Brain tissue consists of gray and white matter. Gray matter is nerve cells, white matter is their processes. The spinal cord, whose total length is about 45 cm, is a regulator of the functionality of all internal organs, which carries out its work through the transmission of nerve impulses.
Diseases of the brain and spinal cord cause disorders that are similar in their manifestations: sensory, motor and autonomic.
Mild disorders
In case of mild disorders (mainly paresis rather than plegia) that cause impairment of the functionality of only one limb, walking is possible. In such cases, the affected leg becomes weak and cannot push off the ground. If the lower segments of the spinal cord are damaged (for example, due to compression by an intervertebral disc due to a herniation), walking either on tiptoes or on heels is impossible. If the high spinal regions are affected, knee tone is impaired, the person can neither climb stairs nor stand on a chair.
Severe disorders
More severe disorders affect the pathways in the spinal nerve, whose job is to send signals from the brain to move the limbs. Typical manifestations are spastic paresis or plegia, impaired tone of the limb, its rigidity and the impossibility of passive movement. If only one leg is affected, it is difficult for a person to push off the floor, and bending the knee is also problematic.
Paresis can also be caused by brain injury, tumor, or inflammation.
Spinal cord tumors
Spinal tumors are the least common group in oncology; in most cases they are benign. On the other hand, they can be very dangerous due to their growth close to the spinal cord and associated anatomical structures.
Causes
Most often, the causes of spinal cord tumors are unclear and represent an interaction of genetic predispositions and environmental influences. Sometimes multiple occurrences of some tumors are part of certain genetic syndromes originally related to other organs (eg, neurofibromatosis, Hippel-Lindau syndrome).
Types of tumors
Spinal tumors can originate either from your own tissue or from surrounding tissue. They are largely similar to brain tumors (ependymomas, meningiomas, astrocytomas, and rarely oligodendrogliomas). In the spinal region, neurofibromas arise, developing from the nerve sheaths emerging from the spinal cord.
Metastases of various malignant tumors that affect the spine can also grow into the spinal canal area. The consequences may resemble primary spinal tumors.
Manifestations
Symptoms of damage to the spinal cord of oncological etiology may not initially appear, but as the tumor grows, they begin to narrow the spinal canal, depress the spinal cord, disrupt the function of the nerves leaving the spinal cord, and damage surrounding tissues.
Manifestations include:
- back pain radiating to the limbs;
- muscle weakness;
- movement disorders;
- impaired sensitivity of some parts of the body.
An unpleasant sign of damage to the lower part of the spinal cord is dysfunction of the sphincters, causing fecal and urinary incontinence, and impaired sexual function.
If the tumor grows from the spinal roots in the lumbar canal below the lower spinal end, symptoms of Cauda syndrome may occur.
Diagnostics
When problems arise, a person is usually examined by a neurologist, who determines the presence of physical dysfunction of the spinal cord in a specific area. The patient is referred to have this area examined using some imaging techniques such as CT or MRI. For tumors that spread into the cerebrospinal fluid, its cytological examination is performed using a lumbar puncture.
Treatment
The basis of treatment for spinal cord tumors is their surgical removal. But due to the location of the lesions, very complex neurosurgical procedures are often required, with a high risk of complications and permanent consequences. Other forms of treatment for some tumors are radiation therapy and chemotherapy.
Symptoms of traumatic toxicosis. The concept of trauma (traumatic toxicosis) is complex
Traumatic toxicosis occurs when the soft tissues of the extremities are compressed for a long time (4-8 hours). In most cases, it affects people who were under rubble after the collapse of buildings or earthquakes; it is often encountered by survivors of bombings or train accidents. I will explain the concept of the term itself in the article.
Symptoms
They appear within a short period, a few hours after the pressure on the arms or legs is released. Symptoms appear like this:
- Pale or bluish color;
- There is no pulse in the freed limb;
- Movement is impossible;
- Loss of sensation.
After just 3-5 hours, symptoms of severe shock appear, the functioning of the central nervous system is disrupted, a person develops a feeling of fear and overexcitation, and then apathy sets in. The liver and kidneys are damaged, and plasmarea appears. In some particularly difficult cases, hematuria and oliguria, anuria and protein in urine may appear, and injured arms or legs swell greatly after 3-5 days and paralysis develops.
Periods of traumatic toxicosis
There are 3 periods (early, intermediate and late). The first is characterized by an increase in swelling of the injured tissue and begins after 2-3 days.
At this time, the pulse in the damaged limbs and sensitivity disappear, they turn pale, and the patient develops a state of shock, the heartbeat quickens and the pressure drops. Also, the volume of urine excreted is greatly reduced to 50−250 ml. in a day.
During the second period, which lasts from days 3 to 9, the victim’s well-being becomes better, swelling decreases, and pain subsides. Blood pressure returns to normal, but with all this, kidney damage only increases. The transition to the appearance of complete anuria begins, even fatal uremia is possible.
The third period begins at 9 or 12 days, swelling subsides, sensitivity is restored. In general, local symptoms begin to predominate, but the pain begins to intensify. It happens that pieces of muscle that have died are torn away, and urine begins to be released normally.
The main tasks for eliminating traumatic toxicosis
There are only two of them, but this should be taken very seriously. First of all, to eliminate long-term compression syndrome you need to:
- Reduce muscle necrosis;
- Reduce intoxication;
To achieve this there are certain methods:
- First, you need to cool the injured limb with ice, this will reduce swelling, then you need to cut the skin and fascia, this will significantly reduce compression. In the most difficult cases, in order to save the victim’s life, a limb has to be amputated.
- To prevent shock, bromides are required, usually hydrochloride, atropine and glucose, and novocaine blockade and oxygen are also used.
- The next action that needs to be taken is to restore the reserve alkalinity of the blood. To do this, 20-25 grams of soda are administered intravenously. and 3 l. sodium chloride solution, the patient is prescribed to drink large amounts of fluid.
- Diuretics are prescribed.
- The main method to combat intoxication is extracorporeal detoxification.
From the very beginning, in order to reduce endotoxicosis, it is necessary to carry out regional perfusion of the affected limb, this is done under a tourniquet. Then, without wasting time, hemodialysis is performed to eliminate acute renal failure. In addition, a patient diagnosed with traumatic toxicosis suffers from an acute form of liver failure. To do this, plasmasorption, hemosorption and plasmapheresis are performed.
The importance of early treatment
The initial and intermediate stages of therapy are the most important; a lot depends on them. First, doctors assess the severity of the patient’s injury and how much muscle tissue has been damaged. Then the amount of myoglobin in the blood is determined, and the amount of free hemoglobin, potassium, magnesium, creatine and creatine phosphokinase is determined. The effect will be many times better if you start treatment as early as possible. If detoxification therapy is started late, the patient will not be saved from uremia. In case of severe crushing of muscle tissues, which are sources of toxic substances, a myomectomy or strip opening is performed. At a later stage, therapy is carried out, wound suppuration - necrectomy; these methods perfectly help restore damaged arms or legs.
One of the important factors for the successful recovery of the patient is carrying out general strengthening treatment; taking vitamins and minerals along with proper nutrition will help the body quickly recover. By browsing the site you can find out all the necessary information about nursing, care, and manipulation.
Vascular diseases of the spinal cord
Vascular diseases of the brain and spinal cord are caused by a disorder that leads to a decrease in oxygen saturation of the spinal cord and brain and, as a consequence, to disruption of the metabolism of neuroglial populations.
Hemorrhages are less common, but prognostically they are a very serious group of cerebrovascular diseases. Doctors encounter bleeding more often in patients taking anticoagulants or antiplatelet agents, people with coagulopathy or amyloid angiopathy.
Causes
Local reasons:
- developmental pathologies;
- arteriosclerosis of the afferent vessels or fibrosis of the arteries of the brain or spinal cord;
- inflammatory vascular diseases (syphilis, herpes zoster, borreliosis);
- aortic surgery (aneurysm, dissection);
- spontaneous dissection of the aortic wall due to thinning;
- vasculitis;
- trauma (often along with cervical myelopathy);
- embolism (spontaneous, iatrogenic);
- spinal angiography;
- post-radiation damage to the vascular wall;
- inflammation caused by bacteria and viruses.
Common reasons:
- hypoxia (including in newborns);
- hypoperfusion;
- heart failure;
- hypovolemia (absolute or relative);
- venous infections of the spinal cord that occur with sepsis and malignant tumors.
The causes of bleeding into the spinal canal are different. The most common vascular malformations (venous angiomas, AV anomalies) are formed by unevenly distributed vessels in the spinal cord and leptomeningeal space with the most common localization in the Th-L junction.
Manifestations
Each spinal cord pathology has its own typical manifestations.
Intermittent spinal cord insufficiency is characterized by repeated reversible ischemic symptoms (paraparesis, pyramidal phenomena, paresthesia of the lower extremities, sensitivity disorders, etc.). When signs appear when walking, most often in older people, we are talking about intermittent claudication:
- disorders in the cervical spine - attacks of falling;
- lesions in the lumbar region - spinal claudication (weakness of the lower extremities during physical activity, disappearing at rest).
Initially intermittent symptoms of a circulatory disorder may eventually lead to permanent problems.
In myelomalacia with long-term damage, the clinical picture is varied and corresponds to a focal disorder, both in the vertical and horizontal directions. Transverse ischemia damage can be divided into several syndromes according to blood supply.
Hematomyelia:
- back pain in combination with radicular symptoms;
- incomplete transverse lesion syndrome;
- dissociated sensitivity disorder in the affected segment, distal spasticity;
- Brown-Sequard syndrome.
Epidural hematoma:
- severe back pain, sometimes radiating to the pelvic area;
- paraparesis of the lower extremities;
- sphincter disorders.
Spinal ischemia:
- severe local pain;
- meningeal symptoms.
In cysts, fistulas, and malfomations, the signs are most often localized in the Th-L junction. They usually appear suddenly, less often - slowly, gradually. Initially, local or radicular pain occurs. Often, already in the early stages of the disease, urination disorder occurs, which can be used as part of the differential diagnosis for tumors or other compressions.
Often the course of diseases fluctuates with more or less complete remissions.
Diagnostics
In the case of sudden paraparesis or tetraparesis of the lower extremities, it is first necessary to exclude other causes known in neurology, in particular the expansion process leading to compression of the spinal cord (tumor, hernia, hemorrhage, etc.). These conditions would require urgent neurosurgery.
Diagnostic methods:
- MRI;
- biochemical examination;
- CT angiography of the aorta (excluding dissection or other pathology, for example, thrombotic aneurysm, etc.);
- spinal angiography (detection of malformation);
- study of biomarkers (if myelitis, Guillain-Barré syndrome and multiple sclerosis are suspected).
Treatment
Treatment of spinal cord ischemia is similar to that of ischemic stroke. In patients who have experienced a bleeding episode due to a vascular malformation, an aneurysm, there is a need to choose between interventional radiology and thromboticization of the bleeding source or a surgical solution.
Spinal surgery can be difficult and risky. The doctor must warn the patient about the possible consequences.
Symptoms of traumatic shock stage of excitation. Classification
According to the etiology (reason), traumatic shock occurs:
- As a result of mechanical injuries (fractures, severe injuries, tissue compression).
- As a result of burns.
- From exposure to low temperatures.
- As a result of exposure to electricity.
By time of occurrence:
- Primary - develops immediately after injury (1-2 hours) and is the result of injury.
- Secondary - appears after 5-24 hours as a result of additional trauma.
If we consider the clinical stages of traumatic shock, then two phases are distinguished:
- Erectile phase. In case of injury, impulses entering the central nervous system cause short-term excitation.
- Torpid phase. Short-term excitation is replaced by inhibition and true shock develops with inhibition of all functions. Hemodynamic disturbances prevail - a drop in arterial and venous pressure, a decrease in cardiac output, impaired gas exchange in tissues and metabolic disorders. As a result of circulatory and respiratory hypoxia, all organs suffer.
True shock is classified according to the severity of its manifestations. The following degrees of traumatic shock are distinguished:
- First degree (this is compensated shock). The victim is a little lethargic, the skin is pale, the extremities may be cold, breathing and cardiac activity are increased. Tachycardia up to 100 beats. Systolic pressure 100-90 mmHg. Art.
- Second degree (or subcompensated shock). The victim is slow and does not move. There is pallor and coldness of the skin, as well as a marbled pattern of the skin. Heart rate increases to 110-120, and pressure decreases to 80-75 mm Hg. Art. There is also a decrease in diuresis. The first two degrees have a favorable outcome, since protective-adaptive reactions and assistance prevent the development of cell hypoxia and deepening of shock.
- Third degree (decompensation). As a result of prolonged spasm of small vessels, hypoxia and cell damage occurs when assistance is delayed. The patient is lethargic, does not respond to external stimuli, and has an earthy-colored skin. Heart rate increases even more (130-140 beats), pressure progressively decreases (60 mm Hg and below), and diastolic pressure is often not determined. The patient develops anuria. This condition is typical for prolonged (hours) traumatic shock. However, properly performed resuscitation measures are often effective and the patient is brought out of shock. However, after removing patients from this state, 70% develop severe complications, the treatment of which is more complex than recovery from shock.
- Fourth degree (terminal, irreversible). Changes in the body reach the point where all measures taken are unsuccessful. Destructive processes in the body continue, deep decompensation of homeostasis is noted and the victim dies.
Spinal cord injuries
Traumatic injury to the spinal cord or spine (ICD-10 code – S14) is the collective name for destructive changes that cause a temporary or permanent change in its function. In particular, the motor, sensory, and autonomic functions of the body that use the spinal cord below the site of the lesion change.
Spinal cord injury is one of the most serious injuries and is often associated with permanent physical and psychological consequences. Contusions leading to damage to the spine occur mainly in road accidents and winter sports.
Causes
70% of severe spinal injuries are associated with a car accident. Damage can occur at different levels and be associated with other injuries, such as damage to the head, chest, abdomen, and limbs.
Often similar injuries occur to passengers in the rear seats who are not wearing seat belts. Damage to the spine and spinal cord today also occurs during sports activities, both at the highest and amateur levels. Risky sports include alpine skiing, snowboarding, hockey, and ice skating.
Mostly such lesions occur as single injuries. Another rare group of spinal cord injuries is industrial injuries, especially falls from a height or being crushed by a heavy load.
Other causes include falls (especially in people aged 45+ years), accidents (eg jumping into shallow water), sports injuries and criminal offences. The following causes include vascular and vertebrogenic diseases, tumors, inflammation, multiple sclerosis, infectious diseases, congenital and degenerative pathologies.
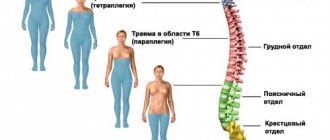
Characteristics of damage
There are 2 main groups based on the height of the lesion: paraplegia and tetraplegia. When a spinal cord injury occurs in the thoracic or lumbar spine, it is referred to as paraplegia. Paraplegia has varying degrees of severity of impaired mobility of the trunk and lower extremities. Since the person has intact impulse in the upper extremities, he can be completely independent, able to perform normal work in a reasonably adapted environment (no stairs, wide doors, sufficient space in the bathroom, etc.).
If the spinal lesion is in the lumbar region, then the mobility of the lower extremities can be partially preserved, and the person can walk with various aids.
With damage at the neck level, the mobility of the lower extremities, torso and, to varying degrees, the upper extremities is impaired. In this case we are talking about tetraplegia. Such extensive damage with deficits in movement of the upper limbs does not allow complete independence; the patient with tetraplegia depends on the help of another person.
It is important to distinguish whether complete or partial damage has occurred. With partial (incomplete) impairment, muscle activity to varying degrees can be maintained below the level of the lesion, neurological and functional prognosis is more favorable.
Of the total number of spinal cord injuries, almost 50% of cases are lesions in the cervical spine.
Post-traumatic state
Damage to the spinal cord means not only loss of mobility of the limbs with the subsequent vital need for a wheelchair, but also impaired sensitivity below the lesion, disorder of reflexes, urination, and sexual function. When the autonomic nervous system is damaged, control of blood pressure and body temperature occurs. The list of serious complications does not end there.
Immediately after injury, there is a significant risk of pressure ulcers, so it is necessary to position the patient alternately on the sides and back. Positioning is carried out after 3 hours.
Another common complication, especially in patients with lesions in the neck or upper chest, is difficulty breathing, increasing the risk of developing a respiratory infection.
The third main group of complications is urinary tract infections. A person, as a rule, becomes ill when a urinary catheter is installed for a long time or when alternative methods of emptying the bladder are used if spontaneous urination is not possible. These complications may occur in the early post-traumatic period but often occur several years after the injury.
There are several factors that can influence a person's post-traumatic state. First of all, this is the type of injury and the degree of damage to the nerve structures (primary injury). Immediately after the injury, swelling of the spinal cord develops at the site of pressure of a possible fracture and bleeding (secondary injury).
At this stage, the consequences of damage can be mitigated. Success depends on proper therapy and early surgery aimed at restoring the width of the spinal canal and relaxing the nerve structures. Immediately after spondylosurgery, intensive rehabilitation begins. Only after a few months can the final functional state be assessed (according to the course).
Types of Injuries
Types of injuries can be assessed by the status of a number of functions, such as:
- motor functions (paresis, plegia);
- sensitive functions (quantitative - dysesthesia, hypoesthesia; qualitative - superficial and deep sensations, dissociated disorders);
- sphincter disorders (urinary retention and incontinence);
- autonomic disorders (hypertension, pulsatile cephalea, increased sweating, piloerection, hyperemia);
- impaired cardiac function (arrhythmia, supraventricular extrasystole, bradycardia, atrioventricular conduction disorder).
Spinal lesions are divided into several groups depending on the type of functional disorder:
- Commotion. A disorder caused by edema or transient ischemia that lasts for several hours. Plegia is corrected within 24 hours.
- Contusion. Structural damage to the spinal cord directly resulting from trauma or bleeding.
- Whiplash syndrome. Caused by a collision with the rear of a vehicle, injury to the cervical spine due to severe flexion and subsequent stretching. The victim may have a constant headache with pain radiating to the upper extremities. Autonomic disorders and dizziness are also present.
- Hematomyelia. Bleeding causing intramedullary lesions.
- Brown-Secard syndrome. Hemisection (half deformation) of the spinal cord to the right or left. Occurs due to penetrating trauma, extramedullary tumors, bleeding, ischemia, inflammation, or iatrogenic causes. Has a relatively good prognosis.
- Compression. Motor dysfunction and sensory disturbance occur.
- Intramedullary lesions (mainly in the cervical region). It is characterized by a movement disorder that is more pronounced in the upper extremities.
- Transverse lesions of the spinal cord. Paraplegia or quadruplegia, urinary retention, spinal shock, and bradycardia are present. Priapism occurs in men. The shock lasts 2-3 weeks. At this time, muscle atony, areflexia, and then central paresis (spasticity and hyperreflexia) occur distal to the lesion. When the cervical spine is injured, paralysis occurs and respiratory failure poses a life-threatening condition. Paralysis over C3 immediately causes respiratory arrest.
After 24 hours of duration of the lesion, the absence of signs of improvement indicates a high probability of lifelong persistence of this condition.
Diagnostics
The following methods are used in diagnosis:
- 3 x-ray projections (antero-posterior, lateral, transoral);
- CT (axial slices, other planes, three-dimensional visualization);
- MRI (recommended if soft tissue damage is suspected);
- electromyography;
- somatosensory evoked potentials;
- motor evoked potentials.
Treatment
ABC (Airways, Breathing, Circulation) principles are applied in therapy, including addressing possible shock.
Methylprednisolone is sometimes given at a dose of 30 mg/kg followed by 5.4 mg/kg over 23 hours or 48 hours (if the initial dose is given 3+ hours after injury).
There is currently insufficient evidence to support the effect of methylprednisolone in patients with complete spinal cord lesions. On the other hand, the associated complications associated with its use are significant and its use is recommended in extreme cases.
A urinary catheter needs to be installed. The spine is also secured and transported in a stable position to a trauma, neurosurgical or orthopedic department, where residual stabilization and decompression are performed.
Prevention
Injury prevention is based on compliance with road safety, control of the intake of addictive substances (drugs and medications), refusal to drive a vehicle when tired, and driver concentration on driving (child in the car, telephone conversations, etc.). Another point is the use of protective devices (reflective materials, airbags, seat belts, child seats). Prevention also includes the area of education, such as awareness of the dangers of jumping into water of unknown depth, lack of safety locks on firearms.
SENSITIVITY DISORDERS. PAIN
Neurogenic disorders of any sensitivity are based on damage to the somatosensory analyzer.
All types of sensitivity are formed by irritation of receptors in the skin, mucous membranes, muscles, joints and tendons, about which information is transmitted to the central nervous system.
Forms of sensitivity disorders. Depending on the type of sensitivity disorders, the following are distinguished:
- disorder of contact types of sensitivity - tactile. pain, temperature when the receptors of the skin and mucous membranes are damaged;
- disorder of distant types of sensitivity - visual, auditory, smell as a result of lesions, respectively, of the ocular or auditory analyzer, the nasal mucosa.
Depending on the disturbance in the perception of the intensity of the sensation, the following are distinguished:
- hypoesthesia - decrease, or anesthesia (complete loss) of sensitivity;
- hyperesthesia - increased sensitivity to the action of a stimulus.
Causes of disturbances in the perception of sensations:
- increased sensitivity of receptors, which is observed with damage or diseases of the skin and mucous membranes, for example with wounds, burns, herpes zoster, etc. P.;
- increased excitability of neurons in the sensory fields of the cerebral cortex and hippocampus, which is observed in neuroses, some mental disorders, and encephalitis.
Depending on the violation of the adequacy of the sensation to the stimulus that caused it. These disorders are called dysesthesias.
Types of dysesthesias:
- thermalgia - the perception of cold and heat effects as painful;
- polyesthesia - a feeling of the action of many stimuli under the influence of one real factor (for example, a feeling of burning, tingling and pressure when the skin is pricked with a needle);
- allodynia - the perception of non-painful effects as painful;
- hyperpathy - excessive pain that occurs under the influence of various stimuli, including non-painful ones (for example, stroking), combined with a loss of the sense of the exact localization of their action;
- paresthesia - tactile, non-painful, but unusual in nature sensations in the form of a feeling of numbness, stiffness, crawling “goosebumps”, tingling. Occurs without any obvious stimulus.
The most common causes of dysesthesia:
- tissue ischemia;
- tissue cooling;
- pathological processes affecting the dorsal roots of the spinal cord (for example, tabes dorsalis - a late form of neurosyphilis).
Mechanisms of sensitivity disorders. At the receptor level:
- an increase or decrease in the sensitivity threshold of receptors for various reasons;
- an increase or decrease in the number of receptors during ischemia or cell degeneration.
At the level of the conduction pathways - inhibition or complete block of the conduction of the excitation impulse. Develops when damaged:
- nerve trunks - for injuries, intoxications, hypovitaminosis. diabetes mellitus, infections, allergic autoimmune processes;
- dorsal roots and dorsal horns of the spinal cord, which is characterized by pain, paresthesia and is accompanied by a disorder of skin sensitivity of the segmental type in the form of the formation of “strips of disturbances” - circular on the trunk and longitudinal on the limbs:
- lateral columns of the spinal cord, which leads to loss of pain and temperature sensitivity on the side opposite to the site of the lesion.
At the level of the central structures of the sensory system:
- change in the sensitivity threshold of neurons;
- disruption of the formation of sensations during action or in the absence of a stimulus.
Pain is a special type of sensitivity that occurs under the influence of a pathogenic stimulus and is characterized by an unpleasant sensation, as well as, possibly, significant changes in the body, including disruption of vital functions and death.
The meaning of pain: signaling and pathogenic.
Signal: the sensation of pain is caused by various agents that have a real or potential danger of damaging the body. Therefore, the pain signal provides:
- mobilization of the body to protect against a pathogenic agent, activation of phagocytosis, changes in central and peripheral blood circulation, etc. Important is the protective behavioral reaction to pain, aimed either at “escape” from the action of the damaging factor, or at its elimination - withdrawing the hand, removing a foreign object bodies etc. P.;
- restriction of the functions of an organ or the body as a whole: for example, a sharp pain during myocardial infarction is accompanied by a fear of death. This forces the patient to significantly limit physical activity, which in turn significantly reduces the hemodynamic load on the damaged heart.
Pathogenic . Pain is often the cause or component of the pathogenesis of various diseases and painful conditions. For example, pain as a result of injury can cause shock: pain due to inflammation of the nerve trunks causes dysfunction of organs; the development of general reactions of the body - an increase or decrease in blood pressure, dysfunction of the heart, kidneys, lungs and other organs.
Causes. Pain is caused by various factors:
- physical (for example, mechanical injury, high or low temperature, electric current);
- chemical (for example, the effect on the skin or mucous membranes of strong acids, alkalis, accumulation of calcium or potassium salts in the tissue);
- biological (for example, high concentrations of inflammatory mediators - kinins, histamine, serotonin).
Mechanisms of pain formation.
Receptors are free nerve endings capable of perceiving the effects of various agents as pain, as well as specialized pain perception receptors - nociceptors .
Neurochemical mechanisms of nociceptor activation.
Irritants. causing pain, they release a number of substances from damaged cells (they are often called pain mediators) that act on nociceptors. Among these substances, biogenic amines (histamine) are of primary importance.
Conducting pathways:
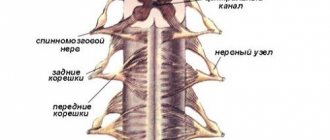
- afferent conductors of pain, penetrate the spinal cord through the dorsal roots and contact the neurons of the dorsal horns;
- spinal cord pathways;
- neurons of the thalamus, hypothalamus, amygdala complex. These structures determine the body’s systemic response to a pain stimulus, including autonomic, motor, emotional and behavioral components.
Central nervous structures.
A holistic sensation of pain is formed by the simultaneous participation of cortical and subcortical structures that perceive pain impulses. In the cerebral cortex, information about pain is selected and targeted “pain behavior” is formed to eliminate the source of pain or reduce its degree.
Clinically, there are three types of pain:
- thalamic pain , which is characterized by transient episodes of severe, debilitating pain and pain combined with autonomic, motor and psycho-emotional disorders;
- phantom pain , which is felt in a missing body part, most often in amputated limbs;
- causalgia is a paroxysmal, intensifying burning pain in the area of damaged nerve trunks, especially the trigeminal, facial, glossopharyngeal and sciatic nerves.
The antinociceptive system is formed by mechanisms that control the feeling of pain, and includes neurogenic and humoral mechanisms. Neurogenic mechanisms are provided by the impulse of special neurons in the brain, which inhibit the flow of ascending pain information to the subcortical and cortical structures. Humoral mechanisms are represented by a number of biochemical systems capable of producing substances that suppress the formation of pain. Neurogenic and humoral mechanisms closely interact with each other and are capable of blocking pain impulses at all levels of the nociceptive system - from receptors to its central structures.
The body's response to pain is manifested by both adaptive and pathogenic changes in the body and includes psycho-emotional, autonomic and motor components.
Psycho-emotional component. The cerebral cortex transforms pain into a painful, unpleasant sensation. Pain is a signal of damage to the body, and therefore the feeling of pain is always of a negative psycho-emotional nature.
Vegetative component. Pain is one of the causes of stress, due to which the nervous and endocrine systems, respiration, blood circulation, immunobiological surveillance system and others are activated, aimed at eliminating the damaging factor.
The motor component includes both an involuntary reaction to a painful stimulus (withdrawal of a limb) and the targeted elimination of a painful factor, such as a hot object.
New research in the treatment of spinal cord lesions
Scientific research into spinal cord diseases and their treatment options continues. The bulk of scientific work is devoted to methods of protecting and restoring the nervous system. This concerns mainly the treatment of secondary problems, the use of drugs against free radicals, apoptosis, and inflammation. Recently there has been a presentation of new cell therapy products, including the use of mesenchymal, neural and induced pluripotent stem cells. The technique has promising but controversial results and uses the growth factors BDNF, NGF and NT-3. The second direction is the use of biomaterials such as nanofibers and hydrogels, but so far without significant results. The third direction is robotic exoskeletons.
Symptoms of traumatic shock. Symptoms of traumatic and hemorrhagic shock
Injured patients are initially agitated, restless, and complain of intense pain in the area of damaged tissue. With severe pathology, depression of the nervous system activity is observed (lethargy, coma). Breathing is frequent and deep; auxiliary muscles are actively involved in it. As the central nervous system is depressed, breathing becomes weakened and shallow. In comatose patients, obstructive breathing disorders may occur (retraction of the tongue, accumulation of sputum and blood in the mouth and throat, and the flow of gastric contents).
The skin of patients becomes bluish in color, and as the shock lasts, it becomes "". This is especially noticeable above the knees and on the hips. With significant blood loss (more than 30% of the blood volume), the skin is pale and moist. Due to impaired microcirculation in patients, peripheral body temperature decreases. The difference between rectal temperature and skin temperature is more than 3 degrees Celsius. A symptom of a “white spot” appears (when you press on the skin, a white spot appears, which normally disappears after 3 s. A significant prolongation of the time of existence of the spot indicates microcirculatory disorders).
Loss of blood and tissue fluid leads to a decrease in the turgor of subcutaneous tissue, the tone of the eyeballs, and the blood supply of the saphenous veins. The pulsation of peripheral arteries is weak; the pulse becomes frequent, soft, thread-like. Blood pressure and central venous pressure decrease. Due to hypotension and compensatory spasm of the renal arteries, renal blood flow (renal perfusion) is reduced. Oliguria develops; the hourly urine output rate is less than 0.5 ml/kg body weight.