consequences, but remains poorly understood. TTH occurs when the muscles of the soft covering of the head are tense or compressed.
There are two ways muscle tension headaches can occur:
- Under the action of central or systemic factors that facilitate and enhance transmission at the neuromuscular synapse (under stress, with neurosis, with thyrotoxicosis); in all cases of psychophysiological insufficiency (psycho-emotional or psychophysical), with somatic diseases, especially with a progressive course (hypertension); with incomplete adaptation after severe somatic or infectious-toxic diseases, as well as after head injuries.
- When tension in the muscles of the soft integument of the head occurs in response to pathological painful impulses during local processes (disease of the eyes, ears, paranasal sinuses, cervical osteochondrosis) - a segmental reflex mechanism.
Clinic: feeling of head being pulled together by a bandage or hoop/helmet. The pain can be local (forehead, parietal region, cervical-occipital region). It is quickly generalized, since tension from one muscle is transmitted to other muscles through the tendon aponeurosis of the helmet. TTH may be accompanied by nausea, non-systemic dizziness; patients find it unpleasant to comb their hair or wear a hat. The persistence of headaches makes patients irritable, they do not tolerate loud sounds, bright light, and sometimes there is a decrease in memory and performance.
Diagnostics: an electromyogram reveals an increase in the potentials of electrical activity of the muscles of the soft integument of the head.
Therapy: Nonsteroidal anti-inflammatory drugs (NSAIDs) are the drugs of choice for the treatment of tension-type headache.
NB! Non-steroidal anti-inflammatory drugs have many restrictions on their use; in particular, due to their ulcerogenic effect, they are contraindicated in inflammatory diseases of the gastrointestinal tract. The exception is paracetamol, which, unlike other NSAIDs, does not block the synthesis of prostaglandins in peripheral tissues.
Pathogenetic treatment of pain of central origin includes tranquilizers and antidepressants. Traditional tricyclic antidepressants are predominantly used. In treatment-resistant cases, β-blockers are prescribed in addition to antidepressants.
For cervical headache, which usually occurs as a result of sudden cervical movements, fatigue, colds, osteochondrosis, along with analgesics, doctors often prescribe central muscle relaxants - tolperisone, tizanidine, baclofen. This is explained by the fact that in the genesis of cervical headache, a significant role is played by central dysregulation of the tone of the cranial and cerebral arteries, the tone of the pericranial muscles, as well as a decrease in the threshold of pain perception.
In life, we very often encounter headaches of mixed origin. In practice, situations are often observed when the same patient has different types of headache, for example, migraine plus tension headache. The most universal and widely used drugs for hypertension of various origins are, of course, NSAIDs.
With segmental reflex genesis of pain, local methods of influence can play a significant role: lidocaine blockades, physiotherapy, acupuncture; and for diseases of the eyes, paranasal cavities, ears - treatment of the processes that caused excessive painful impulses by appropriate specialists.
Hypertension is often recorded in pediatric practice, primarily in schoolchildren, among whom the frequency of headache reaches 60%. Timely determination of the type and genesis of headache and provision of adequate therapy prevents chronic headache. Preference should be given to paracetamol and ibuprofen (suspensions), the use of which is allowed from the first months of a child’s life.
NB! Acetylsalicylic acid is not used for children under 14 years of age due to the risk of developing Reye's syndrome (acute hepatic encephalopathy), which is registered exclusively in pediatrics.
One cannot ignore such a separate group of patients as pregnant and lactating women. During this period, patients should be especially responsible about taking various medications and use them only when absolutely necessary. If rest, sleep, walks in the fresh air do not help and the headache does not go away, then you can resort to taking paracetamol. Other painkillers should not be used due to their ability to cross the placenta or be secreted in milk and cause adverse effects on the fetus or newborn.
Rate of cerebrospinal fluid formation and cerebrospinal fluid resorption
https://youtube.com/watch?v=7_VFq1TY-JI
treatment of hydrocephalus or cerebrospinal fluid system; cerebrospinal fluid resorption; cerebrospinal fluid formation; mlmin; cerebrospinal fluid formation; mlmin.
Stimulation of the cholinergic pathway increases the formation of cerebrospinal fluid up to 100% without interfering with choroidal blood flow. Recently, the role of cyclic adenosine monophosphate (cAMP) in the passage of water and solutes across cell membranes, including its effect on the choroid plexus, has been elucidated. The concentration of cAMP depends on the activity of adenyl cyclase, an enzyme that catalyzes the formation of cAMP from adenosine triphosphate (ATP) and the activity of its metabolization to inactive 5-AMP with the participation of phosphodiesterase, or the addition of an inhibitory subunit of a specific protein kinase to it. cAMP acts on a number of hormones. Cholera toxin, which is a specific stimulator of adenyl cyclase, catalyzes the formation of cAMP, and a fivefold increase in this substance is observed in the choroid plexus. The acceleration caused by cholera toxin can be blocked by drugs from the indomethacin group, which are antagonists to prostaglandins. It is controversial what specific hormones and endogenous agents stimulate the formation of cerebrospinal fluid along the path to cAMP and what their mechanism of action is. There is an extensive list of medications that affect the formation of cerebrospinal fluid. Some medications affect the formation of cerebrospinal fluid by interfering with cell metabolism. Dinitrophenol affects oxidative phosphorylation in the choroid plexus, furosemide affects chlorine transport. Diamox reduces the rate of spinal cord formation by inhibiting carbonic anhydrase. It also causes a transient increase in intracranial pressure, releasing CO2 from tissues, resulting in an increase in cerebral blood flow and brain blood volume. Cardiac glycosides inhibit the Na- and K-dependence of ATPase and reduce the secretion of cerebrospinal fluid. Glyco- and mineralocorticoids have almost no effect on sodium metabolism. An increase in hydrostatic pressure affects filtration processes through the capillary endothelium of the plexuses. When the osmotic pressure increases by introducing a hypertonic solution of sucrose or glucose, the formation of cerebrospinal fluid decreases, and when the osmotic pressure decreases by introducing aqueous solutions, it increases, since this relationship is almost linear. When the osmotic pressure changes by introducing 1% water, the rate of formation of cerebrospinal fluid is disrupted. When hypertonic solutions are administered in therapeutic doses, the osmotic pressure increases by 5-10%. Intracranial pressure depends much more on cerebral hemodynamics than on the rate of formation of cerebrospinal fluid.
Neuralgic headache
This type of pain is classified into a separate group - facial pain (prosopalgia). In the pathogenesis of this type of headache, a key role is played by dysfunction of the central antinociceptive system of the brain with the formation of an irritative focus of pathological activity.
In most cases, the cause of facial pain is a focus of pathological activity in the central structures of nociception related to the trigeminal nerve system and its central projections. In some cases, neuralgia occurs when the sensory nerve is compressed through the mechanism of tunnel syndrome. It is this mechanism that is the main one in neuralgia of the occipital nerve, which is not included in the group of prosopalgia, but is cranial neuralgia.
Exacerbation of prosopalgia is also facilitated by circulatory disorders, hypothermia, infectious and allergic diseases, endogenous and exogenous intoxications, metabolic disorders, and vitamin deficiencies.
Clinic: the first distinctive feature of this type is their paroxysmal nature. In this case, short paroxysms, as a rule, follow one after another, often causing the patient to suffer from neuralgia for hours or days. The pain is usually piercing, shooting, “like lightning” or “electric current.” The second distinctive feature is the presence of trigger, or trigger, zones (dense, painful compactions along the nerves, the so-called myofascial syndrome, etc.), irritation of which provokes an attack. The third characteristic sign is the irradiation of pain to neighboring or distant areas.
Therapy: for neuralgia of central origin, treatment with antiepileptic drugs, such as carbamazepine, is most effective. The analgesic effect of the drug is associated with inhibition of synaptic transmission of stimuli in the spinal nucleus of the trigeminal nerve due to blockade of sodium channels in the membranes of hyperactive nerve cells, reducing the influence of excitatory neurotransmitters and enhancing inhibitory processes. In cases of compression of the sensory nerve endings, in addition to antiepileptic drugs, drugs with local effects are prescribed: lidocaine blockades, physiotherapy, acupuncture.