Spinal cord myelitis is a general name for all inflammatory diseases affecting the spinal cord. Myelitis can develop due to an allergic or infectious lesion. Often the pathological process spreads to several (1-2) segments of the patient’s spinal cord, but there are cases when their number increases under the influence of certain factors. The disease is accompanied by many symptoms, the main of which is disruption of the spinal cord. If the patient is not provided with timely assistance, myelitis can result in serious complications.
Myelitis of the spinal cord
Reasons for appearance
Varieties of myelitis are divided into two main groups, which are formed based on the order of occurrence of the lesion process:
- Primary. Pathology is the result of direct damage (infection, injury) to the patient’s spinal cord.
- Secondary. The disease develops against the background of another disease or is its complication (that is, a consequence of secondary infection).
There is simultaneous inflammation of the brain and spinal cord.
Classification
There is a classification according to the mechanism of occurrence of the inflammation process. Depending on this, myelitis is divided into the following categories:
- traumatic;
- infectious;
- idiopathic (etiology unclear);
- intoxicating.
Infections of an infectious nature are produced predominantly hematogenously, through the blood supply (the only exception is infection in an open wound). The method of penetration of viral infections in primary type myelitis involves the direct entry of viruses through the bite of infected people and animals, blood-sucking insects, or unsterile medical instruments into the blood. The most likely causative agents of infectious primary myelitis are neurotropic (having the ability to penetrate neurons) viruses of tetanus, influenza, measles, chickenpox, rabies, mumps, lichen, polio, various types of herpes (cytomegalovirus, herpes simplex, Epstein-Barr). How else does inflammation of the spinal cord occur?
Classification and causes of the disease
In accordance with the international classification, inflammation of the spinal cord is divided into several types. In accordance with the characteristics of the pathological process, the following are distinguished:
- Acute myelitis. The disease is characterized by a rapid onset and pronounced symptoms. Acute myelitis has a severe course and leads to various complications.
- Subacute disease. Characterized by a gradual onset of symptoms. The pathological process is progressive.
- Chronic illness. It is most often diagnosed in older people.
Inflammation of the spinal cord has several forms depending on the causes of its occurrence. Infectious myelitis is primary and secondary. The pathological process appears when the body is exposed to various infections and viruses. The appearance of the disease is observed when exposed to:
- Enteroviral infections;
- Mycoplasma;
- Syphilis;
- Meningococcal infection;
- Herpes virus;
- Cytomegalovirus infection.
Radiation myelitis occurs in people with cancer treated with radiation therapy. Traumatic forms of the disease develop after various spinal injuries - dislocations, sprains, fractures, against the background of which the penetration of viral infections into the spinal cord is observed.
There are autoimmune causes of the disease, which involve the body producing antibodies to its own cells. The appearance of toxic myelitis of the spinal cord is observed after poisoning the body with toxic substances. If a patient is prone to an allergic reaction and is vaccinated, this can lead to pathology.
Spinal cord myelitis develops when the body is exposed to various provoking factors, which are recommended to be excluded from life.
Provoking factors of secondary type infection
Foci of infection of a secondary type appear in the spinal cord also as a result of the movement of bacteria through the blood supply. The following pathogens are known:
- fungal (Cryptococcus, Blastomyces, Aspergillus);
- bacteria (syphilis, tuberculosis);
- parasites (trematodes, helminths).
Traumatic sources of inflammation:
- irradiation (high-energy radiation);
- electric shock;
- decompression sickness.
Metabolic disorders:
- percinous anemia (neuron death, demyelination, vitamin B12 deficiency); diabetes;
- chronic liver diseases.
In addition to the factors listed above, the inflammatory process in the spinal cord can be provoked by toxic substances (including anesthesia during spinal surgery), collagenosis (connective tissue diseases), heavy metals, inflammation of the meninges (arachnoiditis), and autoimmune diseases.
Inflammation of the spinal cord can be caused by the administration of a vaccine for any of the viral diseases listed above.
Possible complications
The presence of an inflammatory process in the brain (regardless of the type of disease and the stage of its development) is an extremely dangerous condition for human health. Even after a completely cured pathology, the patient may encounter various unpleasant consequences and complications:
- Hearing problems.
- Problems with remembering new information and reproducing old information.
- Strabismus (in various forms), progressive deterioration of vision (usually myopia).
- Decreased intellectual abilities.
- Development of various forms of epilepsy.
- Malfunction of the thyroid gland and other internal organs.
- Problems with coordination of movements.
- Disturbances in the functioning of the cardiovascular system.
When there is inflammation in the brain, there is almost always a possibility of death. If adequate treatment is not carried out, the patient may well die within 4-7 days after the first symptoms of the disease appear.
Features of development
The infection enters the spinal cord from the outside either hematogenously or lymphogenously from the primary focus (with lymph or blood). The second route of penetration is the myelin sheaths or fibers of the spinal cord nerves.
First, the space between and under the membranes becomes infected, then the main brain tissues (white and gray matter) are affected.
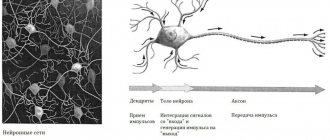
The spinal cord is divided into segments that correspond in size to the vertebrae. Each segment is responsible for reflexes and transmits signals from a specific muscle group or internal organ to the brain and back. Myelitis, depending on the number of infected segments, is defined as limited (localized), distributed among segments (disseminated) or focal (in unrelated or adjacent segments). Opticomyelitis is distinguished separately when transverse myelitis and optic neuritis, which is characterized by demyelination, are combined.
1.What is myelitis? Types of myelitis and risk factors
The diagnosis of myelitis covers the entire spectrum of inflammatory diseases of the spinal cord. Any process of this kind, localized in its white or gray matter, poses a serious threat. The prevalence of myelitis is not high (5 cases per 1 million people). The risk of developing spinal inflammation does not depend on gender or age. According to some studies, the incidence is higher among adolescents and the elderly, which, however, may be due to a greater likelihood of injury and instability of the immune status in these age groups. Myelitis is difficult to treat and often leaves irreversible functional impairment.
The prognosis largely depends on the stage at which treatment is started. However, the initial signs of inflammation in the spinal cord are similar to the symptoms of a number of other diseases of non-infectious origin. For this reason, patients experiencing back pain and sensitivity disorders may not consult a doctor in a timely manner, attributing these manifestations to age, physical activity, and stress. More often, diagnosis is carried out already at the stage of paralysis, paresis, and pelvic function disorders, when a person detects atypical symptoms.
Types of myelitis and risk factors
Depending on the etiology, infectious, intoxicating and traumatic myelitis are distinguished. In addition, this pathology can be primary or develop against the background of existing diseases.
Primary infectious myelitis is observed in the symptom complex of tuberculosis, syphilis, herpes, HIV, meningitis. In this case, the source of infection is localized directly in the spinal cord. Secondary pathogens can be introduced through the bloodstream during general infectious diseases (pneumonia, influenza, measles, typhus, scarlet fever). There is also a high probability of spread of pathogenic flora to the substance of the spinal cord with spinal ostiomyelitis.
Traumatic myelitis develops as a result of a violation of the integrity of the spine with simultaneous penetration of infection into the medulla. Weakened immunity in combination with a violation of the principles of antiseptics during surgical treatment or infection of the victim before first aid can give rise to an inflammatory process in the spinal substance.
Intoxication myelitis becomes a consequence of acute poisoning or long-term constant action of neurotoxic substances (a typical example here is work in hazardous industries).
It is also worth noting that myelitis can develop as a component of paraneoplastic syndrome in cancer or be a consequence of certain autoimmune diseases.
A must read! Help with treatment and hospitalization!
By localization
Based on localization in the brain stem, myelitis is divided into:
- transverse (the affected area is the white and gray matter of the brain in a number of segments at once);
- anterior (affected area - white matter in the zone of the median anterior groove);
- peripheral (the white matter of the brain is affected on the lateral and posterior sides);
- central (gray matter is affected).
The source of inflammation of the gray matter of the spinal cord is the response of the immune system to the presence of a pathogenic factor.
By intensity
The disease according to the intensity of the reaction is defined as:
- Acute, which develops quickly, deep tissue damage, there may be several foci of development.
- Subacute. Slowly develops, accompanied by pain of unknown origin, starting from the lower sections.
- Chronic. It develops over several years, accompanied by defects in tissue nutrition. The main cause of disease: the first type of T-lymphotropic virus and HIV infection.
The main result of the activity of immune cells is neuronal degeneration and demyelination of the closest conducting nerves, which are involved in the inflammatory process. Necrotization of nerve tissue manifests itself in the form of an increase in fragments of cell structures in the cerebrospinal fluid.
Inflammation of the spinal cord is expressed in the form of swelling, tissue swelling, and a blurred boundary between the white and gray matter (visible on MRI). If you zoom in a lot, you can see blood clots in the capillaries, microscopic hemorrhages, destruction of cell walls, and disintegration of the neuronal myelin sheath.
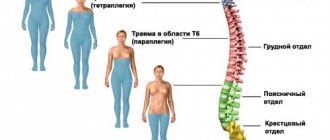
The disease most often (about 40% of cases) affects the thoracic vertebral region and the lower part of the spinal column. In terms of frequency of infection, the second place is the upper half of the chest, lower back and thoracic-lumbar junction. The neck region is rarely infected. Most often, adjacent pairs of vertebrae or several sections are affected (disseminated inflammation).
Symptoms and treatment of spinal cord inflammation are interrelated.
Symptoms
The symptoms of myelitis vary clinically. Their severity is determined by the degree and level of inflammation of the spinal cord. The main ones are the following:
- sensory defects;
- unpleasant sensations of pain;
- dysfunction of the pelvis;
- paralysis.
The first symptoms of inflammation of the spinal cord are similar to the signs of any infectious process: general weakness, chills, increased body temperature up to 39˚. The presence of neurological pathology is indicated by back pain that can spread to neighboring tissues from the affected area.
Severely developed inflammation of the spinal cord substance leads to loss of sensory and motor functions.
Myelitis
The clinical picture of myelitis depends entirely on the location of the inflammation. The level of damage is determined by segments or sections of the spinal cord (each of which has several segments). For example, myelitis can be thoracic, upper cervical, lumbar, etc. As a rule, myelitis covers the entire diameter of the spinal cord segment, disrupting the functioning of all conduction systems. This means that both spheres are disrupted: motor and sensitive.
It is worth describing the symptoms of myelitis taking into account the time of their onset. From the onset of the disease to its peak, the clinical manifestations of the disease change markedly. The first signs of infectious myelitis are completely nonspecific and differ little from other infectious diseases. An acute onset, a sharp increase in body temperature to 38-39˚C, chills, weakness - all “standard” signs of any inflammatory process. Then the disease begins to acquire its characteristic features. The first neurological symptom is usually back pain. It can be very intense (this varies from person to person). Pain in myelitis is not localized in one area: the pain spreads to neighboring areas of the body. Its irradiation (actually, the spread of pain) is a sign of damage to the roots of the spinal cord (radiculitis). The pain can “radiate” to the back, perineum, hips, etc. It all depends on the level of the lesion. Symptoms become more severe over time, and in some cases this “evolution of symptoms” can occur over a period of hours or days.
As already mentioned, the clinical picture of myelitis varies depending on the level of inflammation. Myelitis of the upper segments of the cervical spinal cord is characterized by spastic tetraparesis. It is the most dangerous: there is always a possibility of damage to the phrenic nerve. This, in turn, threatens to stop breathing. The spread of inflammation from the upper cervical segments upward to the structures of the medulla oblongata can lead to bulbar disorders. Myelitis at the level of the cervical thickening is manifested by a combination of flaccid paresis of the arms with spastic paresis of the legs. The lower segments of the cervical spine are affected more often than the upper ones, and their inflammation is not as dangerous. In some cases, it threatens with persistent motor impairments (myelitis of this localization, as a rule, is not life-threatening).
The thoracic region of the spinal cord is perhaps most often affected. Damage to this area causes the development of spastic paralysis of the legs. The latter is tension paralysis. At the same time, the muscles acquire excessive tone, and cramps may appear. The response to testing the knee and Achilles reflexes in thoracic myelitis is always too active. It is worth remembering that with rapidly developing transverse myelitis, decreased muscle tone may first be observed, then, after some time, the disorders acquire the character of spastic paralysis.
The lumbosacral spinal cord is also often affected by myelitis. Symptoms of myelitis of this localization include peripheral paresis in the legs and disorder of pelvic functions such as urinary and fecal incontinence. In parallel with this, the muscles that are innervated by the affected nerves, deprived of normal regulation and nutrition, gradually atrophy.
Sensory disturbances are observed in any type of myelitis. The only unshakable rule: this kind of disorder always occurs below the site of the lesion. Sensitive disorders consist of a decrease or complete absence of pain sensitivity, a decreased reaction to touch, cold, etc. Paresthesia may occur - “non-existent sensations”, for example, “goosebumps”, cold or the feeling of wind.
Diagnostic features
The infectious origin of acute myelitis can be recognized by its characteristic signs, as confirmed by neurological tests. To identify less pronounced chronic and subacute forms, you can use imaging diagnostic methods.
Computed tomography using a contrast agent or magnetic resonance imaging are the leading imaging methods. In addition, myelography (a less effective type of fluoroscopy) is used.
How is the pathogen determined?
The infectious pathogen is determined through bacteriological analyzes of CSF, studies of exudates and blood in the affected area. Spinal cord fluid samples are tested for lymphocyte counts, protein content, and physical changes. If there are large numbers of neutrophils, this indicates the severity of the pathology.
Tests and symptoms may indicate diseases that are similar in their development mechanism: malignant tumors, multiple sclerosis, epiduritis (epidural purulent abscess), arachnoiditis, polyneuropathy, encephalomyelitis. With the help of differential diagnosis, the diagnosis is clarified.
Diagnostics
Diagnosis of transverse myelitis is based on clinical and radiological data. Clinical characteristics of myelopathy are signs and/or symptoms of sensory, motor, or autonomic dysfunction related to the spinal cord. Evidence of inflammation is often observed, either on gadolinium-enhanced MRI or lumbar puncture, in the form of increased CSF leukocytes or IgG index, or the presence of oligoclonal IgG bands unique to the CSF.
If myelopathy is suspected based on the history and physical examination, a gadolinium-enhanced MRI of the spinal cord is first performed to evaluate whether there is a compressive or inflammatory (gadolinium-enhancing) lesion or stroke of the spinal cord, as signs and symptoms may be similar. It is important to rule out compressive myelopathy (compression of the spinal cord), which can be caused by a tumor, herniated disc, hematoma, or abscess. Recognizing these abnormalities is critical because immobilization to prevent further damage and early surgery to relieve compression can sometimes reverse neurological damage to the spinal cord.
Lumbar puncture is used to look for surrogate markers of inflammation in the cerebrospinal fluid. These include increased white blood cell counts in the cerebrospinal fluid, increased protein in the cerebrospinal fluid, and an increased IgG index/or the presence of oligoclonal IgG bands unique to the cerebrospinal fluid. However, it should be noted that a significant percentage of patients with a clinical presentation that otherwise resembles transverse myelitis do not fit these inflammatory characteristics, and therefore the absence of inflammatory markers does not exclude transverse myelitis.
To determine the underlying cause of inflammation, specific tests are recommended to evaluate for the presence of systemic inflammatory disease, such as Sjögren's syndrome, lupus erythematosus (SLE), and neurosarcoidosis. It is important to check your vitamin B12 and copper levels. NMO-IgG should be tested and, if negative, a MOG-IgG test should be ordered. It is necessary to exclude the causes of infection.
MRI of the brain is performed to identify lesions indicating multiple sclerosis or other diseases (neuromyelitis optica, acute disseminated encephalomyelitis, neurolupus, Sjogren's neuro-syndrome, neurosarcoidosis) that can affect not only the spinal cord but also the brain. If no clear cause can be identified, the diagnosis is idiopathic transverse myelitis.
Noninflammatory myelopathies include those caused by arterial or venous ischemia (blockage), vascular malformations, radiation, or nutritional/metabolic causes, and appropriate workup in these situations may include aortic ultrasound, spinal angiography, or evaluation of prothrombotic risk factors.
Within the category of idiopathic transverse myelitis, it may be useful to distinguish between acute partial form, acute complete form, and longitudinally extensive transverse myelitis, as these syndromes present different differential diagnoses and prognoses.
Acute partial transverse myelitis refers to mild to severely asymmetric spinal cord dysfunction involving less than 3 vertebral segments on MRI. Acute complete form of the disorder refers to complete or nearly complete clinical dysfunction below the lesion and MRI lesions of less than 3 vertebral segments. Longitudinally extensive transverse myelitis has a complete or incomplete clinical picture, but the lesion on MRI is longer than or equal to 3 vertebral segments.
Treatment
It is advisable to treat spinal cord inflammation in an inpatient setting or under constant medical supervision. The correct position of the human body in bed and continuous care will ensure minimal tissue and skin damage, since myelitis often causes trophic disorders, which, in turn, provoke the development of bedsores in the patient.
Inflammatory processes become stable and are reduced through hormonal medications (corticosteroids). Bactericidal and antiviral treatment (antibiotics, sulfonamides, immunostimulating agents) ensures accelerated destruction of the infectious pathogen.
To prevent the occurrence of bedsores, procedures are regularly done to improve trophism and blood circulation: ultraviolet irradiation, bandages with healing ointments, washing the skin with potassium permanganate.
When gangrenous lesions appear, therapy involves surgical intervention (necrotic tissue is excised).
If there are defects in the functioning of urination, a catheter is placed in the victim. To prevent diseases of the urinary system, regular rinsing with an antiseptic is performed. Stimulants help the patient strengthen degrading muscle tissue. High tone and muscle contractures in spastic paralysis are softened with muscle relaxants. Thanks to the use of anticholinesterase drugs, conductivity in motor neurons of excitation nerves improves.
Gymnastics and massage
Careful gymnastics, as well as massage, improve muscles and reduce tension in the ligaments during inflammation of the spinal cord roots. During the recovery period after stabilization of motor defects, the patient is recommended to do exercises to restore the elasticity and mobility of the ligaments.
Restorative complex treatment of inflammation of the spinal cord involves physiotherapy: electrophoresis with biologically active substances and drugs, electrical stimulation in the spinal region. In addition, balneological procedures (mud treatment, mineral baths) are desirable.
Determining the prognosis of the pathology is influenced by many factors: the condition and age of the patient, the type of disease (secondary or primary, accompanied by other neurological disorders), the occurrence of the inflammatory process and infection. Positive dynamics prevail in the overall statistics.
Localization Features
According to its localization, arachnoiditis has the following features:
- Cerebral arachnoiditis (inflammation of the brain). It covers mainly the postcranial fossa, as well as the base and surface: Convective. During inflammation, the gyri and the outer surface of the hemispheres are affected. The confective type of pathology leads to motor and sensory disturbances, as well as seizures;
- Sticky. It is extremely difficult to detect due to the lack of a specific localization. This type of disease is characterized by general symptoms characteristic of many pathological processes;
- Optical-chiasmal. In this case, the inflammation is basal, that is, located at the base. The main symptom of such a localization is blurred vision;
- Posterior cranial fossa. Usually, due to this location of the inflammatory process, the patient loses coordination of movements and increases intravenous pressure.
- Spinal arachnoiditis (inflammation of the spinal cord). It has the following localization features: Adhesive. Such a focus of inflammation is characterized by a latent course with signs characteristic of sciatica, neuralgia, etc.
- Cystic. This type of inflammation is characterized by severe pain and difficulty moving. Gradually both sides of the back are covered;
- Cystic-adhesive. Typically, this type of disease occurs without any particular symptoms, but over time, problems with movement appear and sensitivity is impaired.
Disease prognosis
In case of inflammation of the spinal cord, its prognosis is determined by the location of the pathology, its form and severity. As a rule, doctors give a sharply negative prognosis only for the meningococcal type of infection. Other varieties can be treated quite effectively.
The recovery process after inflammation of the spinal cord can take a long period. The patient is given a non-working second disability group with medical recertification every year. It is believed that complete restoration of mobility of the lower extremities after spinal cord myelitis is possible literally 6-8 months after the onset of the disease. With a transverse lesion of the spinal cord of a stroke-like nature, paraplegia and paralysis may persist. It can also end in absolute recovery.
With a similar frequency, there are cases that are accompanied by a gradual progression of symptoms, ultimately ending in the death of the patient over 5-6 years. The most unfavorable prognosis is if the inflammatory focus is localized in the lumbosacral region. There is also a certain danger if the cervical spine is affected.
The highest probability of a patient’s recovery after myelitis is observed with timely medical care. When a patient consults a doctor at the stage of loss of sensation in the limbs, the possibility of full recovery will be significantly reduced.
We now know what inflammation of the spinal cord roots is called.
Symptoms of pathology
The appearance of signs of acute myelitis is observed within 24 hours after the penetration of pathogenic microorganisms into the spinal cord. The patient experiences a sharp increase in body temperature to 39 degrees. When the disease occurs, the appearance of fever or chills is diagnosed. Patients complain of severe pain in the affected area.
Patients experience hyperhidrosis, which is accompanied by increased sweating. In acute myelitis, patients experience weakness and increased fatigue even when performing usual activities.
If the pathology is not treated in a timely manner, sensitivity in the limbs is impaired. In this case, an arm or leg may succumb to paresis and paralysis depending on the area of damage to the spinal cord. With infectious myelitis, the most serious motor dysfunctions occur. A common symptom of the pathology is increased muscle tone.
During the course of the disease, it is impossible to perform mechanical functions. With radiation myelitis, patients experience a decrease in muscle strength. With a long course of the disease, dysfunction of the pelvic organs is diagnosed.
Only a doctor knows thoroughly what myelitis is and how it manifests itself. Therefore, if you suspect a disease, you should consult a doctor.
Prevention
Currently, people are being vaccinated, which protects them from infectious pathologies that affect the membranes of the brain and spinal cord:
- poliomyelitis – infection of the motor function of the cervical spine;
- measles is a disease whose symptoms are a rash in the mouth and skin, cough;
- Mumps is a virus that affects the salivary glands.
All other causes of the disease are difficult to predict and impossible to prevent. The most important thing is to be attentive to your own health; if something bothers you, you need to seek help from doctors in a timely manner and not self-medicate.
We looked at the symptoms and treatment of spinal cord inflammation.