Multiple sclerosis (MS) is a severe, incurable disease of the nervous system that affects young people, often females, and is trending upward mainly in European countries. With a progressive course, it quickly leads to disability.
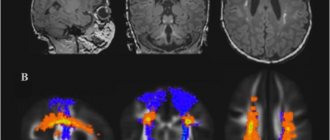
Modern diagnosis of multiple sclerosis is based on complaints and instrumental research data; the disease is difficult to diagnose at the initial stage, when it is possible to start treatment on time. The main information in the early stages of multiple sclerosis is provided by MRI data, which allows one to detect the slightest signs of the disease and identify lesions that have not yet manifested themselves at the clinical level.
MRI of the brain in multiple sclerosis
When making a diagnosis, neurologists at the Yusupov Hospital take into account objective data and the results of MRI, which reveals the dissemination of lesions. The pathological process can be confirmed if two or more lesions are detected on MRI, as well as if the symptoms progress over time (in the presence of subsequent attacks, new lesions or excessive accumulation of the injected contrast agent). In addition, specialists examine the patient’s cerebrospinal fluid, in which oligoclonal bands of immunoglobulins are detected.
The clinic's ophthalmologists determine visual fields, assess the contrast sensitivity of the eye, retinal thickness, and the condition of the fundus. One of the most important diagnostic methods used by our neurologists is a study that tests the somatosensory, auditory and visual evoked potentials of the brain.
Our Moscow center for the treatment of multiple sclerosis uses modern equipment from leading medical equipment manufacturers from the USA and Europe to conduct examinations.
Expert opinion
Author: Boyko Alexey Nikolaevich
Neurologist, Head of the Research Center for Demyelinating Diseases, Doctor of Medical Sciences, Professor
There are many autoimmune diseases, one of them is multiple sclerosis. This is a pathology in which immune cells attack the myelin sheath of a neuron. In simple words, a neuron is like a wire, and the myelin sheath is its insulation, and lymphocytes remove it.
The appearance of multiple sclerosis is associated not only with weakened immunity, but also with vitamin D deficiency - the disease is more common in the north than in the south. Previously, MS was associated with race, but studies have shown that members of the Caucasian race (usually living in northern latitudes) who change their place of residence to a sunnier one get sick less often.
Multiple sclerosis has many symptoms; American neurologists have described more than 500. The diagnosis can only be made by a specialist after a full examination, including MRI and punctures. The disease is rapidly getting younger, women need to be especially attentive to general neurological symptoms and undergo regular examinations, especially if there are risk factors - heredity, vitamin D deficiency, bad habits.
Signs of multiple sclerosis
Some of the first symptoms are loss of vision, paresis, paralysis, weakened sensitivity of the limbs and other parts of the body, and impaired coordination of movements. A person may have the feeling that there is “frozen” on the face, or that the leg or hand is “not his.”
With the development of multiple sclerosis, the following is observed:
- a sharp decrease in performance, mental functions, concentration;
- sudden dizziness for no apparent reason;
- speech problems;
- unilateral decrease in vision up to blindness (impairments appear and disappear);
- problems with coordination of movements;
- impaired motor skills of the hands (the patient finds it difficult to do small work, handwriting noticeably deteriorates, etc.);
- convulsions and non-convulsive epileptic seizures;
- complete or partial paresis of the limbs;
- disturbance of urination, bowel movements, and genital function;
- pain without a clearly defined focus
- anxiety, sudden mood swings, etc.
If several symptoms from the above list appear simultaneously, you should immediately consult a doctor.
The appearance of causeless dizziness may be one of the signs of MS
Treatment
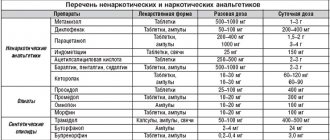
If research results suggest that a patient has multiple sclerosis, doctors at the Yusupov Hospital prescribe symptomatic treatment and betaferon. If a reliable diagnosis was established for the first time (at the onset of multiple sclerosis), it is necessary to influence the primary link of the pathological process. The main goals are to reduce activity and prevent disease progression. To achieve them, the use of one of the drugs is prescribed: betaferon, glatiramer acetate or rebif.
Relapsing-remitting multiple sclerosis in the acute stage requires taking measures aimed at reducing the activity of the pathological process and eliminating the exacerbation (reducing the severity of neurological deficit) or achieving regression of new neurological symptoms. For this purpose, patients at the Yusupov Hospital are prescribed the following medications:
- glucocorticosteroids (methylprednisolone, Solu-Medrol, dexamethasone);
- ACTH (synacthen depot);
- cyclosporine A.
If the patient does not have the opportunity or desire to receive drug therapy, neurologists at the Yusupov Hospital use plasmapheresis to relieve an exacerbation. In addition, patients are prescribed immunoglobulin β-1b or β-1a, intravenous immunoglobulin or glatiramer acetate.
Treatment of remitting-recessive multiple sclerosis in the remission stage is aimed at reducing the activity of degenerative and immunopathological processes, increasing the duration of remission and the severity of the next exacerbation.
For one to two years, patients require intravenous administration of maintenance doses of immunoglobulin (at a dosage of 50 ml per month). Reparative medications, symptomatic therapy, and rehabilitation using modern techniques are prescribed.
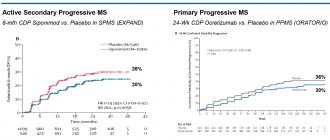
Patients with secondary progressive multiple sclerosis at the Yusupov Hospital are prescribed therapy aimed at eliminating neurovegetative changes, improving immunoregulation and preventing exacerbations. In this case, interferons 1-β or cytostatics (azathioprine, cyclophosphamide, cladribine) and reparative drugs are effective. Symptomatic treatment and rehabilitation are also carried out.
Primary progressive multiple sclerosis is the most difficult to treat. The efforts of doctors in these cases are aimed at slowing down the course of the disease, slowing down neurodegenerative processes, and stabilizing the pathological process. This task can be accomplished through the use of interferons, cytostatic and symptomatic drugs, and intravenous administration of immunoglobulin.
Rehabilitation measures carried out by specialists at the Yusupov Hospital are also effective: massage, physical therapy, physiotherapy and acupuncture.
Make an appointment
Carrying out tomography to diagnose multiple sclerosis
Using MRI for multiple sclerosis, the distribution of demyelination foci in space is revealed and their age is determined. The study is carried out in three planes with a section thickness of 1-3 mm. Scanning is recommended to be carried out on devices with a magnetic field strength of more than 0.5 Tesla, combining studies in the axial (transverse section) and sagittal planes (side view) - for MRI of the brain.
Currently, it is customary to distinguish several MRI manifestations of multiple sclerosis in the form of syndromes:
- Chronic inflammatory demyelination.
- Acute inflammatory demyelination.
- Multifocal degenerative leukoencephalopathy.
- Multifocal diffuse leukoencephalopathy.
The most informative for MRI of the spinal cord in multiple sclerosis are coronal (front view) and sagittal sections on tomographs with a field strength of 1-2 T. The study is carried out in a horizontal position, with the head to the magnet, without preliminary preparation, following the recommendations of radiologists.
Scan Modes
Usually T1 and T2 weighted sequences are used, they are designed to use the differences between tissues in T1 and T2 in order to create maximum contrast between them in normal and pathological conditions, which allows obtaining a large number of types of images in the MRI diagnosis of multiple sclerosis.
| Weighted Sequences | Echo time (TE) | Repetition time (TR) |
| T1 | 15-30ms | 300-500ms |
| T2 | 60-120ms | 1600-2500ms |
It is imperative to use the turbo spin echo technique, the FLAIR sequence (T2 with liquid signal suppression), as well as three-dimensional angiography - 3D TOF. If indicated, three-dimensional thin-section gradient diffusion-weighted sequences (DWI) are additionally performed.
During scanning, pulse sequences are used at various intervals - “inversion recovery” (IR) and “spin echo” (SE). Pathological changes on MRI manifest themselves differently, depending on the type of pulse sequence:
- foci of demyelination in IR mode appear black;
- foci of demyelination in SE mode appear white.
Normal white matter of the brain is visualized:
- light on T1-weighted images;
- on T2 VI – dark.
Foci of demyelination due to an increase in water content have a signal:
- reduced intensity on T1-weighted images;
- elevated on T2-weighted images.
A promising technique is magnetization transfer, based on the exchange of magnetic fields between unbound protons of water and bound protons of myelin, which significantly increases image contrast and makes it possible to better identify nerve fibers devoid of myelin.
MRI of magnetization transfer is especially indicated in situations where there are more than two attacks of the disease, but only one focus in the central nervous system is clinically detected. Visualization of several lesions in the white matter of the brain in this case helps to make an accurate diagnosis.
Doubt can be caused by giant, tumor-like areas accompanied by mass effect (the damaging effect of the formation on surrounding tissues). Magnetic resonance imaging is used to monitor the effectiveness of MS treatment - foci of demyelination change in size at different rates.
Some of them disappear completely, while others appear in a new location. Dynamic scanning reveals exacerbations of the process at the preclinical level. The efficiency of the study increases with the use of contrast techniques.
Applying Contrast
Contrast is used to enhance brain structures with a missing or damaged blood-brain barrier. For this purpose, water-soluble paramagnetic substances based on gadolinium are used; they exhibit an effect from the first to fifteen minutes after intravenous administration.
The ability to accumulate contrast is associated with the activity of the inflammatory process in the nerve fiber; it penetrates into the area of inflammation and edema, causing an increase in the signal on T1-VI in the form of a ring around new or growing areas of sclerosis.
The more pronounced the damage to the nerve fiber, the brighter the image. This process occurs in old lesions, pathological areas located in the cortex and subcortical gray matter, where they are usually not visible on standard T2 images.
The use of Magnevist (a paramagnetic contrast agent based on gadolinium) increases the percentage of detected plaques, which makes it possible to determine the severity of the disease and prescribe adequate therapy. Multiple sclerosis is detected ten times more often on MRI compared to clinical manifestations of the disease.
What do multiple sclerosis lesions look like on photographs?
MS plaques of varying numbers and sizes are detected in the white matter of the spinal cord and in the deep parts of the brain. Characteristic is their location along the edges of the corpus callosum, in the legs, trunk, and cerebellum.
In typical cases, in the structures of the brain, T2-weighted images reveal oval-shaped foci of increased intensity from 2 to 20 mm along the bodies and horns of the ventricles, in the corpus callosum, and less often in the white matter of the cerebral hemispheres, brainstem, and cerebellum. Fresh lesions are clearly visualized with contrast.
Typical MRI signs of sclerotic plaques in the spinal cord are located at the level of the first and second segments, with a diameter of at least 3 mm, most often in the area of the posterior and lateral columns, without swelling of the spinal cord.
Contraindications for tomography
Magnetic resonance imaging is a safe diagnostic method, but there are limitations to its performance. MRI is absolutely contraindicated for owners of an artificial pacemaker, endoprostheses with ferroalloys, metal clips on cerebral vessels, metal fragments and bullets, and drug dispensers.
The study can be done on pregnant women in the first six months of pregnancy, people suffering from severe cardiovascular diseases, or claustrophobia if the benefit from the information received outweighs the risk.
MRI diagnostics of multiple sclerosis is the only method that visualizes lesions before clinical manifestations of the disease. The study allows you to determine the exact size, location, and age of the pathological area. In doubtful cases, it allows you to confirm the diagnosis, track the dynamics of the disease and the effectiveness of the treatment.
Laboratory diagnostics
A blood test is a fairly informative study that allows you to exclude or confirm the diagnosis. To do this, neurologists analyze the following indicators:
- level of anti-inflammatory cytokinins in peripheral blood;
- lymphocyte transformation reaction upon contact with myelin basic protein;
- indicator of antibodies to myelin.
With a confirmed diagnosis in patients with multiple sclerosis, a blood test demonstrates the dynamics of the process.
Diagnostic and treatment methods at the Yusupov Hospital are selected individually for each patient. When selecting drugs and their dosages, the clinical symptoms of the disease and its course are taken into account. The therapy can significantly improve the quality of life of patients.
What does multiple sclerosis look like on an MRI?
Diagnosis of multiple sclerosis allows us to identify the full picture of pathological changes. The following localization of lesions is considered typical:
- superficial parts of the pons;
- paraventricular substance adjacent to the bodies of the lateral and third and the bottom of the fourth ventricles;
- middle cerebellar peduncles;
- white matter under the cerebral cortex;
- optic nerve;
- region of the cervical spinal cord;
- inferior border of the corpus callosum.
Multiple sclerosis on an MRI of the brain looks like round spots with a diameter of up to 2 centimeters, which can merge as the pathology develops. The shade of the changed areas depends on the stage of the disease and can be light, dark or identical to healthy tissues (without contrast it does not stand out).
“Dawson’s fingers” on MR tomograms in axial (left) and sagittal (right) projections - look like light oblong lesions on T1 VI
The classic sign of multiple sclerosis on MR images of the brain is linear plaques located perpendicular to the lateral ventricles. They are called “Dawson's fingers”.
In the spinal cord, foci of demyelination appear as elongated formations spreading from the center to the periphery, involving the dorsal horns in the pathological process.
The final stage of progression of lesions in multiple sclerosis are “black holes”, indicating the destruction of axons.
On an MRI scan of the brain in T1 VI, you can see long-term lesions of MS (indicated by arrows)
Carrying out MRI for MS
The subject needs to remove any objects that may affect the magnetic image, for example:
- glasses;
- hairpins;
- watch;
- jewelry;
- dentures;
- Hearing Aids;
- wigs;
- underwire bras.
Before the scan, your healthcare provider may inject a contrast agent called gadolinium
intravenously. Gadolinium improves image quality and increases the diagnostic accuracy of MRI. During scanning, the inside of the magnet makes loud, repetitive noises such as tapping. The technician may provide earplugs or music to help block out the noise.
Location and symptoms
The location of the lesions determines MS status.
Symptoms also depend on the type and location of the lesions. However, some patches may appear in areas of the brain that do not cause symptoms.
Some locations of the lesions and the MS symptoms they can cause include:
Cerebellum (back of the brain)
- impaired balance and coordination;
Optic nerve (nerve behind the eye)
- problems related to vision;
Spinal cord
- muscle stiffness;
- numbness and tingling;
- pain in the arms, legs, or both;
- problems with urination or bowel movements.