1.1. Etiology and pathogenesis
Peripheral paralysis is always a consequence of damage to peripheral motor neurons and occurs both with damage to the bodies of these neurons located in the motor nuclei of cranial nerves or in the anterior horns of the spinal cord segments, and their axons that are part of various structures of the peripheral nervous system, as well as during blockade neuromuscular synapses.
Selective damage to the bodies of peripheral motor neurons is characteristic, in particular, of epidemic poliomyelitis and amyotrophic lateral sclerosis. Damage to the structures of the peripheral nervous system can be a consequence of trauma, compression, infectious-allergic lesions, etc., leading to the development of radiculopathies, plexopathies, neuropathies, mono- or polyneuropathies. Failure of neuromuscular synapses, which transmit nerve impulses from the nerve ending to the muscle using the mediator acetylcholine-H, occurs with myasthenia gravis and botulinum toxin poisoning.
1.2. Clinic
Peripheral paralysis is characterized by the following main symptoms:
- muscle atony or hypotonia;
- areflexia or hyporeflexia (decreased tendon, periosteal, skin reflexes);
- amyotrophy;
- qualitative changes in electrical excitability of muscles (reaction of degeneration, or degeneration);
- fibrillar (rapid contractions of individual muscle fibers when irritating SC motor neurons) and fascicular (rapid contractions of muscle fiber bundles when irritating the anterior roots or motor fibers of nerve trunks) muscle twitching.
In addition, changes in electrical excitability, called the degeneration reaction, develop in paralyzed muscles and affected nerves. The depth of changes in electrical excitability allows one to judge the severity of the lesion in peripheral paralysis and the prognosis. Loss of reflexes and atony are explained by interruption of the reflex arc; such a break in the arc leads to loss of muscle tone. For the same reason, the corresponding reflex cannot be evoked. Muscle atrophy, or sudden weight loss, develops due to the disconnection of the muscle from the neurons of the spinal cord; from these neurons, impulses flow through the peripheral nerve to the muscle, stimulating normal metabolism in muscle tissue. With peripheral paralysis, fibrillar twitching may be observed in atrophied muscles in the form of rapid contractions of individual muscle fibers or bundles of muscle fibers (fascicular twitching). They are observed in chronic progressive pathological processes in the cells of peripheral motor neurons.
Damage to a peripheral nerve leads to peripheral paralysis of the muscles innervated by this nerve. In this case, sensory disturbances and autonomic disorders are also observed in the same area, since the peripheral nerve is mixed - motor and sensory fibers pass through it. As a result of damage to the anterior roots, peripheral paralysis of the muscles innervated by this root occurs. Damage to the anterior horns of the spinal cord causes peripheral paralysis of the muscles in the areas of innervation by this segment.
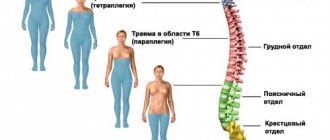
Thus, damage to the anterior horns of the spinal cord in the area of the cervical thickening (the fifth - eighth cervical segments and the first thoracic) leads to peripheral paralysis of the arm. Damage to the anterior horns of the spinal cord at the level of the lumbar enlargement causes peripheral paralysis of the leg. If the cervical or lumbar thickening is affected on both sides, then upper or lower paraplegia develops.
An example of peripheral limb paralysis is the paralysis that occurs due to polio. With polio, paralysis of the legs, arms, and respiratory muscles can develop. When the cervical and thoracic segments of the spinal cord are affected, peripheral paralysis of the diaphragm and intercostal muscles is observed, leading to respiratory failure. Damage to the upper thickening of the spinal cord leads to peripheral paralysis of the arms, and the lower (lumbar thickening) leads to paralysis of the legs.
Manifestations of peripheral paralysis in various syndromes:
Facial nerve syndrome: In children, inflammatory lesions of the facial nerve often occur, leading to peripheral paralysis of the facial muscles. On the side of the lesion of the facial nerve, the folds in the forehead are smoothed, the eyebrow is slightly lowered, the palpebral fissure does not close, the cheek hangs down, the nasolabial fold is smoothed, and the corner of the mouth is lowered. The patient cannot stretch his lips forward, blow out a burning match, or puff out his cheeks. When eating, liquid food pours out through the lowered corner of the mouth. Paresis of the facial muscles is most pronounced when crying and laughing. These disorders can sometimes be accompanied by lacrimation, increased sensitivity to auditory stimuli (hyperacusis), and taste disturbance in the anterior two-thirds of the tongue.
Less commonly, peripheral paralysis of the facial muscles is caused by underdevelopment of the nuclei of the facial nerve. In such cases, the lesion is usually bilateral and symmetrical; symptoms are observed from birth and are often combined with other developmental defects.
Bilateral damage to the facial nerve, most often its roots, can also be observed with multiple neuritis (polyneuritis), inflammation of the meninges (meningitis), fractures of the bones of the base of the skull and other skull injuries.
Oculomotor nerve syndrome: damage to the oculomotor and abducens nerves leads to paralysis of the muscles they innervate and the occurrence of strabismus.
in patients with damage to the oculomotor nerve, divergent strabismus occurs, since the healthy external rectus muscle, innervated by the abducens nerve, pulls the eyeball in its direction. When the abducens nerve is damaged, convergent strabismus develops for the same reason. When the trochlear nerve is damaged, strabismus, as a rule, does not occur. There may be a slight convergent squint when looking down. If the oculomotor nerve is damaged, drooping of the upper eyelid (ptosis) may occur due to paralysis of the muscle that lifts the upper eyelid, as well as dilation of the pupil (mydriasis) due to paralysis of the muscle that constricts the pupil, and impaired accommodation (deterioration of near vision).
With paralysis of the extraocular muscles, the eyeball may protrude from the orbit due to a decrease in their tone (exophthalmos). When looking to the side with a paralyzed muscle, double vision (diplopia) occurs.
Hypoglossal nerve syndrome: Damage to the hypoglossal nerve or its nucleus in the brainstem causes peripheral paralysis of the corresponding half of the tongue. Atrophy of the tongue muscles (thinning of the paralyzed half of the tongue), hypotonia (the tongue is thin, spread out, elongated), deviation of the tongue when it protrudes towards the paralysis, and fibrillary twitching are observed. Movement of the tongue in the affected direction is limited or impossible. Possible disturbance of sound pronunciation - dysarthria.
Accessory nerve syndrome: When the accessory nerve or its nucleus is damaged in the brain stem, peripheral paralysis of the sternocleidomastoid and trapezius muscles develops. As a result, the patient experiences difficulty turning his head to the healthy side and, if necessary, raising his shoulder. Lifting the arm above the horizontal line is limited. Shoulder drooping is observed on the affected side. The lower angle of the scapula extends from the spine.
Syndrome of combined damage to the glossopharyngeal, vagus and hypoglossal nerves (bulbar syndrome): with damage to the glossopharyngeal and vagus nerves, motor disorders are characterized by peripheral paralysis of the muscles of the pharynx, larynx, soft palate, trachea, tongue. This condition is called bulbar palsy. Paralysis of the muscles of the pharynx leads to difficulty swallowing. When swallowing, patients choke. Paralysis of the muscles of the epiglottis leads to the entry of liquid food into the larynx and trachea, and paralysis of the soft palate leads to the flow of food into the nasal cavity. Paralysis of the mouse larynx leads to sagging of the ligaments and to aphonia or hypophonia (the voice becomes silent). Due to the sagging of the soft palate, the voice may take on a nasal tone. The tongue deviates to the healthy side. Due to tongue paralysis, chewing is impaired. The tongue deviates to the affected side, its movements are difficult. Atrophy and hypotonia of the tongue are observed. There is a violation of sound pronunciation: bulbar dysarthria develops. The palatal and pharyngeal reflexes disappear. The vagus nerve provides autonomic innervation to blood vessels and internal organs (including the heart). Its bilateral defeat causes death due to cardiac and respiratory arrest.
Leg muscle paralysis: causes, methods of diagnosis and treatment
If the cause of the cut is a progressive neurological disease, it cannot be completely cured.
There are many treatment methods, they can be divided into the following groups:
- conservative methods - massage, physical therapy (therapeutic exercise), special devices - foot holders;
- surgical intervention;
- folk remedies.
Conservative methods in the treatment of foot paresis are used to restore normal tissue functioning.
Foot massage improves blood circulation, reduces muscle tone, and serves to prevent changes in the foot that are unusual for normal functioning. It is carried out on two legs at the same time, by two massage therapists at once. Massaging begins from the bottom of the foot and goes up.
Exercise therapy helps to strengthen muscles and correct defects that have arisen, and foot holders and plaster casts increase the mobility of the foot by assisting the muscles in lifting and moving the leg. Therapeutic gymnastics for paresis is carried out strictly under the supervision of specialists practicing in this field and having the appropriate education, since although this is a fairly effective method of treatment, incorrect exercises can provoke not only improvements, but also cause harm to the body.
Exercises by a physical therapy instructor are selected individually, based on the characteristics of the body and the causes of leg injury.
Physical therapy for paresis is used together with massage, medications, and physiotherapy.
Exercise therapy may include exercises by fixing a certain body position, for example, the patient gradually assumes a vertical position, while being fixed with straps on a special rotary table (effective in the early stages). This is orthostatic gymnastics for foot paresis, which allows a person to be in a semi-vertical or vertical position, which has a beneficial effect on the normal urge to urinate, and trains the vestibular apparatus.
A special place in the treatment of exercise therapy is occupied by exercises after surgery, which resulted in paralysis. These exercises are divided into 4 stages and last more than 40 days. Their task is to eliminate movement disorders, restore movement skills, and improve the respiratory and cardiovascular systems.
Treatment with gymnastics implies a decrease in muscle tone and an increase in their strength, prevention and elimination of movements unusual for the normal functioning of all human skills.
Surgery is performed to restore the functionality of the foot when the cut to the foot is so severe that the person cannot walk independently. After the operation, you will need to wear special orthopedic shoes for the period prescribed by the doctor.
The operation is aimed at removing the hernia and releasing the affected area from compression.
Folk remedies consist of using infusions that have a beneficial effect on the human immune and nervous system, from herbs such as chamomile, rose hips, elderberry and others.
Depending on the causes of paresis, different courses of treatment methods may be prescribed:
- for injuries to the brain or spinal cord, as a rule, antibacterial drugs are used;
- for botulism - antibotulinum serum;
- in case of poisoning, it is recommended to strengthen the immune system;
- for a chronic disease characterized by pathological fatigue and muscle weakness, take medications that affect neuromuscular conduction;
- For brain tumors, only surgery is recommended.
Medicines
2.1. Goals and objectives of massage
Peripheral paralysis is characterized by deeper functional disorders of the motor system than spastic ones.
For flaccid paralysis, a deep and moderately hard massage is performed. Objectives of massage for flaccid paralysis:
- improve blood and lymph circulation;
- reduce pain;
- help accelerate the regeneration processes of affected nerve fibers;
- strengthen paretic muscles;
- counteract the formation of contractures and deformities;
- increase muscle tone and strength;
- reduce their atrophy;
- promote movement restoration;
- improve and strengthen the general condition of the patient.
Features of hand massage after a stroke
What points should you pay attention to when starting to massage a paralyzed arm?
- The person should lie on their back, side, or sit (if possible). Lying on his stomach may cause his blood pressure to rise; such a massage at home can only be performed in the late period of rehabilitation and with the permission of a doctor.
- The upper body should be elevated by placing a pillow under the back and adjusting the bed.
- In the usual version of the massage, movements are performed towards the center of the body. In this case, the opposite direction is used (from the shoulder girdle to the hand) to avoid an increase in pressure levels.
- Also, due to a possible increase in pressure, gently massage the shoulder girdle.
- You cannot use massage techniques such as chopping, enhanced deep vibration, squeezing, and the like. Use stroking and rubbing.
- Before the massage, you need to warm up your hand. You can put a warm heating pad nearby and cover with a blanket.
- After the massage, several passive movements should be performed (flexion, extension, abduction and adduction).
- The duration of the session, as well as the number of procedures per course and the frequency of their implementation, is determined by the attending physician; it depends on the type of stroke and the nature of the disorders. In case of hemorrhagic stroke, massage can be done a week after the attack, and in the case of ischemic stroke - within a day (depending on the condition). Typically, a massage course after a stroke is about 30 sessions, then you need to take a break for two months. After which it is continued (with the changes made). The duration of one procedure depends on the stage of recovery and ranges from 5–30 minutes.
- When performing massage procedures at home, strict adherence to instructions is necessary to avoid complications.