The most common traumatic brain injury is a concussion. The brain itself does not receive any anatomical damage due to such exposure. Neurological symptoms that occur after a concussion most often resolve on their own. To diagnose the consequences of such an injury, MRI is used. The diagnostic process includes interviewing the patient, visual examination and the use of instrumental techniques. In the acute phase of a concussion, MRI is not used, since no structural changes in the organ occur in this case. Using MRI of the brain, you can determine the condition of the nervous tissue and promptly detect whether the patient has serious problems. This procedure is performed some time after the injury. It makes no sense to do it in the acute period.
Experts classify a concussion as a minor injury, accompanied by minor dysfunction of the organ. A person who has been injured usually has the following symptoms:
- short-term loss of consciousness;
- headache;
- sleep disturbance;
- short-term memory loss;
- nausea, vomiting.
The victim may lose consciousness after receiving such an injury for a period of several seconds to five minutes. After a person regains consciousness, he may not remember the events that preceded the trauma or occurred immediately after it (retrograde or anterograde amnesia). Within a week, all symptoms usually disappear. However, in some cases they may remain, indicating more severe damage. In such situations, the main task facing doctors is their timely identification.
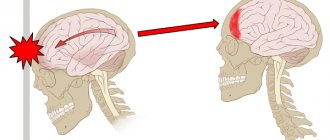
These include, for example, a brain contusion. This injury is more serious. It is accompanied by morphological changes in the organ. Cell damage occurs and connections between axons and their processes are disrupted. Intracranial blood vessels may also be damaged, hematomas and hemorrhages may form. After a strong blow to the head, the nervous tissue receives two blows at once. One of them falls on the site of physical impact, and the other on the opposite area. This occurs as a result of brain injury from the inside of the skull. Such injuries are characterized by a long recovery period, which can last several months. With the help of computed tomography, the doctor is able to promptly find out about the presence of injuries in the patient and prescribe the necessary treatment in a timely manner. The MRI procedure allows you to identify the consequences of an injury after a certain time and, based on the information received, select the optimal method of rehabilitation.
What can an MRI show?
- injuries of varying degrees of severity to soft tissue areas;
- neoplasms of benign and malignant nature;
- disorders of the brain structure;
- inflammation;
- traumatic brain injury (fracture of the skull bones);
- change in the shape or volume of an organ;
- cerebral vascular atrophy;
- pathological disorders in the vascular system (thrombosis, aneurysms, strokes).
In order to identify any serious pathology associated with vascular disorders of the brain or injuries sustained during a concussion, doctors prescribe a tomography using a contrast agent, which is injected into the patient’s vein. This procedure improves the signal visualization that comes from the bloodstream. In this way, the doctor can see a complete picture of the cerebral vascular system. However, in most cases, the study of blood vessels is carried out in a standard way without the use of contrast.
Treatment of concussion
Once a concussion is diagnosed, no special treatment is usually required. However, you cannot immediately go to work, training, or anywhere else except bed. Firstly, it has been established that if bed rest is not observed, the risk of re-injury or complications increases. In other words, you need to rest in order to recover faster. In the future, you need to gradually enter the usual mode of operation. Secondly, in the first day or two, signs of serious complications of the injury (intracranial hemorrhage) may appear, so at first someone should be with the patient to call for help.
Basic rules of behavior after a concussion until symptoms disappear:
- rest;
- sleep more;
- limit physical activity;
- do less activities that require concentration (do not work on the computer, do not play video games, etc.);
- do not drink alcohol or soft drugs;
- avoid stressful situations;
- do not take sleeping pills, sedatives or tranquilizers (unless prescribed by a doctor);
- don't drive.
You should contact your doctor again if:
- you vomited more than three times;
- a severe headache occurred or it began to gradually intensify;
- there were problems with speech and speech understanding;
- gait has changed;
- vision has deteriorated;
- there were convulsions;
- some part of the body has become weak or numb;
- urinary or fecal incontinence has occurred;
- symptoms do not go away within two weeks.
The person who will monitor the patient for the first time should call an ambulance or take the loved one to the hospital if, in addition to the above signs, he notices drowsiness, persistent confusion, anxiety, if he cannot wake up the person (you need to periodically wake up the patient, to check whether he is regaining consciousness), if there is a fever, and also if, due to excessive tension in the neck muscles, it is difficult for a person to move his head. All this may indicate intracranial bleeding, swelling of the brain, inflammation of its membranes.
Consequences of a concussion
After a concussion, a person may experience headaches with symptoms similar to tension-type headaches (TTH) or migraines. With tension-type headache, the pain is not very severe, felt on both sides, and intensifies in the evening. With a migraine, the pain is quite severe, on the one hand, throbbing, and may be accompanied by nausea, intolerance to light and sound. If attacks occur infrequently, then painkillers such as ibuprofen, paracetamol, etc. are quite suitable. If the pain is chronic, the doctor will prescribe medications to prevent it (for example, tricyclic antidepressants in small doses).
In some cases, the blow leads not only to a concussion, but also to injury to the vestibular system. This, in turn, provokes post-traumatic dizziness. The doctor will determine the exact cause of this condition and prescribe appropriate treatment: from simple exercises to surgery.
Also, after a mild TBI, the risk of developing epilepsy during the first five years after injury doubles.
In rare cases, a minor traumatic brain injury can cause damage to the cranial nerves. This condition will manifest as decreased or absent sense of smell (hyposmia or anosmia), double vision (diplopia), facial pain, and pain in the back of the head. These injuries may be permanent, temporary (will go away on their own), or require surgery.
If concussions occur over and over again (as often happens in boxing, football and other sports), it can lead to chronic traumatic encephalopathy. In other words, a person’s mental abilities may deteriorate, personality and behavior may change, depression, suicidal tendencies, speech and gait disturbances, and parkinsonism (stiffness of movements, trembling of limbs) may occur. This also increases the risk of developing Alzheimer's disease in the future. This is why it is so important for athletes to take precautions and give themselves rest. Even if there are no symptoms after a head hit, it is highly not recommended to immediately return to the game: this can be done at least the next day.
Symptoms of concussion and skull injuries:
- damage that is visible to the naked eye;
- headache;
- vomiting reflex;
- nausea;
- loss of consciousness;
- nose bleed;
- pale skin;
- temperature increase;
- decreased performance;
- slow reaction;
- poor appetite.
Symptoms
The symptoms of a concussion are pronounced and characteristic. In the first minutes after injury, the following clinical picture develops:
- vomit;
- pronounced increase in breathing;
- disturbances in the rhythm of the pulse (slowing or, on the contrary, increasing);
- partial or complete loss of memories of immediate events preceding the injury.
Most often, the patient’s recovery period is not accompanied by deviations from the norm in body temperature and blood pressure, but the following characteristic symptom complex of the rehabilitation period is observed:
- severe, varied headaches;
- dizziness;
- nausea;
- general weakness;
- inhibition of cognitive processes;
- noise in ears;
- sweating
It should be noted that all of the above symptoms are characteristic exclusively for patients of the young and middle age groups, while newborns and elderly people demonstrate a slightly different clinical picture. The fundamental difference here is the absence of a symptom of loss of consciousness.
After injury, young children exhibit frequent regurgitation, weakness and drowsiness, while older people report impaired coordination of movements and disorders of mental activity, including memory. Due to the uncharacteristic clinical picture and the vulnerability of the body, patients in this age group first of all need tomography for a concussion.
Features of the MRI procedure
- Before the procedure, it is imperative to identify the presence of contraindications, if the patient has them.
- The patient must remove all metal jewelry and then take a stationary position on a special tomography table. His head is fixed.
- The doctor is in another part of the treatment room, separated by a glass partition. A two-way communication system allows the doctor to give commands to the patient and communicate with him.
- The patient must remain absolutely still to avoid inaccurate test results. Unfortunately, sometimes this is not possible if the patient is afraid of confined spaces or is a small child. For such purposes, a special sedative is provided.
- If the patient is a child who is not older than six years old, the doctor administers a mild anesthesia to keep the child calm. For older children, doctors recommend magnetic resonance imaging (MRI) in the morning.
If a patient has suffered a traumatic brain injury or concussion, the pressure inside the skull bones increases for a short time. At this moment, physical and chemical processes occur in the brain fluid, and cell nutrition also deteriorates. In some cases, the interaction of cellular structures with brain regions is completely lost.
A timely tomographic diagnosis can not only confirm the absence of any serious changes associated with a concussion or traumatic brain injury, but also make an accurate diagnosis and determine the presence of more dangerous problems in order to subsequently create a plan for effective treatment of a concussion.
Physiological manifestations of concussion
Pathology arises, as mentioned earlier, as a result of trauma, which can be of a different nature and affect any part of the patient’s skull. In this case, a lightning-fast increase in intracranial pressure develops, which is considered a direct etiological factor causing further functional disorders - loss of intercellular connections of brain structures, disruption of cellular nutrition, physicochemical transformations.
After a concussion, MRI is also performed to identify more serious consequences, including rupture of intracranial vessels and irreversible traumatic changes in areas of the brain. It is this type of research that is most informative regarding morphological and structural changes.
What diseases does MRI of the brain show - complete list
Most modern instrumental diagnostic methods do not allow a full assessment of the state of the brain: ultrasound practically does not penetrate the skull bones of an adult, CT, based on the principle of X-ray, provides an extremely insignificant amount of data. Magnetic resonance imaging, due to its ability to detect the slightest vibrations of atoms under the influence of an electromagnetic field, is free from these disadvantages. Here is what an MRI of the brain shows from various diseases:
- neoplasms. MRI scans detect tumors of both the brain itself or its membranes, and the pituitary gland. This study is not able to reliably establish the benign or malignant type of tumor, however, it allows us to determine many other parameters. The growth rate, size, and localization of neoplasia relative to vital nerve centers largely determine the need for surgical intervention, its volume, and make it possible to predict the course of the disease;
- vascular aneurysms. An aneurysm is a local thinning and expansion of the vascular wall, which can rupture at any time, causing intracranial hemorrhage. The main danger of this disease is that it is almost always asymptomatic and can instantly kill a person at any time;
Vascular aneurysm on MRI
- ischemic strokes (cerebral infarction). Blockage of the artery lumen by a blood clot or atherosclerotic plaque inevitably leads to the death of some tissue. An MRI will help determine the location of the blood clot and the extent of brain damage. The most important thing is that MRI of the brain allows one to distinguish ischemic stroke from hemorrhagic one, which significantly influences treatment tactics and can save the patient from severe consequences and death;
- encephalitis, meningitis. Inflammation of the brain itself or its membranes is one of the most severe types of infectious diseases. These processes never pass without a trace, and their untimely detection only worsens the prognosis, increasing the patient’s chances of receiving a disability group;
- multiple sclerosis. This pathology slowly, over decades, transforms a person from a healthy person into a deeply disabled person, incapable of even self-care. MRI of the brain today is the only publicly available way to determine the foci of multiple sclerosis and the rate of its progression. Only on the basis of these data can a comprehensive treatment be selected that can slow down or even stop the pathological process.
What does a brain MRI show?
Classification of types of concussions according to ICD 10
Before describing the coding features according to the International Classification of Diseases, Tenth Revision, it is necessary to determine the nature of the changes:
- Open wound;
- No external defects.
The nosology code called “concussion” is “S06”. Name in Latin “commotio cerebri”. When describing the diagnosis, it is necessary to identify:
- Traumatic cerebral edema – “S06.1”;
- Diffuse brain injury – “S06.2”;
- Focal traumatic injury – “S06.3”;
- Epidural hemorrhage – “S06.4”.
When determining the extent of damage, contusions and ruptures should be verified. Traumatic injury is accompanied by a number of changes - cerebral rupture, contusion, intracerebral hemorrhage.
Treatment
For severe TBIs, surgery is usually performed. The procedure may consist of primary surgical treatment. But sometimes, you have to do craniotomy, pump out fluid, remove hematomas, restore (assemble) the skull. After surgery, it is treated with medications.
If the victim is vomiting, it is stopped with an injection of Metoclopramide or Etamzilate. Pain is relieved with analgin. If there is no vomiting, they give a tablet (no more than 2 per dose), otherwise it is administered by injection.
In order to normalize blood circulation and metabolic processes in the brain, Etamzilat and Piracetam are prescribed. The standard dose is 2 tablets (varies depending on the patient’s age).
In addition, based on the nature of the injury and its clinical manifestations, he may prescribe:
| A drug | Therapeutic effect |
| Eufilin | Neutralizes cerebral edema. Prohibited for people with low blood pressure. |
| Askorutin | Strengthens the vascular system. |
| Cefatoxime, Amoxicillin | Prescribed for rupture of the meninges. The first symptoms are discharge of cerebrospinal fluid from the nose and ears. The drugs prevent complications such as meningitis. |
Even if the patient is at home, it is important to follow the following recommendations:
- avoid sudden movements;
- stay in the shade, do not overheat;
- ensure silence;
- get plenty of rest and sleep.
Are blood vessels visible on brain tomography?
Much of what an MRI of the brain shows depends on the presence or absence of additional contrast. The use of contrast agents is especially important when studying the vascular bed in the central nervous system. The introduction of special drugs that respond to a magnetic field allows you to “illuminate” the vessels and make the entire image brighter and more contrasting. In fact, MRI of the brain with contrast is, along with CT, a method that allows one to sufficiently assess the state of the vascular system inside the skull.
The use of this technique is especially useful in assessing the presence, location and size of aneurysms, thrombosis, and abnormalities in the development of the cerebral vascular bed. MRI with contrast also allows a more accurate assessment of the size and boundaries of tumors, based on the data obtained about the vessels passing through them.
Modern contrast agents are quite safe and rarely cause complications. The risk of developing allergic reactions is significantly reduced by conducting a preliminary sensitivity test to the contrast used.