Status epilepticus is a condition characterized by frequently recurring or continuous epileptic seizures lasting up to half an hour.
Moreover, each new seizure occurs earlier than the patient manages to recover from the previous one. During the time between attacks, consciousness remains unclear, and signs of coma persist, which are characterized by impaired blood flow through the vessels and respiratory dysfunction.
Epistatus is the most common neurological condition. The incidence of this pathology is approximately 20 cases per 100,000 people.
In half of the cases, ES occurs in young children. Among people suffering from epilepsy, this condition is more common in children than in adults (in a ratio of 15-25% to 5%).
About 7% of patients with epilepsy have a history of one to three epilepsy attacks throughout their illness.
What is the provoking factor?
The main reason for the occurrence of epileptic seizures is the withdrawal of medications taken, the action of which is aimed at suppressing epileptic seizures.
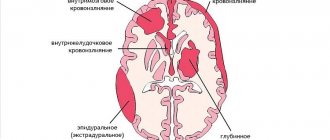
However, status epilepticus can occur not only against the background of epilepsy, but also due to brain lesions, including:
- head injury;
- intoxication;
- intracranial malignant tumor;
- circulatory disorders in the brain;
- infection;
- dropsy of the brain (encephalopathy);
- withdrawal syndrome;
- complications of diabetes;
- hematoma.
The incidence of epistatus without a predisposing factor - epilepsy is approximately 50%.
Causes
The exact cause of epilepsy is unknown. Hereditary factors have been suggested as a possible cause of essential epilepsy. Some types of epilepsy occur as a symptom of other diseases, while others are thought to be caused by head injuries. There may be a genetic predisposition to epilepsy in some families, but scientists do not understand the hereditary factors that can make a person vulnerable to seizures.
The most common causes of recurrent seizures in infants include:
- genetic inborn errors of metabolism;
- other metabolic disorders;
- brain developmental defects;
- injuries received several months before childbirth or several weeks after childbirth (perinatal);
- acute lack of oxygen (hypoxia).
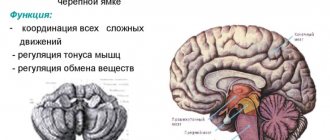
Types and stages of epistatus
The variability of the types of epileptic seizures determines the formation of various clinical forms of epileptic seizures. They are divided into two main groups - convulsive and non-convulsive seizures.
According to the classification, the following types of status epilepticus are distinguished:
- Generalized SE - characterized by widespread tonic-clonic convulsions with an unconscious state.
- Not completely generalized ES - characterized by atypical muscle spasms with complete loss of consciousness. Tonic status is most common among children with Lennox-Gastaut syndrome. Can be observed at different ages. Clonic status is observed with epilepsy in infants, as well as with convulsions with high fever in young children. Myoclonic status is characterized by constant or episodic muscle twitching.
- The status of focal paroxysms proceeds according to the type of Jacksonian epilepsy with muscle contraction of a certain localization, for example, only the muscles of the face, one limb or half of the body. In this case, loss of consciousness may not occur.
- Absence or non-convulsive status is accompanied by a complete loss of consciousness without muscle contractions. Such attacks are characterized by the mildest course, however, due to the absence of seizures, diagnosis can be difficult.
- Partial status is characterized by unconscious and automatic actions with complete or incomplete loss of consciousness.
The stages of development of epistatus are also distinguished:
- pre-status - lasts 1-10 minutes;
- initial - lasts from 10 minutes to half an hour;
- expanded - lasts from half an hour to an hour;
- refractory - lasts more than an hour.
Diagnostics
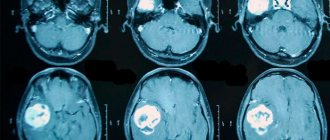
Full-blown status epilepticus is detected as 2 or more generalized seizures without full recovery of consciousness between or as a single prolonged seizure. When classic seizures occur, the condition does not become complicated.
A common mistake is made during underdiagnosis as a result of a false impression formed. Patients regain consciousness between attacks. Various states, apart from vigorous wakefulness, are considered a sign of an anomaly and indicate epistatus.
It is necessary to take into account the possible asymmetry of the results of diagnostic procedures. Experts often diagnose partial ES in patients with problems with consciousness and repetition of unilateral muscle contractions. In such situations, asymmetrical and unilateral motor manifestations often occur when patients are partially unconscious in a convulsive state.
EEG monitoring is required for the normal management of patients with status epilepticus. Therapy should not be delayed for a long period until the desired results are achieved. When the seizures end and patients always regain consciousness, there is no need for an EEG.
When a patient's consciousness changes, regardless of a decrease in the intensity of seizures, it is necessary to reduce epileptroform discharges through EEG equipment.
What does it look like in real life
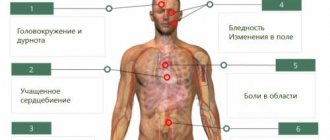
Symptoms of status epilepticus are determined by severe disorders in consciousness, respiratory system and hemodynamics, which are caused by a previous attack; the number of seizures during epileptic status can range from 3 to 20 per hour.
Consciousness by the time of the next attack does not clear up and the person is in a state of stupor, numbness or coma.
With prolonged ES, the comatose state worsens, becomes deeper, convulsions take on a tonic form, an increase in blood pressure is replaced by a sharp decrease, and increased reflexion is replaced by a lack of reactions. Hemodynamic and respiratory disorders become more pronounced.
The convulsions may disappear, and then the stage of epileptic prostration begins, which is characterized by external changes:
- pupil size changes;
- the gaze becomes unconscious;
- mouth slightly open.
It is very dangerous! In this condition, death can occur.
Epistatus necessarily lasts more than half an hour. This condition should be differentiated from episodic attacks, during the intervals between which there is a complete or almost complete clearing of consciousness, as well as a partial restoration of the patient’s physiological state.
The course of convulsive SE can be divided into two phases. At the first stage, compensatory changes occur to maintain blood circulation and the metabolic process.
This condition is characterized by:
- tachycardia;
- high blood pressure;
- vomit;
- involuntary urination;
- involuntary defecation.
The second phase occurs after half an hour or an hour and is characterized by a breakdown of compensatory changes. In this state, the following processes occur:
- lowering blood pressure;
- arrhythmia;
- respiratory dysfunction;
- thrombosis of the pulmonary artery and its branches;
- acute renal and liver failure.
Non-convulsive epistatus is characterized by various disorders of consciousness:
- feeling of detachment;
- immobilization.
In the case of ES of complex partial seizures, the following is observed:
- behavioral deviations;
- confusion;
- symptoms of psychosis.
Status epilepticus from A to Z:
Diagnostic measures
Status epilepticus requires emergency care, so it must be diagnosed as quickly as possible.
To make a diagnosis, the following play a decisive role:
- Collected epileptic history, if the patient has this pathology. The medications taken and their dosages are specified.
- Typical clinical picture.
- Data indicating injuries, intoxications, and so on.
- Biochemistry of blood, study of its gas composition, urine analysis, determination of alcohol content in the blood. These are additionally performed to assess the somatic condition and the reasons that led to the development of a seizure.
- Monitoring of electroencephalogram and blood pressure.
To determine non-convulsive forms, the electroencephalogram is the most informative.
Computed tomography and magnetic resonance imaging are carried out to accurately identify structural changes in the brain, damage, the presence of tumor formations, hemorrhages in the membranes, and so on.
Epistatus is dangerous for human life, so the diagnosis must be made correctly and quickly, even before hospitalization.
First aid - rules and tips
The main goal when providing first emergency care in case of epistatus before the arrival of doctors is to prevent damage and trauma to the patient.
What to do during an attack:
- lay the person on a comfortable surface to reduce the risk of injury;
- remove those items of clothing that may cause discomfort (for example, a tie, a belt), unbutton the collar;
- place rolled clothing under your head;
- carefully turn your head to the side so that the patient does not choke on his saliva;
- if your mouth is slightly open, you need to put a handkerchief or some kind of cloth between your teeth, but in no case a sharp object, so as not to break your teeth;
- remove all dangerous objects that are in the immediate vicinity to avoid injury;
- do not hold the person too tightly, otherwise there is a high risk of broken bones;
- do not open your teeth if they are clenched.
Status epilepticus: clinical picture
Status epilepticus is formed when certain rules for caring for patients with epilepsy are not followed or in the case when an individual independently does not follow absolutely any or some instructions.
The epileptic seizure itself does not have obvious clinical features that would differentiate it from a generalized seizure with classic tonic convulsive and clonic contractile phases. And yet, in such a situational picture there are some differences; with status epilepticus, the person does not return to a conscious state, but experiences large generalized seizures over and over again. In order to distinguish such attacks, it is worth describing a classic generalized seizure, which consists of two phases:
• Tonic phase, which lasts up to half a minute and has severe consequences. The cramp affects every muscle of the person’s body, which refers not only to the external muscles, but also to the internal muscles, mainly the skeletal muscles are affected. Mostly, convulsions are observed in the extensor muscles, the eyes roll back and are fully open, and the mouth is half open. Cramps begin in the muscles of the trunk and then move to the limbs.
• The clonic phase has short-term contractions of the muscles - flexors of the trunk and limbs with twitching relaxation. Duration is up to three minutes. It should be noted that many generalized seizures may have predictors that entail changes in mood, emotional state, headaches and severe deterioration of the condition. Sometimes a seizure begins with an aura in the form of stereotypical short-term disorders, which can manifest themselves in a variety of specific pathologies. Sometimes it is sweating or hyperemia, sometimes you may feel dizzy or feel nauseous.
In a generalized seizure with tonic and clonic phases, there are characteristic signs, namely mydriasis with areflexia, that is, lack of reactivity of the pupils to light stimuli, essentially symptoms of coma. Due to hypersalivation and severe clonic convulsions, foam appears at the mouth and the risk of biting the tongue increases. Due to the fifteen-second coma at the time of the attack, which can be prolonged during status epilepticus, muscle atony is formed, which leads to the involuntary release of feces or urine. When checking the reflexes, complete areflexia will be revealed, which will be restored only with the return of consciousness, moreover, both deep and superficial reflex mechanisms are reduced. At the same time, between groups with phases of tonic and clonic convulsions, consciousness does not return, which greatly aggravates the condition. Such persons require transport to intensive care because the mortality rate is too high.
Status epilepticus is characterized as a severe complication with an acute threat to life.
Reasons for status epilepticus other than those that cause epilepsy itself:
• Convulsive status epilepticus can be provoked by inadequate treatment, especially the prescription of incorrect drugs and the use of inappropriate doses. Considering that patients often self-manage, canceling or reducing the dose of their chosen drugs, then compliance with the patient plays the most important role in this disease. After all, the patient must learn to seek advice about his treatment, otherwise he risks serious harm.
• There are severe forms of epilepsy with enormous resistance to antiepileptic drugs. In such a situational picture, there is a risk of the formation of frequent status epilepticus with the rapid formation of personality traits and even epileptic confusion.
• Some additional factors strongly influence the course of epilepsy, even leading to status epilepticus. Acute infections, and especially those with significant clinical data, can lead to similar complications.
• Intoxication, and especially alcoholism, very easily provoke seizures.
• Many somatic diseases, especially with chronic intoxication, can also aggravate the situation. And especially for patients in such groups, TBIs are very dangerous, which are often accompanied by the seizures themselves, due to the person’s loss of consciousness.
• Brain overstrain, like sleep deprivation, can also provoke such conditions.
Status epilepticus is characterized by violent screams due to muscle contraction; this manifestation occurs during generalized seizures.
Further actions
Relief of status epilepticus is carried out through the following measures:
- ensuring airway patency;
- use of oxygen therapy;
- intravenous injection of Diazepam (maximum daily dose - 40 mg), a side effect of this drug may be respiratory depression.
Further therapy is carried out by administering medications depending on the stage of status epilepticus.
At the initial stage, the following drugs are used to relieve status epilepticus:
- Diazepam;
- Lorazepam;
- Depakine;
- Feniton;
- Oxybutyrate.
Among the side effects of treatment, the following consequences can be identified: arterial hypotension, acute toxic hepatitis, phlebosclerosis, hypokalemia.
At the advanced stage of ES the following is used:
- Diazepam;
- Lorazepam;
- Phenobarbital;
- Sodium thiopental.
At the refractory stage of ES, the following measures are carried out:
- Intubation, correction of electrolyte disturbances, transfer to artificial ventilation of the lungs - to maintain vital functions of the body.
- Barbiturate anesthesia - intravenous injection of sodium thiopental for 20 seconds. 100-250 mg of the drug is administered. If the patient's condition does not improve, a dose of 50 mg is administered every few minutes until the seizure stops. Barbiturate anesthesia can last from 12 hours to a day.
- Dexamethasone and Mannitol injections are given to prevent cerebral edema.
- Infusion dehydration therapy is carried out to eliminate disorders of liquor dynamics and the metabolic process. For this purpose the following are used: Magenzia, Lasix, Cordiamin, Eufillin, Korglykon.
In the event that the epistatus is symptomatic, that is, it arose against the background of brain damage, a neurosurgical operation should be performed to compress the brain vessels.
Treatment
Without emergency assistance, patients die in 50% of cases. To treat status epilepticus, intensive care conditions and specialized ambulances are needed.
First aid
Before doctors arrive, during convulsions it is necessary to protect the patient from possible injuries. Generalized attacks are accompanied by motor activity, disturbance of consciousness, and increased salivation. Before the ambulance arrives, you must:
- lay the person horizontally so that the head is turned to the side and is located above the shoulders (you need to put something under it, for example, a cushion of clothing);
- it is important to improve air access: loosen the collar, remove the tie or scarf, unfasten the tight belt on the belt;
- a soft cloth is placed between the teeth in the slightly open mouth - a handkerchief, a belt, a scarf; using a rigid pad can damage the enamel when the patient involuntarily clenches the jaws;
- traumatic objects are removed from the patient’s arms and legs;
- It is important to hold the epileptic with your hands; involuntary muscle activity is intense.
Drug treatment
The medical team treats status epilepticus with intravenous administration of Diazepam based on the patient’s weight. The permissible daily dose is 40 mg. To relieve paroxysms the following is also used:
- Depakine is a hormonal psychotropic drug;
- Lorazepam is an anti-anxiety tranquilizer;
- Oxybutyrate is a sodium salt nootropic drug;
- Phenytoin is a broad-spectrum antiepileptic drug.
Treatment with these drugs has a depressing effect on patients with status. If respiratory failure is diagnosed after the injection, oxygen therapy is performed. A patient with status epilepticus is given an oxygen mask or intubated (insertion of a breathing tube into the trachea).
If this is not enough, barbiturate anesthesia is performed for up to 12 hours. To reduce brain swelling and improve blood circulation, use:
- Dexamethasone is a hormonal agent that restores microcirculation and metabolic reactions;
- Mannitol is an osmotic diuretic that reduces electrolyte imbalance; Cordiamine, Korglykon, Lasix, Magenzia, and Eufillin can be used for the same purpose.
After the crisis has resolved, the patient’s treatment is continued at home.
Features of the condition in children
Very often, epistatus that occurs in children is a sign of the onset of epilepsy, but it happens that convulsive attacks appear already in the later stages of the course of this disease.
In newborns, a seizure occurs with partial loss of consciousness, while the reaction to external stimuli remains intact.
Generalized SE can manifest itself as tonic-clonic, clonic, myoclonic convulsions.
In nonconvulsive SE, electroencephalography is used to detect peak-wave stupor and slow waves, which reflect a state of epileptic stupefaction. Partial ES can be simple, somatomotor, or dysphasic.
In complex partial epistatus, stable preservation of epileptic twilight of consciousness is observed.
With generalized SE, the main property of an epileptic seizure is disrupted - it does not go away on its own.
The number of attacks can reach several tens or even hundreds per day. In this case, respiratory function and hemodynamics are disrupted, metabolic processes in the brain are disrupted, and the coma state can deepen until death occurs.
Definition and classification of ES
Historically, SE has been defined as “a condition characterized by an epileptic seizure/seizure of sufficient duration or recurrence at sufficiently short intervals to produce a permanent and persistent epileptic state” [2]. This definition was supplemented by the International League Against Epilepsy, which stipulated that the seizure/seizure must last at least 30 minutes, or there must be several seizures during this period of time without recovery of function between them for more than 30 minutes [3].
The first 5 minutes of an attack are called the preliminary/prodromal period, or initial (incipient) SE [4]. Further activity during the attack is divided into early SE (5–30 minutes), established SE (more than 30 minutes) and refractory SE. Emergency intervention corresponds to the temporary definitions of early SE, and urgent intervention corresponds to established SE. In SE, pathophysiological changes develop that cause resistance to anticonvulsants. In children with a primary attack lasting more than 5–10 minutes, the likelihood of the attack stopping without drug intervention is very low [5].
Danger of condition
Mortality in the case of status epilepticus with previously diagnosed epilepsy is 5%, in the case of symptomatic status - 30-50%. If the ES continues for more than an hour, the following serious consequences may occur:
- cerebral edema;
- oxygen starvation of the brain;
- excessive decrease in blood pressure;
- lactic acidosis - excessive accumulation of lactic acid in the body;
- electrolyte imbalance;
- mental retardation and mental retardation in children.
Non-convulsive SE is less dangerous than generalized SE, however, in this case, cognitive impairment may develop.
Epidemiology
In children, the incidence of ES is highest in the neonatal period, then declines over approximately 5 years. The incidence of ES ranges from 10.3 to 61 per 100 thousand people. It is maximum in children of the first year of life and amounts to 135–165 per 100 thousand population [6]. Despite the fact that episodes of ES in children occur more often than in adults, mortality due to ES in children is lower than in adults, amounting to 3% [1, 7]. Most often, SE develops in children with acute or chronic neurological diseases. In individuals aged 5 to 40 years, episodes of SE are relatively rare [8].