Peripheral polyneuropathy develops due to damage to the peripheral nerves. At first, patients do not pay attention to the burning sensation in their arms and legs. Polyneuropathy progresses, other symptoms of damage to the peripheral nervous system develop, and the patient’s quality of life is disrupted. In order to prescribe adequate treatment, doctors at the Yusupov Hospital use modern research methods to determine the cause of the disease.
To treat peripheral polyneuropathy, neurologists use medications that are highly effective and have minimal side effects. Severe cases of the disease are discussed at a meeting of the expert council with the participation of professors and doctors of the highest category. Leading specialists in the field of treatment of diseases of the peripheral system collectively make decisions regarding the management tactics of patients with severe forms of peripheral polyneuropathies.
Causes and types of peripheral polyneuropathies
Peripheral polyneuropathy can develop due to many reasons:
- poisoning;
- nerve injuries;
- tumors;
- immunity disorders;
- lack of vitamins;
- alcoholic illness;
- problems with blood vessels;
- vasculitis;
- blood diseases;
- metabolic disorders.
Peripheral nerves are affected by the pathological process due to endocrine pathology, viral and bacterial infections, and the consumption of certain medications. Polyneuropathy can develop due to family history and in cancer patients. Often doctors cannot determine the cause of the disease.
Polyneuropathy can be toxic, vascular, infectious, somatogenic (appearing due to malfunctions of internal organs), autoimmune and hereditary. The following types of polyneuropathies are also distinguished:
- acute inflammatory demyelinating polyneuropathy (Guillain-Barré syndrome) - develops as a result of damage to nerve fibers by autoimmune antibodies;
- Serum polyneuropathy – occurs when antitetanus or antirabies serum is administered;
- diphtheria polyneuropathy – provoked by the diphtheria bacillus and its toxins;
- autonomic polyneuropathy – occurs mainly due to intoxication with carbon monoxide, hydrogen sulfide, manganese;
- uremic polyneuropathy – develops in chronic renal failure;
- paraneoplastic polyneuropathy – formed in patients with malignant neoplasms;
- diabetic polyneuropathy - occurs in 70% of patients who suffer from type 1 diabetes.
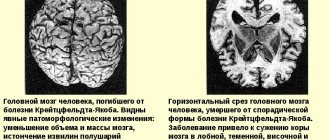
When the nature of the disease is unclear, doctors talk about idiopathic polyneuropathy. Based on morphological characteristics, two forms of peripheral nerve damage are distinguished: myelinopathy and axonopathy. Clinical manifestations of axonopathies and myelinopathies differ in the speed of muscle involvement in the pathological process, the course of the process, and the characteristics of the involvement of sensory, motor and autonomic fibers in the process. Certain forms of peripheral polyneuropathy have specific clinical symptoms that neurologists take into account when making an etiological diagnosis.
Peripheral nervous system disorders: facial neuritis
Neuritis of the oculomotor nerve. The disease is predominantly of vascular, inflammatory, diabetic origin. Observed in intracranial tumors.
Such peripheral neuritis is manifested by drooping of the upper eyelid (ptosis), dilation of the pupil (mydriasis), divergent strabismus and double vision (diplopia).
Treatment according to the etiology of the disease, vitamin therapy, biostimulants.
Neuropathy (neuritis) of the facial nerve . Lesions of other cranial nerves are more common.
The cause of the disease can be hypothermia, infection, trauma, inflammation of the ear or meninges, tumors of the base of the skull. Since the trunk of the facial nerve passes through a narrow bone canal and its terminal branches are located superficially, the nerve is easily injured, and during inflammatory processes tissue swelling develops, which leads to compression of the nerve and the vessels that supply it.
This peripheral nerve neuritis develops acutely or subacutely. There are peripheral and central facial palsy.
Peripheral paralysis is characterized by facial asymmetry - the face is skewed towards the healthy side. On the affected side, the skin folds are smoothed, the eye does not close (lagophthalmos), when trying to close the eye, the eyeball turns up (Bell's sign), food gets stuck behind the cheek, teeth are grinned more in the healthy direction. Dry eyes or watery eyes, disturbances in hearing, taste and salivation may occur.
With central paralysis, only smoothness of the nasolabial fold and drooping of the corner of the mouth are observed.
A complication of this disease of the peripheral nerves can be persistent contracture of the affected muscles and tonic muscle spasm - facial hemispasm.
Diagnosis is based on clinical data and to clarify the diagnosis, an LOP examination, skull radiography, and computed tomography are sometimes performed.
Treatment of this disease of the peripheral nervous system should begin early and be appropriate to the cause of the lesion. For infectious-inflammatory origin, salicylates, methenamine, indomethacin, acyclovir, and prednisolone are prescribed.
In parallel with the etiological treatment, vasodilators are prescribed: dibazol, aminophylline, trental, nicotinic acid, decongestants (Lasix, furosemide, hypothiazide), B vitamins:
The method of “triple” anti-inflammatory infusion therapy is used (parallel intravenous administration of methylprednisolone, rheopolyglucin and trental):
From 5-7 days of illness, thermal procedures (UHF, paraffin, ozokerite) are prescribed.
In the recovery period, prozerin, aloe, FiBS, ultrasound with hydrocortisone are used on the mastoid process and the affected half of the face, electrical stimulation of the facial muscles, exercise therapy, gentle massage, acupuncture.
If there is no effect within 12 months, they resort to neurosurgical intervention.
Care consists of instilling moisturizing eye drops and wearing glasses during the day. At night, apply eye ointment and cover your eyes with a bandage.
Prevention: avoid hypothermia, anti-epidemic measures.
Symptoms and diagnosis of polyneuropathy
The main signs of peripheral polyneuropathy are:
- burning sensation, changes in sensitivity, weakness in the arms and legs;
- atrophy of the muscles of the limbs;
- decrease or loss of reflexes;
- peripheral paralysis.
With polyneuropathy, symptoms of the disease first appear on the tips of the hands and fingers or in the feet. They gradually move up the legs and arms to the limbs. In advanced cases of polyneuropathy, both arms and legs are immediately affected. The symptoms of peripheral polyneuropathy are based on three types of disorders: sensory, motor and autonomic. Depending on the causes and mechanism of development of the disease, the clinical picture may be dominated by symptoms of a certain group or a combination of them.
Sensitive (sensory) manifestations accompany toxic or metabolic subtypes of polyneuropathy. They can be positive and negative. Positive signs include:
- burning;
- severe pain syndrome;
- heightened perception of pain;
- paresthesia (feeling of “goosebumps” on the skin or numbness of a certain area);
- increased sensitivity to tactile stimuli;
- Sensitive (sensitive) ataxia, which manifests itself as unsteadiness when walking, is significantly worsened in the dark and with the eyes closed.
Negative sensory symptoms of peripheral polyneuropathy include decreased sensation in the lower abdomen and fingers. Such signs of the disease are characteristic of inflammatory demyelinating and paraneoplastic polyneuropathy. They can occur with an acute lack of vitamins B12 and E.
Movement disorders manifest as weakness in the limbs. It usually starts from the feet. Often the muscles of the pharynx and head, neck and upper body are involved in the pathological process. Sometimes both upper limbs are paralyzed. This group of symptoms includes muscle twitching, painful cramps, and restless leg syndrome.
The cause of autonomic manifestations of peripheral polyneuropathy is damage to autonomic fibers. Visceral or organ symptoms include:
- fixed pulse;
- pre-fainting states;
- decrease in blood pressure when moving from a horizontal position to a vertical position;
- violation of potency and regulation of sphincters;
- motility disorders of the digestive organs;
- disorders of the respiratory system, sweating and thermoregulation.
Vegetative-vascular symptoms of polyneuropathy include a decrease in the temperature of the skin of the feet and hands, marbled coloration and swelling of these areas. Vegetative-trophic disorders are represented by deformation of nails and fingers, trophic damage to joints, thinning of the skin and the formation of ulcers.
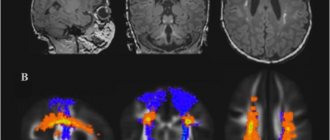
Doctors at the Yusupov Hospital conduct a neurological examination of patients with suspected peripheral polyneuropathy. The neurologist determines the need for further research - electroneuromyography and sensory testing. If indicated, a spinal tap is performed and a cerebrospinal fluid analysis is performed. It can detect antibodies that damage peripheral nerves.
Testing blood glucose levels helps identify diabetes. Doctors use blood tests to determine vitamin deficiencies, kidney failure, metabolic disorders and immune system function. Muscle strength tests can look for signs of seizure activity or motor neuron damage. Assessing the ability to sense vibration, soft touch, body position, temperature and pain sensitivity helps doctors determine damage to sensory structures.
The diagnosis is confirmed using instrumental techniques:
- computed tomography;
- magnetic resonance imaging;
- neuroelectromyography;
- nerve or skin biopsy.
Classification
According to the method of injury there are:
- Compressed (compression) - injury is a consequence of prolonged pressure of great force.
- Bruise (concussion) – injury is a consequence of short-term exposure to a large explosive force.
- Anatomical break can be complete (the integrity of the peripheral nervous tissue is completely damaged, the possibility of recovery without surgical intervention is excluded) and partial (the integrity of the nervous tissue is not completely broken, in some cases it is restored without additional treatment).
In addition, depending on the nature of the damage, there are:
- Open (stabbed, torn, cut and gunshot) - lead to complete rupture of the damaged nerve, in some cases they can be complicated by an associated infection.
- Closed (dislocations, fractures, concussions, contusions and bruises) - lead to partial rupture of the damaged nerve, are best treated.
Based on the time elapsed after injury, the following are distinguished:
- Acute period (lasts up to thirty days from the moment of injury). During this period, degenerative changes increase. Due to certain laws of physiology, it is impossible to assess the severity of the lesion during this period. In the acute period (for open injuries), most surgical interventions are performed.
- Early period (lasts from thirty to one hundred days from the moment of injury). It is characterized by the highest rate of restoration of affected structures. During this period, the degree of damage is determined, as well as its type, level and extent. In the early period, the attending physician, together with the neurosurgeon, determines the treatment tactics and the scope of surgical intervention (if conservative therapy is not effective).
- Intermediate period (from ninety to one hundred and eighty days from the date of injury). The rate of regeneration decreases, in addition, the diastasis of the ends of the nervous tissue that appears after injury increases. Carrying out reconstructive operations during this period is impractical, due to the complexity of the necessary reconstructive techniques and their low effectiveness.
- Late period (from six months to five years after the moment of injury). Due to the almost complete loss of the ability of damaged nerve tissue to regenerate and a significant increase in negative changes, the use of reconstructive surgery is inappropriate.
- Residual period (more than five years from the moment of damage). Full or partial restoration of the damaged nerve is impossible during this period. To alleviate the condition, orthopedic tendon-muscular surgery techniques are used.
Treatment of polyneuropathy
The basis of treatment for peripheral polyneuropathy is drug therapy. Doctors at the neurology clinic prescribe medications to patients that are highly effective and have minimal side effects. Complex therapy of polyneuropathies includes physiotherapeutic methods of treatment. When paresis develops, rehabilitation clinic specialists use modern techniques to restore motor function.
Neurologists determine the cause of peripheral nerve pathology and carry out therapy for the underlying disease. Patients are advised by a geneticist, cardiologist, and endocrinologist. Neurologists at the Yusupov Hospital adhere to European and American recommendations for the treatment of peripheral polyneuropathy:
- treat the provoking disease;
- ensure cessation of interaction with toxins and allergens;
- prescribe symptomatic therapy, vitamins, medications that improve the functioning of the nervous system;
- provide orthopedic care.
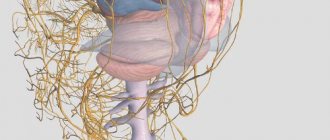
Device
The PNS is structured as a huge number of sensors and neural cables conducting electrical signals through which impulses reach the central nervous system. All of them consist of nerve cells and their processes, folding into individual nerves, which, in turn, are connected into bundles and larger nerve fibers leading to the spinal cord or directly to the brain.
The central peripheral nerves leading to the brain are called cranial and number 12 pairs. All of them are attached to a special organ called the pons and located in the center of the main structure of the human nervous system.
There are slightly more spinal nerves:
- 1 fused pair leads to the coccygeal region.
- 5 to the sacrum.
- 5 pairs in the lumbar region.
- 12 in the chest and 8 in the cervical
All of them are attached to the spinal cord using nerve roots, which are segments consisting of axons that receive signals from the spinal cord, processes that transmit signals to the spinal cord, as well as motor and sensory centers.
The peripheral nerves themselves consist of autonomic and somatic nerves. The latter are conductors of signals from receptors to the central nervous system or orders from the central nervous system to muscles, and autonomic ones, responsible for the unconscious functioning of the body, in turn, are divided into three subgroups:
- Sympathetic, responsible for stimulating the functioning of organs.
- Parasympathetic, on the contrary, is calming.
- Metasympathetic, a subsystem relatively free from the control of the central nervous system, since it is represented by separate complexes of nerve cells that do not report to it and do not influence it, stimulating the automatic contractile activity of hollow internal organs: heart, lungs, bladder, etc.