What's happened
Neuralgia and neuritis are inflammations of the nerves that occur for various reasons; sometimes inflammation occurs not of the nerves themselves, but of their endings or other parts.
Nerve endings are special tiny formations at the ends of neural processes that are responsible for receiving or transmitting information in the form of electrical nerve impulses.
There are several types of endings according to their area of specialization:
- Synapses that transmit impulses between neurons.
- Receptors or afferent endings that transmit information to a nerve cell from the external environment.
- Effectors – transmitting an information impulse from a neuron to tissue cells.
Inflammation of nerve endings is often called neuritis, when in addition to pain, paralysis, paresis, reduction or loss of sensitivity in the area of responsibility of the damaged area of the nervous system may occur.
Neuritis is a more dangerous disease than neuralgia, since the symptoms of neuralgia are caused only by the influence of something on the nerve, and not by its breakdown. With severe neuritis, which is a disease of the nerves themselves with a violation of their internal structure, the nerve may not recover, as well as the functions it performed.
It would be more correct to consider that inflammation of the nerve endings is a disease that is part of neuritis and its classification, and not directly by it, since with neuritis other parts of nerve cells or nerves can be affected.
What promotes inflammation
A variety of negative factors affecting the body or the nerve itself can contribute to inflammation of nerve endings:
- Drafts and hypothermia.
- Infection of the body with viruses, bacteria or fungi.
- Inflammation of surrounding tissues.
- Muscle spasms or compression of the nerve area.
- Bruises.
- Local infections in the form of an abscess.
- Circulatory disorders.
- Deficiency of certain substances, vitamins or minerals in the body.
- Malfunctions of the endocrine system.
- Toxic poisoning.
- Heredity or individual structural features of the body.
- Tumor processes and many other factors.
More often, inflammation of the nerves begins with prolonged negative irritating effects on the nerve or with infection.
Symptoms and types
The classification of inflammation of the nerve endings is based on the area of nerve damage, as well as their symptoms. There are the following main types, each of which has its own individual manifestations:
- Inflammation of the median nerve, also known as the ulnar, carpal, radial or ulnar nerve, which runs along the arm through the wrist. In this case, the work of the hand is disrupted or sensations arise in it in the form of numbness, tingling, pain or restriction of finger movement. The pain can shoot throughout the entire path of the nerve or be localized only at the site of inflammation.
- Femoral nerve problems, where skin sensitivity or the ability to flex the hip joint are reduced, as well as pain along the surface of the leg, which can shoot down the entire leg.
- Inflammation of the nerve endings of the spine, which is one of the most dangerous types of neuritis and manifests itself in the form of severe pain in the back, chest or neck, depending on the affected area, which is called sciatica. Radiculitis also has its own classification, based on symptoms depending on the area of dislocation: radiculitis of the lumbosacral, cervical or thoracic region.
- Inflammation of the peroneal nerve is pain in the heel or lumbago from it, leading to the inability to fully lean on it.
- Damage to the nerve endings of the facial nerve is represented by disturbances in facial expressions, numbness of parts of the face or unpleasant sensations.
- A disease of the auditory nerve, when in addition to pain, hearing is lost or weakened, and problems with balance or nausea begin due to the fact that the auditory nerve is also responsible for the vestibular apparatus.
- Damage to the intercostal nerve causes more discomfort, since pain can occur not only when moving the body, but when breathing, which makes it difficult or unpleasant. In this case, the pain is truly hellish.
- Inflammation of the optic nerve is accompanied by loss or distortion of vision.
- Damage to the sciatic nerve endings manifests itself in the form of pain in the lower limb and impaired sensitivity and ability to move the leg. There are severe cutting groin and lumbar pains.
- Disease of the nerve endings in the occipital region provokes headaches, pain around the back of the head, pain from touching it, “twitching” of the nerve in the head, a negative reaction to light and lumbago in the ear or lower jaw.
In addition to the above, there are many more types of this disease: exactly as many as there are nerves in the body, each of which can become inflamed; other cases are extremely rare.
The concepts of primary inflammation of nerve endings are used - direct, and secondary, which develops against the background of any disease.
Symptoms
Muscles are divided into several large groups, depending on their anatomical location. Damage to different nerves leads to muscle pain in different parts of the body:
- with pathology of the intercostal nerves, pain occurs in the anterior or posterior part of the chest;
- pathology of the sciatic nerve causes pain in the lower back, buttocks, and legs;
- damage to the cranial nerves leads to pain in the face and scalp;
- Infectious nerve damage, especially herpetic, causes long-term pain in various parts of the body.
Vitamin deficiency, diabetes, alcoholism lead to muscle pain in the legs, loss of sensitivity and impaired nutrition of muscles and skin. The general clinical picture of muscular neuralgia is an attack of pain that suddenly appears and suddenly disappears. Each person can describe the nature of pain in their own way. This will depend on many factors:
- characteristics of the body;
- pain threshold;
- localization of nerve pathology;
- extent of damage;
- cause of damage.
With muscular neuralgia, the symptoms are quite varied, and those that are not directly related to nerve damage can also be observed.
Herpetic damage to nerve fibers has special symptoms. In fact, the pain in this case is not muscular, but it is so strong that the person feels that everything hurts - muscles, skin, sometimes even bones. This intensity of pain is due to the fact that the herpes virus destroys the sheath of the nerve fiber. It takes a very long time to recover, so the pain syndrome can persist for months.
The condition occurs due to damage to the intercostal nerves. The extent of pain will depend on the number of affected nerve fibers - from the neck to the costal arch. The pain is of a girdling nature. The pain syndrome intensifies when changing body position, making movements, or physical activity. When pressing on the intercostal spaces, the pain intensifies.
Painful sensations occur in attacks. Attacks of intercostal neuralgia can last from several hours to several days. They can be combined with sensory disturbances in the form of goosebumps and numbness of the skin. Due to the pain, it becomes difficult for a person to breathe; he spares the painful area of the chest.
If neuralgia is localized in the left half of the chest, it can be confused with an attack of angina or myocardial infarction. Taking nitroglycerin helps differentiate these conditions, which stops angina. To exclude myocardial infarction, electrocardiography is required.
A fairly common pathology in older people. The nature of the pain is usually one-sided. The pain starts from the lower back, covers the tailbone and thigh and can radiate to the popliteal region.
The pain is constant, of moderate intensity. With certain movements, increased pain occurs, called lumbago. In this case, a burning sensation occurs, intensifying with the slightest movement. They weaken when lying down.
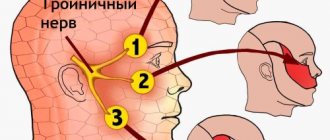
This nerve innervates the skin and muscles of the face. If it is damaged, pain will occur in this area. Pain occurs suddenly, under the influence of so-called trigger factors. They can be overwork, light or sound irritation.
More often the pathology is unilateral. The pain is extremely intense, stabbing in nature. At the same time, numbness of the facial skin and small muscle twitches are observed. The attack lasts no more than ten minutes, then the pain also suddenly stops.
Pain may radiate to the ear or jaw. Often after the attack stops, heaviness in the head, a feeling of pulsation and fullness appears.
Diagnostics
To determine the presence of neuritis, a neurological examination and testing of nerve function using reflexes and testing motor functions, if possible, is performed.
To determine the extent of damage, instrumental examination methods are used:
- Electroneurography is a study of the speed of impulse transmission along a fiber and its conductivity. Allows you to determine the extent and area of damage.
- Electromyography – examines the boelectric activity of muscles and checks the functional state of neurons.
- Evoked potentials are a method similar to electroneuronography, but for deep nerves, such as the optic and auditory, where they are affected by sound or image and the conductivity is recorded by the activity of the corresponding parts of the brain.
- Ultrasound, X-ray, MRI or CT are diagnostic methods designed to identify the physical cause of damage to the nerve and its endings and prescribe the necessary treatment, rather than the disorder itself.
If an infection is suspected, laboratory tests of blood and other tissues are performed, including a biopsy of nerve tissue in extreme cases.
Treatment
Treatment occurs by eliminating the cause of inflammation of the nerve endings, which may require the following procedures:
- Antiviral or antibacterial drug therapy.
- Surgical treatment with compression or physical impact.
- Anti-edematous therapy.
- Stimulation of blood circulation.
- Biogenic stimulation – stimulation of restoration processes with special preparations.
- Anticholinesterase therapy is treatment with drugs that inhibit nervous activity.
- Fortification and replenishment of deficiencies of minerals and other substances.
- Plastic or surgical suturing of the nerve, when a severely damaged area is removed.
- Local administration of drugs directly near the nerve.
- Physiotherapy treatment.
- stimulation of the nerve.
- Symptomatic treatment with anesthetics.
Treatment of inflammation of nerve endings is selected individually and depends on the specific type of neuritis and its location. With this disease, traditional methods selected with the help of a doctor are very helpful.
Symptoms of inflammation of nerve endings
Before starting a diagnosis and prescribing treatment, the patient should describe his symptoms and sensations to the doctor in as much detail as possible. The main sign of inflammation is pain, the source of which cannot always be identified independently. It can get worse at night, with any physical activity, even walking, sometimes in the cold.
The second most characteristic sign indicating that there is inflammation of the nerve endings in the body is a burning and tingling sensation in the affected area. Depending on the area of pathology, pain can occur even with minor skin irritations.
In general, all symptoms depend on the area of the body in which the damage occurs. For example, when the nerve endings of the legs become inflamed, the sensitivity of the foot or lower leg worsens. Often movements in the knee area are severely limited and the slightest change in position causes pain. In case of eye disease, pain makes itself felt when moving the eyeballs, and vision often decreases.
Symptoms of neuritis
The first signs of neuritis:
- Feeling of pain at the site of the inflammatory process;
- Numbness of the innervated area;
- Tingling sensation.
Main symptoms of neuritis:
The main symptoms of neuritis depend on the type of nerve fibers affected - sensory, motor and autonomic, as well as on the cause and severity of the inflammatory process:
Inflammation of sensory fibers causes - paresthesia (decreased sensitivity, running "goose bumps", a feeling of numbness and tingling in the innervation zone), feeling pain.
Inflammation of motor fibers is caused by impaired motor function (paresis - partial, paralysis - complete), weakening and/or atrophy of muscles, decreased or loss of tendon reflexes.
Inflammation of vegetative fibers is caused by local hair loss, skin depigmentation (the appearance of vitiligo), xeroderma, thinning and swelling of the skin, fragility of the nail plate, the appearance of trophic ulcers, increased sweating and others.
Additional symptoms of neuritis
The following symptoms are characteristic of different types of neuritis, and depend mainly on the location of the innervated area/organ/tissue:
Read also Carbuncle - causes, symptoms, photos and treatment of carbuncle
Neuritis of the facial nerve (Bell's palsy) is an inflammation of the nerve responsible for the work of the facial muscles of one half of the face.
Symptoms of facial neuritis are the appearance of weakness in the facial muscles, which manifests itself in the form of partial or complete absence of facial movements, as well as facial asymmetry, similar to the consequences of a stroke. With neuritis of the facial nerve, on the affected side, wrinkles on the forehead are also smoothed out, the eyelid is drooping, and the corner of the mouth is drooping.
Inflammation of the nerve endings of the spine
Very sharp pain is accompanied by damage to the nerves of the spine. Infectious diseases of the spine, osteochondrosis, and severe trauma can lead to inflammation.
Sometimes the back area is sharply pierced by acute pain, which can arise as a result of excessive stress, which often leads to radiculitis. Its main symptom is vertebral neuralgia. Symptoms gradually increase as the spinal disease progresses. Radiculitis also often appears after “advanced” osteochondrosis. It can “settle” in any area of the spine, which leads to constant pain in the back, reminiscent of impulses.
With osteochondrosis, which is the cause of back pain in 90% of cases, a degenerative change in the intervertebral discs occurs. When a disc ruptures, it extends beyond the spinal region. Around it are located blood vessels and nerve endings. If the disc touches them, the person experiences pain.
Among the main diseases of the spine that provoke acute pain are also intervertebral hernia, lumbago, sciatica, scoliosis, and intercostal neuralgia. Of course, this is not the entire list of diseases that can provoke inflammation of nerve endings. Therefore, you should not self-medicate.
In most cases, a warm wool scarf or blanket on the lower back is not enough. Only a doctor can make an accurate diagnosis and prescribe effective treatment to promote a speedy recovery.
Treatment of neuralgia with folk remedies
- pour chopped willow bark (10 g) with boiling water (200 ml);
- simmer over low heat for 20 minutes;
- strain through cheesecloth, drink when cool.
You can treat yourself with an effective mixture at home, which should be used every other day for a month:
- Mix iodine and glycerin in equal proportions in a dark glass bottle.
- Shake the bottle and moisten a clean swab with the solution.
- Lubricate sore areas except the spine area.
- Homemade tincture based on fir cones, dandelions, pine needles - alcohol tinctures with an anti-inflammatory effect are obtained from the listed plant materials. Take 0.5 liters of vodka for a glass of fir cones or dandelions and let the mixture steep. Use as a rub in small quantities before bedtime.
- Warm compress with beeswax. The wax is softened in a steam bath, a warm wax cake is applied to the sore spot, and bandaged with a bandage. The compress can be left overnight.
- Ointment made from dried lilac buds based on pork fat. Grind the dry kidneys into powder and mix with pork fat in a ratio of 1:4. The resulting fat mixture can be used 2 times a day to relieve pain.
Find out more about how to treat intercostal neuralgia at home.
Inflammation of the occipital nerve
Inflammation of the occipital nerve leads to frequent headaches. Pain occurs in the back of the head and radiates to the front and sides of the head. Often, patients describe pain similar to what they experience with migraine. The scalp can also become very sensitive to various types of touch. For example, even when trying to comb your hair, unpleasant painful sensations occur.
By the way, with occipital inflammation of the nerve endings, doctors often encounter some difficulties. They are due to the fact that it is often difficult at this stage to distinguish inflammation from other causes that cause headaches. Therefore, the patient is obliged to describe all the symptoms present in as much detail as possible and honestly answer the doctors’ questions.
If headaches bother you constantly, you should immediately consult a specialist. In this case, taking exclusively painkillers, which the patient chooses at his own discretion at the pharmacy, is not enough. Doctors often conduct complex diagnostics, including computed tomography and magnetic resonance imaging. This is necessary because sometimes secondary occipital neuralgia can be caused by infections, brain tumors, injuries, and lupus.
If the inflammation does not require surgical intervention, the doctor will prescribe treatment aimed at relieving pain. Drug treatment is combined with physiotherapy procedures and massage. In addition, doctors recommend getting more rest. Additionally, a course of anticonvulsants and steroidal anti-inflammatory drugs may be prescribed.
Cases where surgical intervention is required to treat a disease occur less frequently. For chronic pain and lack of positive results from conservative treatment methods, surgery is indicated.
Treatment of inflammation
Sometimes inflammation of the nerve endings is so severe that pain occurs even with the slightest irritation of the skin.
In order for the prescribed treatment to be effective, it is necessary to establish the cause that caused the disease. If all the symptoms indicate that an infection has led to inflammation of the nerve endings, doctors usually prescribe antibiotic injections. Treatment with antiviral drugs is often required.
In case of decreased blood circulation (ischemia), medications are taken that dilate blood vessels and stimulate their function. If symptoms indicate traumatic neuritis, doctors prescribe painkillers and anti-inflammatory medications. Additionally, a course of injections may be prescribed.
When drug treatment comes to an end, the patient may be referred to physical therapy.
Sometimes surgical intervention is required to free the nerve. The need for surgery occurs when there is severe pressure or when the nerve grows in the wrong direction.
Inflammation of nerve endings is often a symptom of serious diseases. Therefore, it is impossible to neglect pain in the area of the sciatic nerve, spine, head or other area of the body. You should immediately consult a doctor to relieve any discomfort. Regular pain is not a reason for self-medication, which can lead to unpleasant consequences. It is important to find the cause of the pathology and eliminate it with the help of a competent doctor.
The nervous system is responsible for sensory, motor activity and the functioning of the endocrine and immune systems in the human body. The development of the inflammatory process in the nerve roots causes pain and limited mobility. It is difficult for a person to move, the sensitivity of joints and soft tissues is impaired. Inflammation of the nerve in the leg, the symptoms of which cause significant discomfort, appears more often as a concomitant pathology against the background of other diseases of the spine or viral damage to the body.
Treatment of neuritis
How to treat neuritis? Treatment of neuritis depends on the type, cause and location of the disease, but usually includes the following points:
1. Treatment of the root cause of the disease, i.e. disease or pathological condition that led to nerve disorders; 2. Drug therapy; 3. Physiotherapy. 4. Surgical treatment.
Treating the root cause of the disease
Accurate and thorough diagnosis for neurological disorders is very important, since treatment directly depends on this point. In addition, it is necessary to exclude secondary diseases.
2. Drug treatment of neuritis (medicines for neuritis)
Important! Before using medications, be sure to consult your doctor!
2.1. Relieving infection
Antibacterial and viral infections are the most common causative agents of various infectious diseases, accompanied by inflammatory processes, intoxication and decreased reactivity of the immune system. And due to the fact that nerve fibers penetrate all parts of the body, it costs nothing for pathological microorganisms to involve the nervous system in the inflammatory process.
Relieving the infection is generally considered more of a point of treating the underlying disease that led to the inflammatory process in the nerve.
Bacterial infections can be treated with antibiotics, while viral infections can be treated with antiviral therapy. In addition, the prescription of a specific antibiotic depends on the type of pathogen.
Read also Gingivitis. Causes, symptoms, types and treatment of gingivitis
Antibiotics for neuritis: against staphylococcal infections - Amoxicillin, Vancomycin, Clarithomycin, Erythromycin, Oxacillin, Cephalexin, against streptococcal infections - Azithromycin, Doxycycline, Levofloxacin, Ceftriaxone ", "Cefotaxime", "Erythromycin".
Sulfonamides – antimicrobial drugs for neuritis: “Sulfanilamide”, “Sulfamoxol”.
Antiviral drugs for neuritis: interferon and its derivatives (Betaferon, Interlock, Laferon, Neovir, Reaferon, as well as gamma globulins.
2.2. Detoxification therapy
The waste products of pathogenic infectious agents in the body cause symptoms of intoxication (poisoning), which causes the patient to experience nausea, sometimes vomiting, a feeling of weakness and general malaise. This is also facilitated by the spread of microbes killed through the body due to the use of antibiotics or antiviral drugs.
To remove dead bacteria, as well as their waste products, detoxification therapy is used, which includes:
- Taking sorbents - “Atoxil”, “Polyphepan”, “Enterosgel”;
- Drink plenty of fluids, preferably with added vitamin C (ascorbic acid);
- The use of diuretics (diuretics) - “Diacarb”, “Furosemide”;
- In case of severe intoxication of the body, intravenous infusion of solutions of glucose, polysaccharides (“dextran”) and water-salt solutions, “Urotropin”.
2.3. Anti-inflammatory therapy
Non-steroidal anti-inflammatory drugs (NSAIDs) and glucocorticoids (hormones) are used to relieve pain, as well as stop the inflammatory process in the nerves.
Among the drugs in the NSAID group are Ibuprofen and Nimesil.
Among glucorticoids one can o.
It is better to relieve high fever in children using water-vinegar based compresses.
For tunnel syndromes, medications are injected directly into the affected canal - “Hydrocortisone”, “Novocaine”.
If the cause of the inflammatory process is a violation of the blood supply to the nerve (ischemia), vasodilating drugs are prescribed - Papaverine, Eufillin.
2.4. Symptomatic treatment
Sedatives are prescribed to reduce the activity of the nervous system, which leads to a reduction or prevention of the development of muscle spasms - “Persen”, “Bekhterev’s Medicine”.
Additional intake of vitamins is required - B vitamins, vitamin E (tocopherol), vitamin C (ascorbic acid), vitamin PP (nicotinic acid), milgama, neurobion, neurorubin. Vitamin therapy is necessary to restore nerve function.
In addition, for neuritis the following can be used:
- Gravity treatment methods;
- Antihistamines;
- Angioprotectors and antiplatelet agents;
- Proteolytic enzyme inhibitors.
Physiotherapeutic treatment
Physiotherapeutic procedures for neuritis include:
- Plasmapheresis;
- Mud applications;
- Massage of the innervated muscles where the inflamed nerve is located;
- Hyperbaric oxygenation;
- Pulse currents;
- Ultraphonophoresis with hydrocortisone;
- UHF;
- Electrophoresis of novocaine, neostigmine and hyaluronidase.
Additionally, electrical stimulation of the affected muscles can be performed.
Special therapeutic exercise (physical therapy) also has a beneficial effect on the body. Exercise therapy (exercises) for neuritis directly depend on the location and type of the inflamed nerve.
The use of physiotherapy is prescribed on the 6-7th day of treatment for neuritis.
Surgery
Surgical treatment of neuritis is used for:
- traumatic etiology of this disease;
- lack of effectiveness of conservative treatment;
- no signs of nerve recovery.
Signs of sciatica
Sciatica is an inflammation of the sciatic nerve, which is one of the largest in the body. It originates in the spinal cord, and its branches pass through the buttocks along the entire lower limb all the way to the toes. The main causes of the disease:
- prolonged hypothermia;
- compression of nerve endings due to displacement of the intervertebral disc;
- mechanical injuries of the lumbar spine;
- heavy physical activity;
- viral, infectious diseases;
- pelvic organ injuries;
- piriformis syndrome;
- osteochondrosis;
- bone spurs on the vertebrae;
- narrowing of the spinal canal (stenosis);
- pregnancy;
- diabetes;
- rheumatoid arthritis;
- compression of the nerve by an oncological neoplasm.
The main symptoms of sciatica are a burning sensation and pain that appears in the lower spine and spreads downward to the leg. Uncomfortable sensations intensify with the slightest movement, disturbing even at night. The patient is limited in movement, and difficulties often arise with the functioning of the hip and knee joints. When diagnosed, abnormal neurological reflexes are observed.
Inflammation of the sciatic nerve most often affects one limb, while the opposite side may become numb, tingling, or have a pins and needles sensation. This is due to a violation of the innervation of muscle tissue. Bilateral inflammation of the sciatic nerve also occurs; the patient experiences severe pain when trying to stand up or make any movement.
The most common cause of inflammation of the sciatic nerve is pinching of the nerve endings due to protrusion of the intervertebral hernia.
The pain syndrome can be of varying degrees of intensity, accompanied by tingling and numbness in the leg, loss of sensitivity of soft tissues.
If timely treatment is not carried out, damage to the sciatic nerve can lead to limited mobility in the knee, feet, disruption of the digestive system, possible urinary and fecal incontinence, often reddened, swollen skin on the lower back or thigh area. The disease must be treated by a neurologist or neurologist.
Therapy for occipital neuralgia
Treatment of facial neuritis with leeches is gaining increasing popularity. The healing effect is observed due to the properties of leech saliva: it restores the necessary nutrition of tissues, dilates blood vessels, and relieves pain. Thus, the use of hirudotherapy for neuritis gives:
- relieving inflammation;
- pain reduction;
- improvement of vascular function;
- strengthening the immune system;
- removal of edema.
Neuralgia of the occipital region causes the greatest discomfort. Severe shooting pains appear in the head. This occurs when surrounding tissue pinches a nerve. Attacks may be accompanied by fainting, vomiting and nausea. Often the pain can be felt in the temples, eyes and forehead
It is important to know the causes of this disease in order to consult a doctor in time
- Occipital neuralgia is accompanied by headache. Symptoms, the treatment of which is aimed at eliminating the causes of the disease, are characterized by acute, lumbago-like pain that begins and ends unexpectedly.
- When you turn your neck or touch the back of your head, pain occurs.
- The nerve is usually affected on one side of the head. But bilateral inflammation is also possible.
- If you touch the skin on your head, you feel pain and discomfort.
- In bright light, your eyes begin to hurt.
In medical practice, two methods of treating this disease are used: conservative and surgical. Drug treatment includes:
- Rest without any physical activity.
- Massage of the nerve affected by the disease.
- Treatment with anticonvulsants: Gabapentin, Finlepsin, Carbamazepine.
- Using muscle relaxants.
- Blockade of nerves in the occipital region. Steroid drugs are used for this procedure. Inflammation is well relieved with Kenalog, Metipred, Dextamethasone, and Hydrocortisone.
If the disease is not treated, occipital neuralgia enters the chronic stage. Symptoms that will be successfully treated, especially with the use of occipital nerve blockade, can be eliminated at an early stage of the disease. Otherwise, surgery will be required. It is carried out in two ways using high quality medical equipment.
How else is occipital neuralgia treated? Symptoms, the treatment of which is often associated with surgery, can be alleviated with the help of folk remedies.
- To prepare the herbal infusion, oregano, peppermint and thyme are used. It is added to the water when a person takes a bath. Herbs are mixed in equal quantities. Place one tablespoon of the mixture in a glass of boiling water, then infuse the solution and filter. Treatment continues for one month, 10 minutes per procedure.
- Compresses made from pickled cucumbers, potatoes and onions relieve headaches. Vegetables are chopped and poured with wine vinegar. They infuse for two hours. Apply a compress to the forehead and back of the head in the morning and evening.
- Drops of beet juice in the ears can quickly relieve headaches. There is no need to cook it. Instead of drops, you can grate the vegetable, wrap the mass in gauze and put it in your ear.
Drug treatment is carried out:
- Painkillers and anti-inflammatory drugs: Diclofenac, Ketoprofen, Ibuprofen, Ortofen. These drugs relieve inflammation and swelling of tissues. But they have a negative effect on the mucous membrane of the intestines and stomach. They are used only as prescribed by a doctor. Physiotherapeutic procedures are prescribed to eliminate pain, but they do not cure the disease. Sciatic nerve neuralgia is treated with various alcohol tinctures, ointments and decoctions. Symptoms, the treatment of which can be effective if the cause of the disease is eliminated, are characterized by impaired sensory function in the area of innervation of the sciatic nerve. Therefore, the use of these funds will only help get rid of the pain syndrome.
- Steroid drugs: Prednisolone, Diprospan, Dexamethasone. These medications are most often prescribed by injection. You cannot use them on your own, as they have side effects.
Remember, ineffective treatment helps to eliminate symptoms for a while. Very soon the pain will return, become even stronger and begin to spread throughout the body. And only comprehensive treatment helps to successfully cope with the disease.
Neuritis and neuralgia
Neuritis is usually infectious in nature. With this disease, inflammation of the femoral, sciatic, tibial or peroneal nerve is observed. The main causes of pathology include the following conditions:
- hypothermia;
- infectious diseases;
- inflammatory diseases of the genitourinary system;
- vascular disorders;
- intoxication of the body;
- compression of the nerve trunk;
- chemical, alcohol poisoning;
- hypovitaminosis;
- complications of diabetes.
When the femoral nerve becomes inflamed, pain, burning and numbness occurs in the outer thigh. Discomfort increases while walking and when making sudden movements. In addition, it is difficult for the patient to bend his leg at the knee.
Sciatic nerve neuritis is most often caused by spinal injuries, pelvic fractures, or cancerous tumors. The main symptoms are impaired sensitivity of the muscles of the lower leg and foot, the patient cannot stand on his toes and heels, the back surface of the buttocks and thighs goes numb. The pain can occur spontaneously, have a throbbing or aching character.
Neuritis of the tibial nerve is manifested by difficulties in flexing the toes, the skin is hyperemic and hot to the touch. Symptoms of pathology are caused by mechanical injuries, viral and infectious diseases.
Neuralgia of the external femoral nerve is manifested by pain on the outer side of the thigh, the syndrome worsens at night, causes insomnia, walking and physical activity also lead to significant discomfort.
Pinched nerve in the knee joint
A condition that develops against the background of a pinched nerve can cause sharp pain in the leg or knee. The main symptoms of the pathology include the following:
- acute pain in the knee;
- decreased sensitivity, numbness;
- burning sensation, tingling sensation;
- involuntary nervous tic;
- limitation of motor activity in the knee;
- muscle atrophy of varying degrees.
Neuralgia (nerve pain) is not an independent disease; most often it appears when the meniscus is damaged, increased physical activity, joint inflammation, as a result of injuries, fractures. In turn, lack of mobility, a sedentary lifestyle, and obesity can also lead to a pinched nerve in the knee. If oncological tumors appear in the joint area, compression of the nerve roots occurs as the tumor grows. This condition can only be treated surgically.
Sometimes inflammation of the nerve endings in the knee is caused by pinching of the sciatic nerve in the spine or compression by intervertebral hernias. For this reason, treatment must be carried out comprehensively.
What is neuritis?
Neuritis is an inflammatory disease of peripheral nerves, characterized by a decrease or complete loss of sensitivity, as well as motor disorders of the tissue innervated by this nerve.
It should immediately be noted that innervation is the supply of various tissues and organs with nerves, through which the central nervous system (CNS) provides them with sensitivity and motor function.
Neuritis can also cause the development of partial (paresis) or complete paralysis.
Most often, the optic, auditory, facial, trigeminal, radial and sciatic nerves are affected by the disease.
If the inflammatory process develops in one place, the disease is called neuritis, while damage to nerves in several places is called polyneuritis.
The main symptoms of neuritis (manifested at the site of inflammation) are decreased sensitivity, numbness, partial or complete impairment of motor function, and pain.
The main causes of neuritis are infections, trauma, tumors, hypothermia, poisoning, various diseases (osteochondrosis, arthritis, diphtheria and others).
Development of neuritis
Thanks to the nervous system, we can see, hear, smell, move, breathe, etc.
The collection of nerves in the body form the peripheral nervous system.
A nerve is a part of the nervous system, which consists of bundles of nerve fibers covered with a sheath, providing communication between the brain (cerebral, spinal) and other parts of the body, organs, and tissues.
There are also blood vessels inside the nerve.
The largest nerves are called nerve trunks, after which they branch significantly, and at the end points, control of the tissue/organ by the nervous system can be achieved with just one nerve fiber. The structure of the nerve may differ depending on its location.
The mechanism of development of neuritis is quite complex, but is caused mainly by disturbances in the nerves - metabolic and vascular processes, their injury, tumors, and infection.
These factors lead to the destruction of myelin and Schwann cells, which are involved in the transmission of nerve impulses along the fibers. With severe pathology, the axial cylinder is also destroyed. At the same time, the nerve fibers are not able to perform the function of transmitting nerve impulses from the brain to the tissues, which is why the latter are not able to perform their functions.
Neuritis, neuralgia and neuropathy (neuropathy) - difference
This is also an interesting question, since various sources combine these concepts, indicating the sameness of this disease. However, in clinical practice these concepts are separated, since the causes, localization, symptoms and further treatment regimen may differ slightly.
Let's consider the distinctive features of these concepts.
Neuritis is characterized by inflammation of the peripheral nerve itself, in which pronounced changes also occur. The inflammatory process involves the myelin sheath (contains myelin and is located inside the glial sheath of the nerve) and the axial cylinder.
Neuropathy (neuropathy) is a disease of peripheral nerves (most often nerve trunks) of a non-inflammatory nature, in which degenerative and metabolic damage to the nerves occurs. The causes of neuropathy are usually impaired blood supply, injury, and metabolic disorders. Symptoms of neuropathy are decreased sensitivity, decreased reflexes, and decreased strength. Neuropathy in psychiatry is diagnosed in the case of increased excitability of the nervous system with increased fatigue.
Neuralgia is characterized by inflammation of the peripheral nerves, but loss of sensitivity, paresis, paralysis and impaired motor activity in the innervation zone are not observed, nor are there any (or minimal) structural changes in the nerve itself. The main symptom of neuralgia is pain (often severe) at the site of innervation, decreased sensitivity. There may be autonomic disorders.
Neuritis statistics
According to medical statistics, neuritis most often occurs in older people, especially women.
Neuritis - ICD
Neuritis: ICD-10 - M79.2, ICD-9: 729.2; Neuropathy: ICD-10 - G60-G64;
Diagnostic methods
To identify symptoms of inflammation of the sciatic, femoral or tibial nerve, relieve acute pain and carry out treatment, you need to consult a neurologist. The doctor examines and interviews the patient. X-rays of the injured limb are taken in different projections; magnetic resonance imaging may be necessary.
In order to diagnose sciatica and neuralgia, the Lasegue test is performed or the “tension symptom” is checked. The essence of the technique is based on identifying spastic muscle contractions when nerve roots are pinched. When the sciatic, femoral and tibial nerves are stretched when bending a straight leg at the hip joint, the patient feels acute pain in the leg, lower back, and thigh.
Lerrey's symptoms help identify nerve inflammation. The patient is asked to rise from a lying position with straight legs. Severe pain indicates damage to the femoral, sciatic or tibial nerve. Pinched vertebrae are determined by the Bekhterev method. The patient's healthy leg is lifted, but pain appears in the affected limb.
Additionally, the patient may need to consult a rheumatologist, neurosurgeon, vertebrologist, oncologist, traumatologist and vascular surgeon. Specialists will help you correctly diagnose and prescribe treatment.
Treatment of inflammatory diseases
Symptoms of infectious neuritis of the sciatic, tibial, femoral and knee nerves can be relieved by taking antibacterial drugs. Additionally, treatment with non-steroidal, anti-inflammatory, antiviral drugs, muscle relaxants, and vitamin therapy is prescribed.
If the symptoms of neuralgia are caused by dilation of blood vessels, ischemia, thrombophlebitis, treatment with vasodilators is prescribed. In case of injury, the limb is fixed and, if necessary, a plaster or tight bandage is applied. The patient is prescribed bed rest; he needs to sleep on a hard mattress. To relieve pain, swelling of the limb should be treated with ointments and gels containing anesthetics; diuretics are also prescribed.
If the pain is too severe, it must be stopped with novocaine or hormonal blockade.
After acute symptoms are relieved, patients are treated with physiotherapeutic procedures: massage, electrophoresis, exercise therapy, UHF, electromyostimulation, manual therapy. For carpal tunnel syndrome, medications are injected directly into the affected canal.
When medication and physiotherapeutic procedures do not help relieve pain, the patient’s condition worsens, and surgery is performed. In this way, decompression of the pinched femoral or tibial nerve is performed. In case of irreversible processes in the nerve fibers, the neurosurgeon performs stitching or plastic surgery of tissues. It is necessary to treat surgically a torn meniscus in the knee, displaced fractures, and hernias of the spinal column.
Inflammation of the sciatic, femoral, tibial and peroneal nerves in young people responds well to therapy, treatment has a positive prognosis. In elderly patients suffering from diabetes, the disease is progressive, and paralysis of muscle tissue and deformation of the joints of the foot may develop.
Pain is the main signal that an unnatural, inflammatory process is occurring in the body, affecting one or another organ or system.
So, inflammation of the nerve endings can cause a lot of pain and neurological problems - numbness and flaccid paralysis, loss of performance, and so on.
Inflammation of nerve endings is an inflammatory process that occurs in the body and affects nerve fibers, endings, and as a result, the development of neuritis occurs.
Doctors distinguish two types of neuritis - primary, which in turn is divided into colds, tunnel or ischemic, and secondary, developing against the background of other neurological pathologies, or as a consequence of their development.
Where do the roots of the problem come from?
Inflammation of the nerve ending can be caused by various reasons:
- external factors - pinching, injury, poisoning;
- internal factors - these reasons include diabetes and pregnancy, excess weight and rheumatism, disruption of the endocrine system, infection and heredity.
But the main root causes that can provoke inflammation of the nerve roots are:
- hypothermia and infections that develop with colds;
- injuries and malfunction of the circulatory system;
- lack of vitamins in the patient’s body, especially B vitamins, as well as poisoning with alcohol , toxins or other harmful substances and heavy metals;
- problems with the functioning of the endocrine glands - this is diabetes mellitus or goiter.
Causes of acoustic neuritis
Infectious diseases
- Influenza is a respiratory disease caused by the influenza virus. After penetration into the mucous membrane of the respiratory tract, the pathogen spreads through the bloodstream throughout the body, affecting various organs, including the auditory nerve.
- Acute respiratory infections caused by adenovirus, parainfluenza virus, respiratory syncytial virus, etc. These infections are known as the common cold. They are rarely complicated by acoustic neuritis; more often this occurs in young children or weakened elderly people.
- Meningitis is a serious disease in which inflammation of the meninges develops. It can be caused by bacteria and viruses and can spread to the auditory nerve, which passes through the cranial cavity.
- Mumps, or mumps, is a viral infection that affects the parotid salivary glands.
- Rubella is a viral infection. Once in the blood, the virus has a strong toxic effect on the nervous system.
Toxic neuritis of the auditory nerve
- Medicines. Antibiotics (neomycin, kanamycin, monomycin, streptomycin), drugs for the treatment of malignant tumors (cisplatin), quinine, acetylsalicylic acid (aspirin) and its derivatives have the most pronounced toxic effect on the auditory nerve. Ototoxicity (toxicity to the auditory nerve) is most severe in children.
- Harmful substances in production: salts of lead, mercury and other heavy metals, phosphorus, arsenic, petroleum products, gasoline. Substances that, with prolonged exposure to the body, lead to hearing loss and inflammatory processes in the auditory nerve, are found in almost every industrial enterprise.
- Alcohol and nicotine are also toxic to the auditory nerve, especially when abused.
Head injury
- circulatory disorders;
- swelling, which varies depending on the severity of the injury;
- pinpoint microscopic hemorrhages from capillaries or more massive ones from cerebral arteries.
infection
Occupational hazards
- Constant exposure to high noise conditions: work in workshops where presses and other equipment that produce loud noise are installed. Typically, neuritis of the auditory nerve, and then hearing loss in these cases, develop gradually over time, with constant regular exposure to noise.
- Acoustic trauma is the acute impact of loud noise on the ear. This is a short, loud sound that causes a strong increase in pressure in the ear and injury. A shot, whistle, etc. can act as a traumatic agent.
- Effect of vibration on the body. Acoustic neuritis and hearing loss are manifestations of vibration disease. Its other symptoms: increased fatigue, headaches and dizziness, poor circulation in the hands and feet (pallor, coldness, pain, tingling and other unpleasant sensations).
Age-related changes in the body
- Arterial hypertension, hypertension. Poor circulation in all organs and systems is a typical complication of high blood pressure. When the auditory nerve stops receiving enough blood, inflammation develops.
- Poor circulation in the arteries of the brain. Most often it is caused by atherosclerosis and thrombosis of cerebral vessels as a result of their age-related changes.
- Age-related changes in the hearing aid - most often occur at the age of 60 - 70 years and are a natural phenomenon of the aging of the body.
- Consequences of a stroke.
Share the article on social media. networks:
Symptoms depending on location
The symptoms of inflammation depend on which nerve or its ending is affected. However, doctors identify common symptoms that are generally characteristic of inflammation of the nerve ending:
- attacks of neuropathic pain , which intensify during physical exertion, during hypothermia, or after a long stay in an uncomfortable position;
- loss of sensitivity and numbness , a feeling of tingling and crawling “goosebumps” throughout the body;
- inability to fully move the limbs , muscles weaken, may gradually atrophy and decrease in size;
- there is a malfunction in the functioning of the vascular system, internal glands of organs and systems , as a result of which the patient sweats excessively, cyanosis and swelling appear on the skin.
Narrower symptoms of inflammation of the nerve ending will depend on the type of neuritis and its location:
- Inflammation in the forearm - ulnar, radial or median nerve - manifests itself in the form of a disruption in the mobility of the limb, when the patient is unable to bend or moves the arm with difficulty, or moves the fingers poorly. At the same time, pain and a feeling of numbness or tingling develop along the affected nerve itself, at the site of inflammation.
- Inflammation of the endings of the femoral nerve - in this case, there is a violation in the ability to flex the limbs in the hip and knee joints, the sensitivity of the dermis decreases, especially in the lower part of the leg and foot, the muscles become flabby and weaken, decreasing in size.
- Inflammation of the endings of the peroneal nerve leads to the fact that a person is simply unable to fully rest on his heels, the gait changes, lameness and shuffling of the foot develop.
- Damage to the endings of the facial nerve - in this case, the affected half of the face will become more relaxed, asymmetry develops, the eyes may not close, the patient is unable to control facial expressions, and the lips move worse.
Diseases arising from inflammation of the nerves
Due to the fact that the inflammatory process is the infringement of the nerve ending, this can lead to the development of many neurological diseases. In particular, with inflammation of the nerve endings of one location or another, the patient may develop the following symptoms:
- Inflammation of the optic nerve roots and, as a result, the appearance of fog before the eyes, problems with visual acuity, pain when moving the eyeball.
- An inflammatory process affecting the hearing aid - in this case, the patient hears poorly and is bothered by tinnitus. If the inflammatory process spreads to the nerve surrounding the brain and the vestibular apparatus, the patient may experience fainting and dizziness, nausea and vomiting, and sensorineural hearing loss may develop.
- Inflammation of the nerve ending can also lead to damage to the facial nerve and, as a result, the lower lip will be displaced downward, the palpebral fissure will widen, and the patient will lose the ability to control facial wrinkles.
- Inflammation of the end of the radial nerve leads to the patient developing drop hand syndrome - the inability to straighten the forearm, wrist, and loss of sensitivity on the back of the hand.
- Inflammation of the nerve endings affecting the endings of the fibular nerve leads to the development of the syndrome of hanging lower limbs - the patient loses the ability to fully move and stand on his heels. His gait changes and muscle atrophy occurs at the site of the inflammatory process and pinching of the nerve ending.
- The inflammatory process and damage to the end of the brachial nerve leads to attacks of pain in the joint, inability to fully move the arm, muscle weakness is diagnosed, and sensitivity of the dermis at the site of inflammation.
- Solaritis - we are talking about inflammation of the end of the solar plexus nerve, acute pain is felt in the chest.
As you can see, inflammation of the nervous system can be localized anywhere - it can be the eyes and shoulders, arms and legs, the solar plexus area, the face and the hearing aid.
Most often, inflammation and, accordingly, infringement of the end of the nerve process affects the facial, optic and tibial nerves - the nervous system permeates the entire body of the patient, which determines that the location of the neuritis can be anywhere.
Types of neuritis
The classification of neuritis is as follows:
Type:
- Mononeuritis - the development of the inflammatory process occurs in one nerve;
- Polyneuritis - the development of inflammation occurs simultaneously in several nerves.
Read also Ichthyosis. Causes, symptoms, types and treatment of ichthyosis
With the flow:
- Spicy;
- Subacute;
- Chronic.
By localization
Optic neuritis – an inflammatory process develops in the optic nerve; divided into:
- Orbital (retrobulbar) neuritis - inflammation develops in the optic nerve located outside the eyeball - from the exit from the sclera to the chiasm.
- Axial retrobulbar neuritis - inflammation develops in the maculopapillary bundle of the optic nerve, which is often accompanied by optic nerve atrophy and vision loss.
- Interstitial retrobulbar neuritis - inflammation develops from the optic nerve sheath to the nerve trunk, deep down.
- Peripheral retrobulbar neuritis - inflammation begins with the optic nerve sheaths, then spreads along the septa to its tissue; proceeds to the interstitial type, with the formation of exudative effusion, accumulating in the subdural and subarachnoid space;
- Transversal neuritis - the inflammatory process spreads to the entire optic nerve, initially developing in the axial fascicle or in the periphery, and then affects other tissues;
- False optic neuritis is an anomaly in the development of the optic nerve, the clinical picture resembles an inflammatory process, while there is no atrophy of the optic nerve or visual dysfunction.
Axial neuritis - inflammation develops in the axial cylinders of the nerve fiber (axon).
Interstitial neuritis - inflammation develops in the connective tissue of the nerve, most often caused by autoimmune processes.
Parenchymal neuritis - inflammation initially develops in nerve fibers (axons and myelin sheath), after which it spreads to the connective tissue parts of the nerve.
Autonomic neuritis - inflammation develops in the peripheral fibers of the autonomic nervous system, accompanied by trophic disorders.
Ascending neuritis - develops mainly when the peripheral part of the arms and legs is injured, after which the pathological process from the periphery moves to the center of the nervous system.
Cochlear neuritis - inflammation develops in the cochlear part of the auditory nerve, the symptoms of which are tinnitus and decreased sound perception.
According to clinical manifestations:
Gombeau's neuritis is characterized by the disintegration of the myelin sheath of nerve fibers, while the axial cylinder remains intact.
Hypertrophic Dejerine-Sotta neuritis is characterized by hypertrophy of the sheath of nerve fibers, which initially leads to compression of the conductive part of the nerve, after which the nerve begins to gradually degenerate and lose its functionality.
Rossolimo neuritis is one of the forms of hypertrophic Dejerine-Sotta neuritis, characterized by a recurrent course and occurring mainly in childhood.
By etiology (cause of occurrence):
Traumatic neuritis - the development of the disease is caused by nerve injury.
Occupational neuritis - the development of the disease is caused by a person’s professional activity - poisoning (chemical fumes, heavy metals and other substances), exposure to vibration on the body.
Infectious neuritis - the development of the disease is caused by infection of the body, infectious diseases.
Alcoholic neuritis - the development of the disease is caused by alcohol consumption, the effect on the body of which is the removal from the body of B vitamins, which are responsible for the functioning of the nervous system, as well as dead brain cells (the process of cell death occurs during alcohol intoxication).