Trigeminal neuralgia of the face often manifests itself in attacks with severe pain symptoms, as well as other signs. If treatment is not carried out, then the manifestations of the disease will worsen in the future, which can lead to various complications.
Trigeminal neuralgia is also called Trousseau's tic . This nerve element is designed to control the facial and chewing muscles. With neuralgia, symptoms of intense pain usually appear in the places where the nerve branches pass.
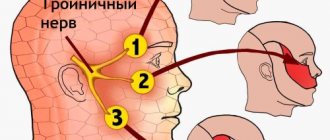
Photo 1. What is the trigeminal nerve responsible for?
The disease is often diagnosed in people of working age; small children can rarely get it. It is worth noting that, compared to other pathologies that may affect the peripheral nervous system, trigeminal neuralgia causes the most unpleasant symptoms. In addition, the complexity of treatment is influenced by the wide variety of causes that can cause pathology and its progression. In addition, difficulties often arise already at the diagnostic stage, since the signs of neuralgia are similar to other disorders of the nervous system.
Causes
The variety of factors that cause trigeminal neuralgia is quite large. They are divided into two groups and belong respectively to exogenous, that is, external, and endogenous, that is, internal. Usually the disease occurs as a result of :
- Serious mechanical trauma to the facial area or skull
- Hypothermia
- Deviations in the blood supply to the areas where the vessels approach the trigeminal nerve. Quite often these are consequences of atherosclerosis, abnormalities in the structure of blood vessels, the presence of an aneurysm, etc.
- Disturbed metabolism
- Stem stroke
- Various chronic diseases
- The appearance of cancerous or benign neoplasms
- Multiple sclerosis
- The existence of cystic phenomena in the area where the nerve endings pass. The cause of such formations is often incorrect or insufficient dental, ophthalmological and other treatment.
Photo 2. Innervation diagram
At the initial stage, it is rare that the action of the pathological process covers the entire area of the trigeminal nerve. However, if neuralgia is not treated, then the likelihood of it spreading to healthy parts is very high. In this situation, it is impossible to avoid the aggravation and expansion of a person’s existing symptoms and manifestations.
Clinic
According to ICD 10, trigeminal neuritis heads the group of diseases of this pair of cranial nerves.
The trigeminal nerve has this name because it consists of three branches and is mixed, that is, it has both motor and sensory fibers. Accordingly, the clinical picture and severity of symptoms of trigeminal neuralgia depend on the affected area.
If the pathological process affects the first branch, then the pain is localized in the skin of the forehead, a small area of the scalp, the upper eyelid, and the back of the nose. Due to disruption of the upper nasal sinus, the patient may complain of impaired sense of smell. On neurological examination, a decrease in the corneal and brow reflexes may be noted.
When the second branch of the trigeminal nerve is damaged, pathological symptoms are observed in the area of the upper lip, lower eyelid, upper cheek and area of the lateral surface of the face. These are pain, numbness, paresthesia and sensory disturbances. The teeth of the upper jaw and maxillary sinus are also affected.
The last branch contains motor and sensory fibers and innervates the rest of the face. Damage to the third branch of the trigeminal nerve is characterized by paralysis of the masticatory muscles and paresis of the facial muscles. In this case, the retraction of the muscles in the area of the temporal fossa and the asymmetry of the masticatory muscles are very clearly visible. The patient may complain not only of pain, but also of changes in the bite. If the lesion is bilateral, then the lower jaw will sag. Such symptoms are associated with damage to motor fibers.
Second
and the third branches are most often affected. But if it is postherpetic neuritis, then the causative agent lies in the Gasserian node and then all parts of the trigeminal nerve are affected.
The pain in this disease is paroxysmal, short-term, and has a sharp, “shooting” character. There can be up to several dozen such cases a day, and their duration ranges from a few seconds to ten minutes. The painful sensations are very vivid and cause severe discomfort. Any touch can cause it. Because of this, patients sharply limit their activity, may refuse to eat, shave, or personal hygiene, and reduce their social life.
A disease such as trigeminal neuritis has symptoms that are not only pain.
Inflammation of the trigeminal nerve is often unilateral, which, when motor fibers are damaged, is noticeable to the naked eye: the corners of the eyelids and mouth are drooping, facial expressions are sluggish or completely absent. Small muscle twitches and tics may appear.
Autonomic symptoms include excessive salivation, lacrimation, hyperhidrosis, and redness of the skin.
Symptoms
In most cases, almost three-quarters, the trigeminal nerve is affected by neuralgia on the right side . Quite rarely, defeat affects both sides at once. The disease develops through periods of exacerbation and remission, when its symptoms either intensify or disappear. The most favorable period for exacerbations is autumn and spring, which is associated with an increase in humidity simultaneously with low temperatures. It must be remembered that if the disease is not treated, then bilateral manifestations cannot be avoided in the future.
Trigeminal neuralgia manifests itself in various symptoms; consider each of their groups in detail.
Painful
Symptoms of pain are the most characteristic and occur almost always. Their character is intense and sharp, they are not always present, manifesting themselves in attacks. Often, during an exacerbation, a person prefers not to move at all, so as not to provoke increased pain, and remains in this state until the pain subsides. Many compare these manifestations with an electric current that was sent through the body. Typically, an attack of trigeminal neuralgia lasts a matter of minutes, but this usually occurs tens or even hundreds of times a day, which negatively affects the strength and psychological state of the patient.
The location of the pain usually corresponds to the location of the nerve branches in the face. However, in some situations, symptoms are present throughout the face and their specific location cannot be identified, since there is irradiation between nerve branches. If the patient does not take measures and treatment is not carried out, then the area of pain will steadily increase.
Quite often, pain appears after physical provocation of trigger areas. In such cases, a simple press is enough to trigger an exacerbation. Trigger areas on the face include the area:
- Corner of mouth
- Brows
- Bridge of the nose
- Inner cheeks
- Nose
Motor functions
Quite often, trigeminal neuralgia leads to muscle spasms in the face. These symptoms gave the second name to the disease, which is also called pain tic. During an exacerbation, an uncontrolled contraction of the muscle structures responsible for chewing actions, the orbicularis ocular muscles and others occurs. Usually the manifestations are noticeable on the side on which pain and neuralgia are observed.
Reflexes
The presence of reflex disorders that may affect the mandibular, superciliary and corneal zones cannot be independently detected. Only a neurologist can do this when examining a person.
Vegetative and trophic
These symptoms are hardly noticeable at the early stage of the disease; they appear in more advanced cases directly during exacerbation and consist of:
- Severe paleness or redness of the skin of the face
- Increased lacrimation and salivation
- Runny nose
- In advanced stages, swelling of the facial area, falling eyelashes, and dry skin are often observed.
Late stage symptoms
- Pain sensations change in character from paroxysmal to constant
- The entire half of the face, where trigeminal neuralgia is present, immediately hurts
- Anything can cause pain - loud sounds, bright lights, as well as memories of the pathology itself.
Trigeminal neuralgia
N
Trigeminal neuralgia (TN) is a chronic relapsing disease that occurs with remissions and exacerbations of varying duration, individual attacks of which are manifested by sudden, intense, shooting pain in the innervation zones 3, 2 and, extremely rarely, 1 branches of the trigeminal nerve, with a predominance on the right side faces. In European medical literature, the first description of this disease belongs to the Venetian physician Massa (1550), but NTN was identified as an independent nosological form by the English physician John Fothergill (1781) in his monograph “Painful lesions of the face.” In the International Classification of Diseases, 10th Revision (ICD-10), “trigeminal nerve lesions” include “trigeminal neuralgia (paroxysmal facial pain syndrome)”, “atypical facial pain”, “other trigeminal nerve lesions” and “unspecified trigeminal nerve lesions” " The International Headache Society (IHS), in the section on “cranial neuralgias, nerve pain and deafferentation pain,” considers “trigeminal neuralgia” to be “idiopathic” and “symptomatic,” as well as “facial pain not included in this group.”
Views on the etiology and pathogenesis of NTN differed significantly. Until the beginning of the 20th century, the prevailing opinion was that hypothermia of the face, local chronic infections (dental system, maxillary sinuses), meningitis and arachnoiditis of the base of the brain played a decisive role in the origin of this disease. Opinions have been expressed about compression of the peripheral branches of the trigeminal nerve in the narrow and long canals of the facial skeleton. The cause of NTN was assumed to be malocclusion, an unusually high position of the apex of the temporal bone, irritating the trigeminal nerve root, and calcification of the arachnoid membranes. Currently, the generally accepted point of view is that compression of the fifth nerve root at the site of its entry into the medullary pons plays a decisive role in the origin of NTN.
an abnormally tortuous blood vessel (usually the anterior superior cerebellar artery), tumors of the cerebellopontine ganglion (acoustic neuroma, arachnoendothelioma) or multiple sclerosis plaques. It is believed that compression by a pathologically tortuous blood vessel occurs in 88%, by tumors of the cerebellopontine angle in 6% and by multiple sclerosis plaques also in 6%. The pathological mechanism of pain is most convincingly explained by the “gate control” theory of Melzack and Wall (1965). When the trigeminal nerve root is compressed in the area of its entry into the medullary bridge by a pathologically tortuous superior anterior cerebellar artery (less often by another pathological formation), damage to the deep sensitivity fibers of the maxillary and mandibular divisions occurs due to the characteristics of the typical anatomical relationships of sensory fibers in this part of the trigeminal nerve system. Under normal physiological conditions, stimulation of fast-conducting deep sensory nerve fibers inhibits the flow of signals along superficial sensory fibers that conduct pain signals. When the integrity of the nerve fibers is violated, contact occurs between the fibers of the deep and superficial systems, therefore, stimuli that normally cause inhibition of pain signals (movement of the lower jaw, swallowing, etc.), on the contrary, will contribute to an increase in the pain flow in the sensory nuclei of the trigeminal nerve of the brain stem and trigger a typical a signal subjectively felt in the form of pain. Of course, other diverse stem, subcortical and cortical structures also take part in the formation of pain during attacks of trigeminal neuralgia, but the above-described mechanism of pain appears to be the leading one.
According to long-term observations from the clinic of nervous diseases of the dental faculty of the Moscow State Medical and Dental University, women suffer from trigeminal neuralgia more often than men in a ratio of 3:1, right-sided localization occurs in 70%, left-sided in 29%, and bilateral in 1%. The average age of NTN patients entering the clinic for the first time is 55 years, while anamnestic data indicate the onset of the disease 8–10 years earlier. The first attack of pain without any apparent reason occurs in 34%, coincides with dental treatment in 27%, with negative emotions in 17%, in the rest the onset of the disease is accompanied by a variety of factors (sudden hypothermia of the face, respiratory infection, local injuries, etc.) .
Only 23% of patients with NTN develop a full-blown pain syndrome, while the rest have limited, local, low-intensity, shooting, tugging or piercing pain in the alveolar process or medial parts of the face. Such attacks of pain occurred several times a day, without a clear connection with triggering factors or zones. Various types of outpatient therapy (acupuncture, parenteral vitamin therapy, physiotherapy) led to the cessation of pain for an average of 18 months. In some patients, regression of such moderate pain occurred without any treatment.
Full-blown typical pain paroxysm
trigeminal neuralgia is quite characteristic and
consists of several key symptoms:
1. Short-term, never exceeding two minutes (on average 10 - 12 seconds) extremely intense pain of a shooting nature, compared by patients with an electric shock.
2. Between individual attacks of pain there is a “light interval” of varying duration, depending on the nature of the exacerbation.
3. The pain pattern always has a certain extent within the boundaries of the segmental innervation of the trigeminal nerve and does not change significantly with subsequent exacerbations.
4. The presence of trigger zones - hypersensitive areas on the skin of the face (usually in the area of the nasolabial triangle) and in the oral cavity, mild irritation of which leads to a typical pain attack.
5. The presence of triggering factors - actions or conditions under which typical attacks of pain in NTN occur. Most often this is washing, chewing, swallowing, talking, sometimes even a breath of wind.
6. Typical pain behavior. As a rule, during an attack of pain, patients do not cry or scream, but freeze in one position in which the attack catches them and, trying not to move, wait out the painful period. Sometimes they rub the pain area or put pressure on it.
7. Avoid trigger zone irritation. When the patient is asked to indicate it, he does not bring his finger a few centimeters to the hypersensitive area, for fear of provoking an attack of pain, and when the doctor tries to touch this area, he involuntarily recoils.
8. At the height of a painful attack, twitching of the facial muscles may occur, but recently, due to the use of antiepileptic drugs for the treatment of NTN, this symptom is rare.
9. Absence of sensory deficit in the pain area. The exception to this is patients after surgical treatment of NTN.
The traditionally described soreness of the exit points of the trigeminal nerve branches on the face (supraorbital notch, infraorbital and mental foramen) does not have significant diagnostic significance, and the resulting pain attack is associated with stimulation of the trigger zones of the corresponding area of the face.
The first visit at the onset of NTN, as a rule, is to the dentist, since the hypersensitive areas in the vast majority of patients are located not only on the face, but also in the oral cavity. Until the end of the 20th century, when dentists were less familiar with the etiology of NTN, healthy teeth on the side of pain attacks were often mistakenly removed. It should, however, be noted that tooth extraction was carried out at the urgent request of the patients themselves, due to the fact that after the next tooth extraction, painful paroxysms stopped for some time. This phenomenon can be explained from the standpoint of the “pain gate” theory, when irritation of the deep sensitivity receptors of the periodontal tissues leads to the release of inhibitory mediators in the nuclear stem complex of the trigeminal nerve and the temporary cessation of attacks of neuralgia.
During the period of remission, the phobic syndrome
, with the formation of protective behavior, because patients, fearing a relapse of the disease, always eat on the half of the mouth opposite the pain and wrap their heads even in warm weather.
The stage of advanced pain attacks can last for decades with remissions and exacerbations, but over time, in old age, typical neuralgic pain attacks acquire neuropathic features in the form of mild pain, a decrease in the intensity of acute pain, and the appearance of dull constant atypical facial pain.
Apparently, a certain staged nature in the course of NTN is explained by the peculiarities of damage to the trigeminal nerve root under the influence of compression by pathological formations of the cerebellopontine angle.
It should be borne in mind that in case of persistent pain syndrome, the appearance of symptoms of neurological deficit both from the trigeminal and other cranial nerves (especially the facial and auditory), a thorough examination of the structures of the posterior cranial fossa (MRI, auditory evoked potentials, etc.) should be carried out. to identify possible space-occupying lesions and urgent neurosurgical intervention.
The classification criteria of MAIB and MOGB contain descriptive characteristics of atypical pain syndromes of the facial nerve, which are similar in clinical manifestations to NTN. The most important among them are the following:
- Secondary NTN
with lesions of the central nervous system is characterized by sudden, intense, recurring pain in the distribution area of one or more branches of the trigeminal nerve, which in its manifestation does not differ significantly from attacks of typical NTN, except for the longer duration of an individual paroxysm and the rapid addition of sensory deficits. - Symptomatic NTN
occurs, according to our data, in 7% of patients with multiple sclerosis. Clinical manifestations are little different from those of typical trigeminal neuralgia, except for the presence of Lhermitte syndrome of craniocervical localization and trigger factors in the form of head turns.Secondary NTN in facial trauma is characterized by chronic, throbbing, burning pain with paroxysmal intensifying attacks in the distribution areas of the terminal branches of the trigeminal nerve. The pain syndrome is characterized by moderation, duration, and minor trophic disorders occur over time. Chronologically, the onset of the disease coincides with facial trauma, reconstructive surgery, or difficult tooth extraction.
- Postherpetic NTN
is a neuropathy rather than a neuralgia. Chronic sensitivity disorder with a predominance of constant itching over pain is usually localized in the area of the first (ophthalmic) division of the trigeminal nerve. Against this background, short-term, low-intensity shooting pains occasionally occur, spreading from the eyelashes or eyelids to the scalp. Despite the fact that the pain is of moderate intensity, its constant nature, especially in combination with itching, is difficult to bear. Characteristic skin scars are whitish in color against the background of hyper- or depigmentation of the skin in the forehead and anterior scalp. - Glossopharyngeal NTN
manifests itself as sudden, often nocturnal, one-sided, severe, burning pain, recurring pain in the root of the tongue, radiating to the tonsil, pharynx, external auditory canal (auricular or otalgic variant) or to the neck (cervicalgic variant). Triggering factors can be mechanical irritations of the root of the tongue and pharynx (swallowing, ingestion of cold or sour foods).
SUNCT – syndrome
(English abbreviation of the words - short-term, one-sided, neuralgic pain with conjunctivitis and lacrimation). It manifests itself as unilateral, lasting tens of seconds, usually daytime periorbital pain, accompanied by transient conjunctivitis, lacrimation and sweating of the forehead. There is no neurological deficit.
The only effective drug for the conservative treatment of NTN is carbamazepine
(
Tegretol
, etc.). Carbamazepine, synthesized by Schindler in 1957 and introduced into clinical practice for the treatment of NTN by Bloom in 1963, is chemically a derivative of iminostilbene, the ability of which to reduce the permeability of the membranes of neurons involved in nociceptive reactions to sodium and determines its analgesic effect.
Tegretol has an anticonvulsant and at the same time psychotropic effect. It can be prescribed as a primary treatment or in combination with other antiepileptic drugs. The psychotropic effect of Tegretol helps to increase the sociability of patients and their social rehabilitation. In case of essential trigeminal neuralgia, Tegretol in most cases prevents the appearance of paroxysmal pain
. Tegretol causes rapid improvement in mental and autonomic symptoms.
Tegretol is an antiepileptic drug with a half-life of 20–40 hours (with repeated doses and combination therapy with other anticonvulsants, it can be reduced to 8–12 hours), quite completely, but slowly and unevenly absorbed from standard tablets in the upper and lower intestinal tract. tract, reaching the maximum level in the blood serum after 4 to 8 hours. The active substance carbamazepine combines with plasma proteins (about 75%), is almost completely metabolized in the liver and turns into an active metabolite - epoxide, which also has anticonvulsant properties.
Contraindications to this drug are bone marrow diseases, atrioventricular block, hyponatremia, combination with monoamine oxidase inhibitors, lithium drugs, petit epileptic seizures. The effectiveness of carbamazepine is increased by diltiazem, verapamil, nicotinamide, erythromycin, and reduced by valproate, haloperidol, and phenobarbital. The drug is available in the form of tablets of 200 and 400 mg, prolonged-release tablets with a dividing groove of 200 and 400 mg, chewable tablets of 100 mg and in the form of syrup (2%) (bottles of 100 and 250 ml).
For NTN, the following treatment regimen is usually prescribed:
– two days 100 mg 3 times a day (daily dose 300 mg), – two days 200 mg 2 times a day (daily dose 400 mg), – two days 200 mg 3 times a day (daily dose 600 mg) , – three days, 200 mg 4 times a day (daily dose 800 mg).
If there is no analgesic effect, they move on to higher dosages - 1000 and 1200 mg per day, divided into 4-6 doses. The recommended starting dose for elderly patients is 100 mg 2 times a day. When a sufficiently pronounced result is achieved, you should stop at the appropriate daily dose for a month and then also slowly reduce the effective dose. Treatment with carbamazepine at this amount must be continued without interruption for at least six months, and then transferred to maintenance doses (200–400 mg per day in two doses). Recently, carbamazepine (Tegretol) is produced in syrup, which is well tolerated by patients with NTN.
Tegretol tablets and syrup should be taken with or after meals with a small amount of liquid. The syrup should be shaken before use. Chewable tablets should be taken after meals with a small amount of liquid. Swallow extended-release tablets (either whole or, if so prescribed, only half) with or after meals with a small amount of liquid, without chewing them. Chewable tablets and syrup are especially suitable for patients who have difficulty swallowing tablets. Due to the slow, controlled release of the active substance from the scored tablets, the daily dose can usually be taken in 2 divided doses. Before starting treatment, it is necessary to conduct a study of liver function and blood picture. Subsequently, blood tests should be performed weekly during the first month of treatment and then monthly. Liver function should be monitored periodically. Non-progressive or persistent asymptomatic leukopenia, which is often observed, generally does not require discontinuation of the drug. However, Tegretol treatment should be discontinued if progressive leukopenia or leukopenia accompanied by clinical symptoms such as fever or sore throat occurs. The drug is well tolerated. In some cases, especially at the beginning of treatment, side effects such as loss of appetite, dry mouth, vomiting, diarrhea, constipation, headache, dizziness, drowsiness, ataxia, accommodation disturbances, diplopia may be observed; confusion may occur in older people and excitement. These side effects usually disappear after 7–14 days on their own or after a temporary reduction in the dose of Tegretol.
A less effective drug than carbamazepine, but still having a fairly pronounced analgesic effect, is phenytoin
. Phenytoin is prescribed 2-3 tablets per day, contraindications are liver and kidney dysfunction, cachexia, heart rhythm disturbances, porphyria. Among the adverse reactions, the most common are agitation, vertigo, gingival hyperplasia, Dipuytren's contracture, etc. The effectiveness of this drug is increased by propanolol and chlordiazepoxide, and reduced by steroids, folic acid, and haloperidol.
In a number of patients with NTN, some other drugs have an analgesic effect, a number of decreasing effectiveness of which is presented as follows - carbamazepine, phenytoin, clonazepam, valproic acid.
During the period of exacerbation of NTN, intravenous (more effective drip) administration of sodium hydroxybutyrate
, 5 ml of a 20% solution twice a day (hypokalemia is a contraindication), intravenous jet injection
of nicotinic acid
1%, starting from 1 ml, with a gradual increase to the “ignition” effect (usually 6–8 ml) and a decrease to the original dose.
During the period of exacerbation, hydrocortisone ultraphonophoresis, laser puncture on pain points, and classical acupuncture are used.
For concomitant spastic conditions accompanied by pain syndrome due to NTN, antispastic drugs - muscle relaxants - are used. One of the representatives of this group is tizanidine (Sirdalud)
. Sirdalud is a centrally acting muscle relaxant. By stimulating presynaptic a2-adrenergic receptors, it leads to inhibition of polysynaptic transmission of excitation in the spinal cord, causing muscle hypertonicity. The drug is effective for moderate to severe pain, especially when the pain intensifies during the night. The drug is well tolerated. The dose is selected individually over 2–4 weeks. and is 2–6 mg/day.
If conservative therapy is ineffective, neurosurgical treatment methods
– retrogasseral thermorizotomy, microvascular decompression of the trigeminal root, etc.
Diagnostics
If there are signs of trigeminal neuralgia, the main one of which is pain in the facial area, then it is important not to delay visiting a neurologist for diagnosis, since in the absence of treatment the disease progresses very quickly. The first step is to evaluate the symptoms and take an anamnesis. The second mandatory stage is a neurological examination with testing of reflexes and sensitivity of various parts of the head. If the disease is in remission, its diagnosis becomes much more difficult. In such conditions, pathologies can only be identified using an MRI of the head.
Additional diagnostic methods include:
- Dental examination, since neuralgia often occurs against the background of dental damage, poor-quality installation of dentures, and so on. In this case, the cause can be identified using a panoramic X-ray of the head, which will help identify pinching of the trigeminal nerve.
- Electromyography, which shows the passage of electrical impulses along nerve endings.
- General blood test, which excludes or confirms the viral origin of neuralgia
Treatment at home
Doctors categorically do not advise treating facial neuralgia using folk remedies at home. Traditional medicine and homeopathy have the right to life in this case, but only on the condition that they will be part of a therapeutic complex that was developed and approved by the attending physician.
The most common folk remedies used for this pathology include:
- Acacia infusion (to be smeared twice a day on the skin located above the painful area).
- Mumiyo ointment (used internally and externally).
- Applications of ointment made from black poplar buds.
- Tincture of red rose petals.
Treatment
Depending on the degree of damage to the trigeminal nerve and, accordingly, how severe its neuralgia is, treatment is prescribed using various methods:
- Physiotherapeutic
- Medication
- Surgical intervention
The first two methods are usually combined, and the third is used if there is no effect from conservative therapy.
Photo 3. Treatment with physiotherapy
With physiotherapeutic treatment, treatment is carried out:
- Dynamic currents
- Electrophoresis
- Laser therapy
- Ultraphonophoresis
Drug therapy includes taking, as prescribed by a doctor, the following drugs that have anticonvulsant and antispasmodic effects:
- Finlepsina. This remedy is used quite often, as it is a very effective anticonvulsant that relieves neuropathic pain
- Carbamazepine
- Baclofen
- Gabapentina
- Sodium hydroxybutyrate
- Trentala
- Nicotinic acid
- Vitamna B
- Glycine
If conservative treatment fails to achieve results, then surgical treatment is prescribed, which can be carried out using the following method:
- Percutaneous balloon compression
- Microvascular decompression
- Glycerin injections
- Radiofrequency ablation
- With ionizing radiation, due to which the trigeminal nerve is partially destroyed in the affected areas
- The use of ionizing radiation to destroy the affected nerve.
ICD-10 code – G50 Trigeminal nerve lesions
Neuralgia of the glossopharyngeal nerve - description, symptoms (signs), treatment.
Short description
Glossopharyngeal neuralgia is a rare disease affecting the IX pair of cranial nerves (glossopharyngeal nerve), characterized by the appearance of paroxysmal pain on one side of the root of the tongue, pharynx and soft palate when eating hot, cold or solid food, talking, yawning or coughing.
Code according to the international classification of diseases ICD-10:
G52.1 Lesions of the glossopharyngeal nerve
Frequency - 0.16:100,000; men get sick more often. Etiology • Usually unknown • Tumors (nasopharyngeal or intracranial, pharyngeal cancer) • Trauma • Cicatricial changes in the nerve root • Osteophytes of the jugular foramen • Aneurysms.
Symptoms (signs)
Clinical picture • Paroxysms of acute pain of a tugging, drilling, stinging nature, lasting up to several tens of seconds • Trigger zones - root of the tongue, palatine tonsil, palatine arch • Pain is provoked by swallowing, especially hot or cold food, as well as coughing, laughter • Often radiates to the ear , pharynx, behind the angle of the lower jaw • May be accompanied by fainting states (as a result of excessive stimulation of the parasympathetic nervous system) against the background of bradycardia, a drop in blood pressure - swallowing syncope.
Treatment
Treatment • The drug of choice is carbamazepine 400–1200 mg/day. • Second-line drugs •• Phenytoin 300–600 mg/day •• Baclofen 10–80 mg/day; start with 5–10 mg 3 times a day (as adjuvant therapy with phenytoin or carbamazepine) •• Valproic acid. • Surgical treatment is indicated only when surgically correctable causative factors are identified (see Etiology).
Synonyms • Glossopharyngeal neuralgia • Weisenburg–Sicard–Robineau syndrome • Sicard syndrome
ICD-10 • G52.1 Lesions of the glossopharyngeal nerve
Consequences
The neglected condition and lack of treatment for trigeminal neuralgia, in addition to annoying and exhausting symptoms, results in the following consequences and complications:
- Partial or complete paralysis of the facial muscles
- Hearing loss
- Severe facial asymmetry
- Deep damage to the nervous system
Photo 4. Consequences for the face
The highest rate of development of negative consequences is observed in groups of older patients - more often women than men - who have cardiovascular diseases and metabolic problems.
Treatment options
If neuralgia occurs, do not self-medicate, but immediately seek help from a doctor. He will determine the exact cause of the disease and prescribe an adequate course of treatment, which may include means and methods that we will consider below.
Medication
Medicines for the treatment of neuralgia:
- Muscle relaxants are medications that relieve muscle hypertonicity (mydocalm, baclofen).
- Anticonvulsants (tebantin, finlepsin).
- Anti-inflammatory and analgesic ointments (piroxicam, apisatron).
- Vitamin complexes.
Physiotherapy
The following procedures are prescribed:
- Electrophoresis.
Simultaneously with the effect of electric current on the patient’s body, B vitamins and painkillers are injected intramuscularly. Used as one of the main methods of treating neuralgia. This method is suitable for people who have problems with the gastrointestinal tract, and taking pills is undesirable. - Light therapy. Treatment with bright light from an artificial source is indicated for patients who cannot cure the disease for a long time.
- UHF. Exposure of the body to a high-frequency magnetic field helps to warm up the affected tissues. The method is indicated at the final stage of therapy.
- Darsonval. A special drug conducts a high-frequency, low-power current pulse through the affected areas, which improves blood supply and tissue nutrition. Often used for intercostal neuralgia.
- Fluctuarization. Exposure of affected tissue to fluctuating current reduces pain and enhances tissue regeneration.
Prevention
As we noted above, the nature of the development of trigeminal neuralgia can be internal or external. It is impossible to influence many internal factors; for example, it is impossible to correct congenital narrow canals, but external causes that most often lead to pathology can and should be influenced.
To avoid nerve disease you should:
- Do not expose the head and especially the facial area to hypothermia, which is especially critical in winter
- Avoid head injury
- Do not start and respond in a timely manner to various pathologies that can provoke the neuralgia in question, for example caries, sinusitis, tuberculosis, herpes, etc.
If it so happens that a person develops an illness, then under no circumstances should it be left to chance. You must definitely go to a medical facility and fully undergo the treatment that will be prescribed.
What is neuralgia, types of disease
Neuralgia is a disease of the peripheral nervous system, which is manifested by severe pain, the pain is localized along the affected nerve. In severe cases, sensation and motor function may be impaired.
There are several classifications of neuralgia:
By etiology (origin):
- Primary (essential) – as a rule, the cause of such pain cannot be determined;
- Secondary (symptomatic) - are not an independent disease, but just a symptom of others.
By localization:
- Limbs;
- Faces;
- Torso.
The most common types of neuralgia are:
- Trigeminal nerve;
- Intercostal nerves;
- External cutaneous nerve of the thigh;
- Pterygopalatine ganglion;
- Glossopharyngeal nerve;
- Occipital nerve.