The essence of the problem
Progressive multiple sclerosis (PMS), as a severe form of this demyelinating disease, is classified into primary progressive multiple sclerosis (PPMS) and secondary progressive multiple sclerosis (SPMS). The first is true when the course of the disease continues to worsen by the time it is diagnosed (15% of cases). The second begins as relapsing-remitting multiple sclerosis (RRMS), which eventually develops into SPMS in 80% of patients.
The vast majority of drugs offered by the pharmaceutical industry that modify the course of multiple sclerosis (MDMS) are aimed at treating RRMS as its most common form (85% of primary diagnoses). Thus, Ocrevus (ocrelizumab), promoted by Roche, declares that it is suitable for the treatment of patients with both RRMS and PPMS. And if in relapsing-remitting multiple sclerosis ocrelizumab is indeed a highly effective DMT (although by no means unconditionally), then in the case of primary progressive multiple sclerosis it is not yet possible to call Ocrevus really working. Even the US Food and Drug Administration (FDA) approved ocrelizumab for PPMS with great reluctance, apparently due to the lack of any other treatment options. However, the Swiss pharmaceutical giant continues to seek evidence that its monoclonal antibody against CD20 can also treat PPMS.
Novartis offers Mayzent (siponimod), which is suitable for patients with SPMS, but only in the active form, that is, when the inexorably progressive disease continues to be characterized by periods of relapse. Alas, siponimod could not achieve the same acceptable efficacy as in RRMS for patients with SPMS.
Ocrevus and Mayzent only slightly curb the worsening disability in progressive multiple sclerosis: a tiny 6 percent difference from placebo will never be considered evidence of a fundamental change in the course of the disease.
According to global statistics, the global population of patients with multiple sclerosis breaks down as follows: RRMS accounts for 57% of patients, while PMS covers 43%, including 15% of patients with PPMS and 28% with SPMS.
The medical need for new breakthrough and, most importantly, highly effective drugs for the treatment of progressive multiple sclerosis still remains unmet. The community of doctors and patients dreams of either reversing disability, followed by sustainable maintenance of the gains achieved, or at least a stable stop in the progression of multiple sclerosis.
First signs
For many, the first signs of multiple sclerosis appear in what doctors call clinically isolated syndrome (CIS). This episode of neurological symptoms usually lasts 24 hours.
There are two types of CIS:
- Monofocal episode: You have one symptom.
- Multifocal episode: You have more than one symptom.
The most common symptoms in CIS are:
Optic neuritis. Usually only one eye is affected, but in rare cases both can be affected.
Main manifestations:
- blurred vision;
- faded shades;
- pain in the eyes, especially when moving.
Numbness and tingling.
Main manifestations:
- sensation of electric shock when moving the head or neck. it may move along the spine or into the arms or legs;
- numbness in the face;
- tingling in the legs.
Not everyone who has CIS will get MS . The likelihood is higher if there is damage to the brain from loss of myelin.
The hypothesis that found the answer
Atara Biotherapeutics is working on the theory that the Epstein-Barr virus is closely linked to the development of multiple sclerosis. And to do this, she is developing therapies based on T cells, as critical components of the body's immune system that selectively target specific viral antigens. Targeted T cells recognize and eliminate Epstein-Barr virus-infected B lymphocytes and plasma cells from the central nervous system. The result of modulating the pathophysiology of multiple sclerosis is the prevention of subsequent autoimmune attacks and the opening of the possibility of restoring the central nervous system through the mechanisms of remyelination, dendritic and axonal sprouting (proliferation), and synaptic remodeling.
Atara's achievements, supported by clinical trial data, confirm that its hypothesis is correct. Moreover, the demonstrated clinical effectiveness of the experimental treatment of progressive multiple sclerosis is incredible, because it was possible not only to stop the worsening of an already serious disease, but also to reverse it.
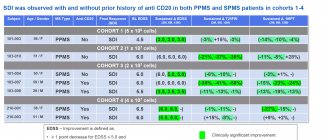
Atara is conducting clinical trials of ATA188, a T-cell immunotherapy containing cytotoxic T-lymphocytes against specific protein antigens of the Epstein-Barr virus (EBV). Experimental ATA188 is allogeneic and is produced ahead of time by in vitro cultivation:
The scales are as follows:
- Fatigue Severity Scale (FSS): minimal clinical improvement was −0.7 points;
- Multiple Sclerosis Impact Scale (MSIS-29) [physical ability domain]: −8 points;
- T25-FW: −20%;
- 9-HPT: −20%;
- subjective mobility questionnaire (MSWS-12): −8 points;
- EDSS: −1 point (with initial EDSS 3–5 points) and −0.5 points (EDSS 5.5–7.0);
- Visual acuity (VA) [LogMAR]: minimum −0.1 change in each eye.
It has been confirmed that the long-lasting declared therapeutic efficacy of ATA188 directly correlates with increasing dosage of the drug.
Based on the results, Atara selected dose cohort 3 for study in part 2 of the clinical trial. It is possible that participants from the maximum dose cohort 4 will subsequently join as soon as their 12-month data is ready.
The safety profile of ATA188 is characterized by the absence of dose-limiting toxicity and fatal adverse reactions. All negative phenomena associated with therapy were mild to moderate in severity. Although one patient experienced a severe adverse reaction that led to withdrawal from the clinical trial, it occurred amid ongoing symptoms of an upper respiratory tract infection and possible dental infection. Runny nose was the only adverse reaction recorded in more than one subject.
ATA188 had no clinically significant effect on cytokine production, including cytokine release syndrome.
Definition
Multiple sclerosis (MS) is a chronic neuroimmunological (both nervous and immune systems are affected) autoimmune disorder involving the brain, spinal cord, and peripheral nerves.
Through a mechanism that is not entirely understood, the protective insulating substance called the myelin sheath that covers the nerve is destroyed. The disease gets its name “multiple sclerosis” because the inflammatory attacks, which cause characteristic scars (plaques or spots) of the myelin sheath, manifest themselves unpredictably, vary in intensity, and occur in different parts of the nervous system.
The course of the disease is paroxysmal - periods of exacerbation are followed by periods of remission. The randomness of the location of the next injury can lead to a wide range of neurological symptoms, which can vary from person to person. It has recently become known that the nerve fibers themselves (axons), in addition to the myelin sheaths, are also affected early in the disease process.
Without treatment, the disease leads to permanent disability over several years.
More than hope
And although the development of multiple sclerosis is probably driven by more than one causative factor, the Epstein-Barr virus is the only risk factor known to date that is necessarily necessary for the manifestation of the disease. It has been proven that 100% of patients with multiple sclerosis have been exposed to EBV. At the same time, EBV-infected cells, especially memory B cells, which have become immortal due to viral infection, play, it is believed, a critical role in the immune cascade responsible for relapsing and progressive forms of multiple sclerosis. The success of existing pharmacotherapy, which depletes the pool of all peripheral B cells, once again demonstrates the key position of these cells in the pathophysiology of multiple sclerosis. The justification for continuing experiments with the treatment of multiple sclerosis using ATA188, cytotoxic T cells selectively targeted against EBV-infected B cells and plasma cells, both circulating in the body and persisting in the central nervous system, has been shown.
Some observations are that the effectiveness of ATA188 in improving disability status appears to depend on the initial EDSS score: the more advanced the disease, the less (or slower) the healing power of the treatment appears. Still, even a one-point improvement in the EDSS score is remarkable. After all, if the patient, for example, initially walked with a cane, then after ATA188 therapy he gained the ability to walk independently.
Clinical trials of autologous ATA190, which Atara abandoned due to manufacturing difficulties, highlighted the fact that in patients with severe neurological disability (baseline EDSS score 8.0), irreversible axonal degeneration and neuronal loss limit therapeutic options for improvement. even if autoimmune attacks on the central nervous system are prevented by EBV-specific T-cell therapy. Nevertheless, even in such advanced patients, treatment had a beneficial effect on the general condition, physical and cognitive abilities, as well as on the physiological plane, including bladder function, visual acuity, and spasticity.
Available medications can only slightly slow down the worsening of progressive multiple sclerosis—they cannot stop or reverse the disease. If ATA188 achieves this in a rigorously controlled Part 2 clinical trial, we are in for an evolution in the treatment paradigm for progressive and other forms of multiple sclerosis.
Diagnostics
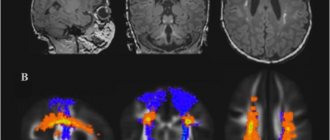
Multiple sclerosis (MS) is diagnosed based on clinical findings and supporting data from ancillary tests, such as magnetic resonance imaging (MRI) of the brain and spinal cord and cerebrospinal fluid examination. Clinically, the attack must be compatible with the pattern of neurological deficits seen in MS, which usually means that the duration of the deficit is several days to several weeks.
Traditionally, MS could not be diagnosed after only one symptomatic episode because diagnosis required repeated attacks involving lesions separated in time and space. And before, doctors could only “sit and wait” for the disease, after one episode, to “make itself known” again.
The Macdonald criteria, expanded and modified in 2021, make it possible to diagnose MS even with the first clinical episode.
This early diagnosis is important because axonal loss can occur even in asymptomatic patients in the early stages of the disease. Studies of patients treated with interferon with a first attack of neurological symptoms suggestive of MS have demonstrated a reduction in disability and a reduction in the incidence of secondary relapses.
Multiple sclerosis and Epstein-Barr virus
Genetic and environmental factors are believed to contribute to the risk of developing multiple sclerosis, a chronic inflammatory demyelinating disease of the central nervous system that causes progressive disability. Over the past four decades, there has been growing evidence that Epstein-Barr virus (EBV) plays a significant role in the development of multiple sclerosis. The assumption is supported by a number of independent studies indicating the universal presence of infection in patients and the presence of high titers of serum antibodies against EBV both during the clinical course of multiple sclerosis and before its manifestation.
Epstein-Barr virus (EBV) and multiple sclerosis: the autoreactive B-cell hypothesis. Image: Trends Mol Med. Mar 2021; 26(3): 296–310.
Epstein-Barr virus, or human herpes virus type 4 (HHV-4), is unique in many ways. Thus, in order to colonize the body, it infects B-lymphocytes, activates and promotes their clonal reproduction, and then throughout a person’s life it persists as a latent infection in memory B-cells that carry the phenotype of resting cells. The virus, switching from latent (sleeping) to lytic (replicating) form through modulation of its nuclear genes, latent membrane proteins (LMP) 1, 2A and 2B and the viral early early protein BZLF1 (ZEBRA), is reactivated in plasma cells and epithelial cells of the tonsils, organizing own transmission to other organisms through saliva and genital secretions. Although this double-stranded DNA gammaherpesvirus infects approximately 95% of the world's adult population, the number of EBV-infected cells in the body is kept under strict immune control, including EBV-specific cytotoxic CD8+ T lymphocytes, which destroy proliferating and lytically infected cells. cells.
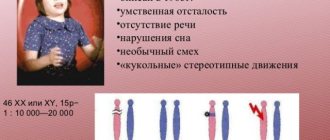
In some cases, immunological surveillance of EBV weakens, which is reflected in the development of various diseases. The Epstein-Barr virus is known to cause infectious mononucleosis. It is associated with certain cancers, including Hodgkin's lymphoma, Burkitt's lymphoma, gastric cancer, and nasopharyngeal carcinoma. Epstein-Barr virus is associated with childhood disorders such as Alice in Wonderland syndrome and acute cerebellar ataxia. It is believed that it increases the risk of developing autoimmune pathologies, including dermatomyositis, systemic lupus erythematosus, rheumatoid arthritis, and Sjogren's syndrome.
In relation to multiple sclerosis, in susceptible hosts, EBV infection is thought to endow infected autoreactive B cells with an abnormal ability to survive and proliferate. Such latently infected cells accumulate in the lymphoid structures and target organs affected by this disease. In the brain, this leads to the constant production of autoantibodies that attack and damage oligodendrocytes, myelin and neurons.
Atara's analysis of post-mortem brain samples from patients with multiple sclerosis and healthy controls (without neurological disease) found that despite evidence of Epstein-Barr virus infection in both groups, EBV-positive immune cells were more common and densely populated in the brain. the brain of patients with multiple sclerosis.
Atara specialists, using immunohistochemistry, in situ hybridization, optical microscopy and semi-quantitative analysis, studied post-mortem brain biopsies from patients with multiple sclerosis (n=17) and healthy individuals (n=9). The presence of LMP-1 was found in 93% of biopsies from the multiple sclerosis group and 78% of the control group, while the former showed a significantly greater presence of CD138+ plasma cells and LMP-1-enriched cell populations.
Remarkably, 78% of chronic areas of brain damage in multiple sclerosis and only 33.3% of healthy brain samples contained CD138+ plasma cells in parenchyma where they should not be. It is possible that EBV infection is responsible for the extravasation of the latter from the vascular network of the brain, endowing the inflammatory process with persistence.
In 46% and 44% of tissues, respectively, the BZLF1 protein was found, despite the fact that in the case of biopsies with multiple sclerosis, it was predominantly associated with areas of chronic brain damage. BZLF1 is thought to be able to suppress the production of interleukin 2 (IL-2) and interleukin 6 (IL-6). In addition to participating in B-cell maturation, IL-6 is important for neuro- and oligodendroglial genesis under normal conditions and after injury.
In addition, in 85% of brain samples from patients with multiple sclerosis, there was a much more pronounced presence of immune cells with EBV-encoded small RNA-1 (EBER1) than in biopsies from healthy individuals.
Prevention of ARVI
With multiple sclerosis, it is better to prevent a cold than to treat it later. For these purposes it is used:
- Frequent hand washing (after returning home from the street or contact with money);
- Avoid contact with people who have ARVI and do not visit places with large numbers of people during the epidemic;
- Take vitamins;
- If someone in the family has contracted a cold, then this person needs to start a course of treatment with amixin;
- Eat well;
- Avoid stress and get enough sleep;
- Annual flu vaccination.
If you follow the above recommendations, you can avoid both ARVI and another exacerbation of multiple sclerosis.
Additional evidence
Antiviral therapy for multiple sclerosis is being pursued by the Swiss-French company GeNeuro with its experimental temelimab. According to one hypothesis, some viruses can give impetus to the development of multiple sclerosis.
Thus, multiple sclerosis-associated retrovirus (MSRV), which belongs to the pathogenic W family of human endogenous viruses (pHERV-W), can be transactivated by external factors, for example, human herpes virus type 6 (HHV-6) or Epstein-Barr virus. The result is the generation of the pathogenic envelope protein MSRV-Env, which, by overactivating the endogenous toll-like receptor 4 (TLR4), triggers a pro-inflammatory cascade and suppression of remyelination.
Temelimab (GNbAC1) is a recombinant humanized monoclonal antibody that selectively targets the extracellular domain of MSRV-Env for its neutralization.
What not to take if you have MS
With this disease, especially its severe forms, the following medications should not be taken (they can worsen the patient’s condition and cause an exacerbation of the disease):
We also recommend: Treatment of influenza in diabetes mellitus
- Drugs with a pronounced immunostimulating effect that will promote the activation of phagocytosis.
- Preparations based on echinacea.
- The drug Indomethacin and its derivatives.
Stress, strict dieting, excessive exercise and fasting can also worsen the condition.
Excessive physical activity is contraindicated
Wash your hands!
It would seem like a simple preventative measure.
Soap and water kills most germs in about 15 seconds, but it takes longer than you might think. Try saying the numbers from 21 to 36 out loud while washing your hands. Usually, this procedure took you less time, didn’t it? After you have washed your hands, try not to touch the tap. This recommendation is especially important if you are in public spaces or if you have a sick person at home. By touching the tap with clean, damp hands, you risk reintroducing viruses to them. So try to use your elbow, forearm or paper towel to cover the water.
An alternative to soap and water is alcohol-based hand sanitizers. They do not need to be washed off, so they can always be on your desk, in your purse or briefcase, or in your car.
Cough cough...
Since childhood, many of us have been taught: “when you cough, cover your mouth... with your hands.” But such manipulation is a direct path to the spread of infection. When you cough or sneeze, viruses are released in your saliva and sputum. Covering our mouths with our hands, we “collect” them on our palms, and then...we greet employees with a handshake, take hold of pens, phones, dishes, etc., allowing viruses to freely find new “victims.” If you or your counterpart coughs or sneezes, try to cover your mouth and nose with disposable paper handkerchiefs, which can be thrown away immediately!
The Japanese walking around during a flu epidemic wearing masks (which must be changed every two hours) evokes sarcastic smiles. But their common sense is worth learning from.
This is how a small “set of rules for the prevention of influenza and ARVI” turned out, which will be useful not only for PC users. Follow the rules of personal hygiene, try, if possible, to limit contact with other people for a while, drink more fluids, do not deny yourself positive emotions and be healthy!
Source