Description of other types of diseases starting with the letter “T”: Toxic encephalopathy; Torsion dystonia; Traumatic encephalopathy; Peripheral nerve injuries; Transient global amnesia; Transient ischemic attack; Cavernous sinus thrombosis; Tuberculous meningitis; Brain tuberculoma; Tuberous sclerosis.
Torsion dystonia is a progressive disease of the central nervous system, which is quite rare in medical practice. The main symptom of the pathology is uncontrolled contraction of various muscle groups, leading to the development of pathological postures. As the pathological condition progresses, the patient experiences various forms of hyperkinesis (sudden involuntary movements).
Complications include joint contracture and spinal curvature. The diagnosis of torsion dystonia is made based on the exclusion of other pathologies of the central nervous system and secondary torsion dystonia. Therapy is carried out with B vitamins, antiparkinsonian drugs, antispasmodics and anticonvulsants. In case of stereotactic destruction of subcortical structures of the brain, surgical treatment is resorted to.
General information about pathology
Torsion dystonia (from the Latin “torsio” - twisting) is a chronic disease of the central nervous system, entailing tonic muscle disorders with the subsequent appearance of hyperkinesis and the formation of aphysiological postures in the patient. A pathology of this nature was first described in 1907, but given the symptoms it was classified as hysterical neurosis.
Later, in 2011, G. Oppenheim proved the organic nature of torsion dystonia, but for a long time there were numerous discussions on the nosological affiliation of the disease. The pathogenesis of torsion dystonia still remains unexplored.
The diagnosis of torsion dystonia is made to patients of any age. However, the vast majority of patients are young people under twenty years of age. 65% of the disease is diagnosed in children and adolescents under 15 years of age. Depending on the place of residence, the incidence of the pathology is 1 case per 160 thousand people or 1 per 15,000. On average, 40 cases per 100,000 population occur.
Torsion dystonia is considered a fairly pressing problem in modern medicine. This is due to the fact that the disease is becoming more common and leads to disability in young people. Moreover, today there is no truly effective pathogenetic therapy to minimize the complications of the disease.
Definition of pathology
Torsion dystonia is a neurological disease characterized by chaotic muscle contractions. Because of them, the patient takes various pathological positions, which is the main sign of a disease of the musculoskeletal system. They first learned about the disease at the beginning of the 19th century, but doctors attributed it to manifestations of neurosis. A description of this form of dystonia was obtained only a few years later by the scientist G. Oppenheim. He revealed the organic nature of the pathology, but the pathogenesis was never clearly defined.
The code for dystonia according to the ICD (International Classification of Diseases) 10th revision is assigned to G24. It describes in detail all forms of the disease. This disease should not be confused with VSD (vegetative-vascular dystonia), since they differ in both clinical picture and causative factors. Mostly young people suffer from such disorders. According to statistics, 70% of cases occur in children. In adulthood, it actually occurs 2-3 times less often.
Reasons for the development of torsion dystonia
The causes and mechanism of development of torsion dystonia still remain in question. In medical practice, symptomatic and idiopathic cases of pathology are known. The only thing that can be said with certainty is the hereditary nature of torsion dystonia. There is also evidence that there are several ways of inheriting the disease: autosomal dominant and autosomal recessive. In the case of autosomal dominant inheritance of the pathology, it manifests itself at a later age and is characterized by a relatively mild course.
Symptomatic torsion dystonia is diagnosed when:
- Wilson's disease;
- cerebral palsy;
- epidemic encephalitis;
- Huntington's chorea;
- brain tumors;
- traumatic brain injuries.
There is a widespread belief among doctors that the pathology in question is a consequence of a disorder in the metabolism of dopamine in the body. This assertion is not groundless. Thus, in most cases of a confirmed diagnosis of torsion dystonia, an increased level of dopamine hydroxylase is found in the blood of patients.
Regarding the pathogenetic theory of the disease, the most common one is the one that says that the disease develops as a result of a disorder of subcortical regulation. This theory is confirmed by pronounced morphological degenerative changes in the subcortical nuclei (substantia nigra, basal ganglia, red, subthalamic).
Causes
The disease has two forms of occurrence: hereditary and symptomatic. Symptomatic cases are characterized by the following provoking factors: oncology, tick bites and the development of encephalitis, cerebral palsy, post-traumatic complications.
This disease has not been studied in more detail. Medicine does not consider more obvious reasons for the occurrence of such disorders. Scientists accurately identify several forms of this disease, the appearance of which is determined by several factors .
The autosomal dominant type of the disease appears in adulthood, the symptoms are not too difficult to tolerate. Torsion dystonia appears due to diabetes mellitus, difficult childbirth, poor heredity, central nervous system pathologies, vascular problems, intoxication, toxoplasmosis, cerebral palsy, etc. The hereditary variety of the disease is diagnosed less frequently; manifestations in such a situation occur in 2-3 generations in the same family or in a situation where the parents of the children are too closely related.
Classification of torsion dystonia
The focal form of torsion dystonia is accompanied by tonic spasms of individual muscles. This group includes:
- Writer's cramp. In this case, the hand muscles contract involuntarily, which is why the patient has problems with writing. This also includes spasms of the foot and neck muscles.
- Oromandibular dystonia – there is an involuntary contraction of the masticatory muscles (mouth, cheeks, tongue).
- Idiopathic blepharospasm - due to the fact that a tonic spasm of the orbicularis oculi muscle occurs, the patient experiences involuntary closure of the eyelids.
- Spasmodic dysphagia - the patient complains of difficulty swallowing function or its complete absence.
- Spasmodic dysphonia - there is a tonic contraction of the vocal muscles, which is accompanied by loss of voice production function.
Other forms of torsion dystonia are:
- Hemidystonia – the muscles of half the body are affected and impaired.
- Generalized form - almost all muscle groups are subject to uncontrolled contraction.
- Segmental form of dystonia - tonic contraction is observed in several muscle groups, which are mainly located nearby.
- Multifocal – a combination of several focal forms of torsion dystonia.
Classification
Torsion dystonia is a common disease, reflected in the World Classification of Diseases, according to ICD-10 it has the code G20-G26.
In modern medicine, it is customary to distinguish the gradation of the disease according to various principles.
By age characteristics:
- infant group - up to 2 years;
- children's group - 3–12 years old;
- teenage – 13–20 years;
- dystonia of early age - 21–40 years;
- dystonia of older age - after 40 years.
According to the anatomical distribution, the following types of dystonia are distinguished:
- focal - a specific area of the body is captured (head, neck, facial muscles, torso, upper and lower limbs, vocal cords);
- segmental form - characterized by the involvement of two or more adjacent parts of the body (head and neck, neck and arm);
- multifocal - involves more than two non-adjacent parts of the body (face and leg, arm and leg);
- generalized - manifested by the involvement of both legs or torso, one lower limb and torso;
- hemidystonia - the process involves the muscles of half the torso, face and neck, which often indicates a secondary condition.
According to the pathoanatomical principle:
- with degeneration, when there is a disappearance of certain functional features of the muscular system and muscle group;
- without degeneration - the damage is static.
According to etiological criteria:
- Primary. Diagnosed when muscle twisting is the only symptom. They occur for a genetic reason. There are two forms: local and generalized (uncontrolled tonic contractions of the muscles of the whole body).
- Dystonia-plus. This group includes cases with severe dystonic syndrome, which is supplemented by concomitant symptoms (paroxysm or myoclonus), but without degeneration.
- Neurodegenerative. Hereditary diseases (Wilson's disease and others) with a progressive process of degeneration.
- Secondary. They are characterized by a sudden condition with an established cause; there is no degeneration of functions.
The genetic classification includes a large number of gene mutations and is hereditary in nature, transmitted in an autosomal recessive or autosomal dominant manner. This form has a second name - idiopathic torsion dystonia, and is characterized by slow progression.
At the diagnostic stage, the doctor differentiates the disease, determines its type and severity.
Clinical picture
The first symptoms of torsion dystonia are focal spasms. They appear periodically and mainly when there is a load on the muscle group that is susceptible to the disease. For example, at an early stage of development, the writing form of pathology appears only during writing. Involuntary contractions correspond to hyperkinesis (motor acts that the patient cannot control). Such movements may have the following character:
- tonic;
- myoclonic;
- tick-shaped;
- hemiballic;
- tremor-like;
- choreatic;
- athetoid;
- myoclonic.
At the same time, hyperkinesis is less pronounced in the distal parts of the limbs than in the proximal ones. Rotational movements of the torso or limbs along the longitudinal axis are typical for pathology.
A characteristic symptom is a change in the number of involuntary acts or spastic postures. They correspond to the functional activity and body position of the patient, as well as his emotional state. Thus, while walking, the patient experiences corkscrew-like movements of the body, and when trying to perform a certain action, involuntary contraction of the muscles of the limbs.
All manifestations of torsion dystonia disappear during a period of calm, namely during sleep. Moreover, patients can adapt to their movement disorders and temporarily reduce the severity of involuntary movements. At this time, they can perform complex motor movements and fully maintain self-care.
Frequent and involuntary muscle contractions often lead to hypertrophy or prolonged spasm. In the latter case, connective tissue replacement of muscle tissue occurs, as a result of which shortening of the muscle is formed and its ability to stretch is lost. Constant and prolonged muscle spasms lead to degenerative processes that develop in the joints. Next, joint contracture is formed.
Tonic spasms of the back muscles provoke the development of the following diseases:
- scoliosis;
- rachiocampsis;
- lumbar lordosis;
- kyphoscoliosis.
At later stages of the disease, the patient's respiratory function may be impaired.
In some cases, at an early stage of development of the pathology, its local forms are noted, which over time and without proper treatment develop into a generalized form. The generalized form is accompanied by an “unusual” gait with a wide gait. Periodically, the patient's posture becomes abnormal and the person freezes in it. In some patients, isolated local manifestations persist during the disease, and the dystonic process passes without generalization. As a rule, this clinical picture is observed in patients aged 20-40 years.
Conservative treatment
While it is impossible to cure torsion dystonia, it is possible to slow down the progression process. The main drugs for treatment are Nakom, Sinemet, Madopar. In clinical practice, these drugs have proven to be among the most effective. Over a short period of time, they help relieve a person from pathological postures and from frequent attacks of hyperkinesis. The effectiveness of treatment is much higher than when treating parkinsonism with the same drugs.
In some patients, it is worth combining levodopa, Yumex and bromocriptine. Taking these three medications will help avoid numerous complications. In addition, such a treatment regimen will be effective throughout the entire period of the disease and does not depend on its stage or duration.
Diagnostic measures for torsion dystonia
In the neurological status, the following symptoms allow one to suspect the development of torsion dystonia:
- rigidity of certain muscle groups;
- preservation of tendon reflexes;
- no reduction in muscle strength;
- absence of sensory disorders.
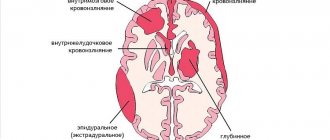
The neurologist, first of all, must differentiate idiopathic torsion dystonia from secondary torsion-dystonic syndromes. Secondary syndromes, in most cases, are characterized by symptoms of damage to the nervous system, sleep disturbances, and autonomic disorders. As part of differential diagnosis, patients are referred to:
- EEG;
- Echo-EG;
- Doppler ultrasound of head vessels or REG;
- MRI or CT scan of the brain.
Torsion dystonia can be distinguished from hepatocerebral dystrophy by the fact that the patient does not have pigment deposits in the cornea. There is also no liver damage and a decrease in blood ceruloplasmin is observed. The difference with epidemic encephalitis is the absence of an acute period. A patient with torsion dystonia does not have sleep disorder, diplopia, convergence disorder, or autonomic dysfunction.
Diagnostics
If symptoms characteristic of torsion dystonia are detected, the patient should consult a neurologist. The specialist will interview the patient and conduct an examination. Particular attention will be paid to increased muscle tone while maintaining muscle strength and the absence of disorders associated with sensitivity.
The purpose of diagnosis is to differentiate torsion dystonia from other neurological diseases. The following examination methods will help with this:
- Electroneuromyography allows you to see changes in the activity of muscle tissue and nerve pathways.
- Magnetic resonance imaging is prescribed to identify damaged areas of the brain.
- Radiography makes it possible to see the condition of the skull bones and indirectly confirm the presence of certain pathological processes.
- An electroencephalogram determines the degree of brain activity.
Based on the results obtained, the doctor will be able to accurately make a diagnosis. The treatment regimen is drawn up depending on the severity of the disease and its causative factor.
Therapy methods
When treating torsion dystonia, the same drugs are used as in the treatment of parkinsonism. We are talking about the following medications:
- combination decarboxylase inhibitor levodopa and carbidopa;
- dietazine;
- anticholinergics trihexyphenylide;
- selegiline;
- triperiden;
- centrally acting antispasmodics (diphenyltropin);
- vitamins B1 and B6;
- a-DOPA (in small quantities);
- carbamazepine, baclofen, tiapride (if hyperkinesis is pronounced).
In addition to drug treatment, patients are prescribed hydrotherapy and exercise therapy. In the secondary form of dystonia, treatment depends on the underlying cause of the disease.
In case of disability or rapid progression of the pathology, surgery is indicated, which is performed by a neurosurgeon. In this case, stereotactic combined destruction of the basal subcortical structures, namely the ventrolateral thalamic nucleus and the subthalamic zone of the brain, is indicated. If dystonia is local in nature, then it is performed contralateral to muscle disorders.
The operation for the generalized form, in most cases, is carried out in several stages. Surgery is performed first on the opposite side from where the symptoms are most severe. After 6-8 months, the operation is performed on the second side. If the severity of rigidity is symmetrical, the first stage of the operation is performed on the dominant hemisphere. In the majority of cases (80%) after surgery, there is a period of improvement in the patients' condition, which persists for a long time in 66% of cases.
Course of therapy
The essence of therapy for torsion dystonia is to eliminate the causative factor and relieve symptoms. It includes physiotherapeutic procedures, lifestyle modifications and medications. In severe cases or when other treatment methods are ineffective, surgery is used.
The course of drug therapy usually includes the following medications:
- Muscle relaxants (Tizanidine, Mellictin) are used to reduce the tone of muscle tissue and relieve convulsive attacks.
- Anticholinergic drugs (Scopolamine, Metamizil) block M-cholinoreactive systems and relieve spasms.
- Sedatives (Relanium, Phenazepam) reduce nervous excitability, improve sleep and restore the usual psycho-emotional background.
- Beta-blockers (Ormidol, Aldometa) are prescribed as an addition to the therapy regimen. They reduce the effects of adrenaline, which normalizes the heart rhythm and stops tremor (shaking).
The desired effect from taking medications is not always achieved. To improve the patient's condition, surgery may be prescribed. It comes in 2 types:
- Neurostimulation represents a group of minimally invasive operations. With its help, the surgeon acts only on certain areas of the brain.
- Radiotomy and stereotactic techniques are considered full-fledged surgical interventions. Their essence lies in the destruction of damaged areas of the cerebral cortex.
Minimally invasive surgeries are easier to tolerate and have fewer side effects and a shorter recovery period. Full surgical intervention is required for extensive brain damage. Such radical treatment methods have their own indications:
- low effectiveness of drug therapy;
- rapid progression of the disease;
- rapid development of a generalized type of pathology.
Forecasts
The outcome of idiopathic torsion dystonia depends on the time of manifestation of the disease. The early onset of pathology entails a severe course. In this case, early generalization and deep disability of the patient develops. When intercurrent infections occur, the patient's death follows.
With timely surgical treatment, the prognosis is more favorable. In most cases, after surgery, rigidity and hyperkinesis disappear in patients. They retain the ability to walk, perform complex movements and care for themselves. In cases with secondary torsion dystonia, a favorable prognosis will be only if timely and effective treatment is possible. In this case, regression of spasms and hyperkinesis is noted.
Consequences
Despite the effectiveness of modern treatment methods, most doctors noted the rapid progression of torsion dystonia. The disease very often behaves aggressively and leads to disability and death. Radical methods of therapy (surgical intervention) do not help in all cases. This is especially true for generalized forms of torsion dystonia. Avoiding the consequences and transferring the pathology into remission is possible only with timely detection and preparation of an effective treatment regimen.
Torsion dystonia is a neurological disease characterized by involuntary contractions and spasms of muscle tissue. The essence of treatment is the use of various drugs to improve the general condition and slow down the progression of the pathology. If there is no effectiveness, surgery is performed.
Types of violation
Torsion dystonia is characterized by uneven muscle tone of parts of the body, and rotational movements often occur.
The disease most often manifests itself in the form of spasms of individual muscle groups - the focal form. With this form, involuntary closure of the eyelids occurs due to tension in the orbicularis oculi muscle. Contraction of the muscles, cheeks, mouth and tongue also occurs, swallowing is difficult, and in some cases with spastic dystonia the patient cannot speak.
https://www.youtube.com/watch?v=WNeGz-fydbE
Torsion dystonia, depending on its manifestations, is divided into 2 types:
- Symptomatic etiology - is a consequence of diseases or damage to the brain (brain tumors, cerebral palsy, encephalitis, traumatic brain injury).
- Hereditary etiology - transmitted hereditarily. Transfer can be carried out in different ways. In some people, the disease is transmitted by a dominant type (the disease is traced in 2-3 generations), in others by a recessive type (the disease is traced in 4-5 generations, and there are cases where the parents were related).
Also, the disease, depending on the degree of damage, is divided into the following types:
- Local. Not all muscle groups are affected, but individual ones (writer's spasm, buccal or facial dystonia, blepharospasm). When the neck muscles are damaged, spastic torticollis occurs.
- Segmental. Spasms of several adjacent muscle groups occur.
- Generalized. With this disorder, the muscles of the pelvis, back, trunk and limbs are affected.
Pathogenesis and clinical manifestations
Direct torsion dystonia develops as a result of a disturbance in the metabolism of the neurotransmitter dopamine in the extrapyramidal system of the brain (subcortical motor center). In this case, two forms arise - dopamine-dependent (rigid) and dopamine-independent (hyperkinetic). This is a very important point, since the treatment will vary for different forms. It is also known that the autosomal dominant variant is milder than the autosomal recessive variant.
An important sign of torsion dystonia is its gradual development. Initially, the patient complains of small rotational spasms in various parts of the body, most often on the extremities (especially the lower ones). This usually occurs on one side of the body. In this case, difficulties with walking very often arise.
Subsequently, such corkscrew-like spasms begin to appear much more often in other parts of the body. This is the so-called local form. It can become generalized, in which large muscle groups are involved. Symptoms intensify if the patient tries to concentrate and make the right movement. During sleep, symptoms of the disease usually disappear.
If the hyperkinetic form is characterized by clonic convulsions (i.e., muscle contraction is followed by its relaxation), then with the rigid form spastic ones develop (convulsions in which the muscles are tense for a long time). In this case, fixed pathological postures arise, both in local areas and in the entire body.
With the further development of torsion dystonia, complications such as writer's cramp, contractures, joint deformation, curvature of the spine and torticollis appear. The gait changes, and disturbances in speech, chewing, swallowing, and breathing may occur. Due to the constant load on the muscles, their hypertrophy occurs.
Pathogenesis
The above etiofactors cause dysfunction of the multi-level system for regulating muscle tension. The result is spontaneous impulses that over-activate certain muscles. The activated muscle group enters a state of tonic contraction, which leads to violent movement followed by freezing.
Depending on the location of the muscle group subject to pathological impulses, involuntary turning of the head, twisting of the body, squinting of the eye, dystonic trismus, etc. are possible. The alternation of excessive tension of antagonist muscles underlies hyperkinesis - involuntary motor acts of varying amplitude and speed. The pathogenetic mechanism of development of many MD continues to be studied.