Interferons are a group of proteins produced by the body's cells in response to viral and bacterial attacks, as well as invading small molecule chemicals. The anti-inflammatory effect of interferons was established in the middle of the twentieth century.
It was observed that a cell infected with the influenza virus begins to produce interferon, which prevents the further spread of the infection. And since 1957, interferon began to be considered the most important internal factor of protection against infectious agents.
Somewhat later, data were obtained on the property of Interferon to stimulate the immune system. Therefore, today it is used as a medicine, which is available in different forms.
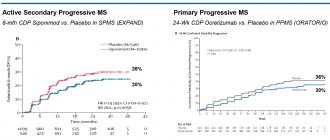
Interferons beta do not slow progression of MS
Scientists from the University of British Columbia (Canada) conducted a retrospective study, the results of which cast doubt on the effectiveness of interferon-beta therapy for multiple sclerosis (Betaferon, Avonex, Rebif).
Previously, the published results of several small post-marketing studies conducted by European scientists confirmed the long-term effectiveness of the “gold standard” PMTRS.
The results of the study, published in the Journal of the American Medical Association (JAMA), not only became the subject of discussion in the scientific world, but also received resonant responses on the websites of the Multiple Sclerosis Societies of America, Canada, Great Britain, in such media as the New York Times and Time.
Interferon beta studies
Helen Tremlett, professor and chair of the Department of Neuroepidemiology and Multiple Sclerosis at the University of British Columbia, presenting information about the study on the long-term effectiveness of interferons, noted:
We know that this class of drugs can be very helpful in reducing relapse rates. We do not recommend that patients stop taking these medications, but these findings suggest that expectations regarding the potential benefits of drug treatment should be more realistic and disability-sensitive.
Let us recall that interferons beta are course-modifying drugs for multiple sclerosis (MSDs), approved as first-line drugs for preventive treatment of MS in most countries of the world. The results of clinical studies of these drugs show that their use can reduce the frequency and severity of relapses (exacerbations) of the disease by a third and delay severe disability.
Canadian scientists analyzed data on patients diagnosed with relapsing-remitting multiple sclerosis enrolled in clinics in British Columbia between 1985 and 2004. Experts studied the connection between treatment with beta interferons (Betaferon, Avonex, Rebif) and a decrease in the rate of disease progression and disability.
In total, the medical records of 2,656 patients were analyzed during the study. Of these, 868 were included in a group of patients who were treated with beta interferons (Avonex or Betaferon or Rebif) between July 1995 and December 2004. 829 patients were included in the first comparison group: these patients, from July 1995 to December 2004, were eligible for treatment with interferon beta according to indications, but did not receive it for various reasons. 959 patients were included in the second comparison group (historical comparison group): these patients would have been eligible for treatment according to the indications, but the data on these patients covered the period from April 1985 to June 1995, a period when beta interferon therapy for MS was not yet used in wide clinical practice. Accordingly, these patients also did not receive DMT therapy.
Contraindications
Contraindications include: allergic response of the body; hypersensitivity to the active substance; pregnancy; breastfeeding period; childhood and adolescence; severe depression; renal failure.
“While taking these medications, I had severe allergies to ragweed, coffee, honey, and watermelons. Over time, after finishing taking it and limiting myself in food (excluded meat, sweets, baked goods), allergy symptoms began to decrease.”
Treatment with interferon is carried out with caution in the following concomitant diagnoses:
cardiac ischemia; convulsions; liver pathologies.
In this case, the patient needs strict medical supervision. Dosage and course duration The use of drugs from the interferon group in the treatment of multiple sclerosis is carried out under the supervision of the attending physician, which is explained by the frequent development of side symptoms.
The product is intended for subcutaneous and intramuscular administration. The recommended dosage is 8 million IU. At the beginning of treatment, as a rule, the patient is prescribed a reduced dose, which is gradually increased to the required dose. This approach reduces the likelihood of unwanted reactions.
The total duration of interferon treatment for multiple sclerosis is unknown. On average, admission lasts three to five years, but everything is individual.
Injections of the drug can also be given at home, but in this case the person is required to complete a training course on the proper preparation and administration of the medication.
Observations
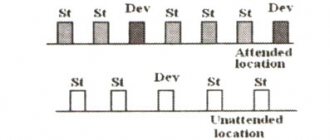
The mean follow-up period was 5.1 years for the group of patients receiving DMT and 4.0 years for the control groups.
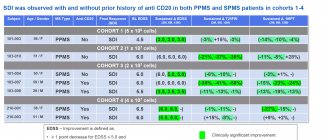
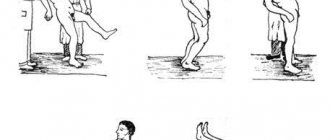
The main purpose of the study was to analyze the time period during which patients from different groups achieved an Expanded Disability Scale (EDSS) score of 6 points. A condition in which, for more than 150 days, a person requires intermittent or constant unilateral assistance (cane, crutches, walker) to walk about 100 meters with or without rest
EDSS scores of 6.0 reached 10.8% of patients in the group of patients treated with interferon beta. 5.3% of patients from the first comparison group (who did not receive DMT treatment during the period when DMT treatment began to be used in clinical practice). And 23.1% of patients from the second comparison group (historical comparison group, patient data covered 1985-1995).
After making statistical adjustments that affected the analyzed results (gender, age, disease duration, baseline (at the start of the study) EDSS score, etc.), the researchers concluded that treatment with beta interferons was not associated with a statistically significant difference in the score the likelihood of achieving an EDSS of 6.0 compared with groups of patients who were not treated with any DMT drugs.
In conclusion, Canadian experts note:
We found no evidence that interferon beta therapy is associated with slower progression of disability in patients with relapsing-remitting multiple sclerosis. The ultimate goal of MS treatment is to prevent or delay long-term disability. The findings call into question the routine use of interferon beta drugs to achieve this goal.
Sources: full text of the study results Association Between Use of Interferon Beta and Progression of Disability in Patients With Relapsing-Remitting Multiple Sclerosis
Key words: multiple sclerosis, children, Betaferon.
Multiple sclerosis is a chronic progressive disease of the central nervous system that usually affects young and middle-aged people. Clinically, the disease manifests itself as diffuse neurological symptoms with the involvement of several functional systems in the pathological process, which leads to loss of performance, ability to move and self-care. According to the World Health Organization, among neurological diseases, multiple sclerosis (MS) is the most common neurological cause of permanent disability in young people. In recent years, there has been an increase in the number of patients with multiple sclerosis throughout the world, which is associated, firstly, with improved diagnostic capabilities and, above all, with the widespread introduction of magnetic resonance imaging into medical practice, and secondly, with an increase in life expectancy against the background specific treatment, thirdly, with a true increase in incidence. In Russia, on average, multiple sclerosis occurs with a frequency of 30 to 100 cases per 100,000 population. It is noteworthy that just 20 years ago, in medical circles, multiple sclerosis was viewed as an exclusively adult disease. However, in recent years it has become obvious that multiple sclerosis also occurs in childhood. Epidemiological studies conducted in Russia and abroad have shown that in 5-10% of patients, multiple sclerosis manifests itself before the age of 18 years [1, 2]. Questions of the etiology and etiotropic treatment of this disease remain open to this day. In recent years, the multifactorial etiology of multiple sclerosis has become increasingly recognized, based on which the main role in the development of the disease is given to the influence of external factors on genetically predisposed individuals. It is assumed that a combination of external and genetic factors can lead to the development of inflammatory and immunopathological reactions, which are accompanied by immunological and biochemical changes in both the central nervous system and the body as a whole. Studies conducted at the Research Institute of Pediatrics of the Scientific Center for Children's Diseases of the Russian Academy of Medical Sciences (Dir. Academician of the Russian Academy of Medical Sciences A.A. Baranov) showed that multiple sclerosis in childhood has its own clinical features in the form of a predominance of symptoms of damage to the pyramidal tract and brain stem, with relatively rare sensory and pelvic violations. In case of optic neuritis, an unfavorable prognosis is caused by the early development of secondary atrophy of the optic nerves. One of the main differences between multiple sclerosis with its onset in childhood, despite the high frequency of detected “giant” lesions, is the slower formation of irreversible degenerative changes, both according to MRI (local and diffuse atrophy of the brain substance) and clinical (dissociation between the volume focal brain damage and the severity of neurological disorders). The presence of moderate clinical manifestations with a large number of lesions on MRI indicates great opportunities for compensation of impaired functions in childhood. The distribution curve of patients by age of onset of multiple sclerosis depending on gender showed a predominance of boys in the age group from 3 to 5 years, and a clear predominance of girls in the age group from 10 to 13 years [3, 22]. In more than 97% of pediatric patients, multiple sclerosis debuts in the form of a relapsing-remitting type of disease [3]. The long-term prognosis of disease progression in this category of patients remains a subject of debate, however, retrospective studies have shown that despite the longer average period of time from the onset of multiple sclerosis to the achievement of persistent neurological disability, in general, compared with adult patients at the time of the formation of irreversible neurological deficit, patients with pediatric onset of the disease are younger than patients who became ill after 18 years of age [3]. Since multiple sclerosis is a heterogeneous disease in terms of its development mechanism and types of clinical course, therapy is differentiated. Within the framework of the existing concept of the pathogenesis of multiple sclerosis, today the most effective pathogenetic treatment is immunomodulatory therapy, the appearance of which in the clinical practice of a neurologist has changed therapeutic approaches to a pathology previously considered incurable, and has made it possible to actually reduce the frequency of exacerbations in relapsing-remitting and secondary progressive courses. multiple sclerosis. Medicines, so-called “course-modifying drugs for multiple sclerosis,” reduce the frequency of exacerbations of multiple sclerosis by an average of 30% and, to varying degrees, slow the rate of progression of irreversible disorders leading to disability. They have long been widely used in adult patients with multiple sclerosis, especially at the stage of relapsing-remitting disease. The safety and tolerability of immunomodulatory drugs have been well studied, but all major studies conducted in this area have included patients over 18 years of age. One of the leading modern principles of immunomodulatory treatment of MS is the earliest possible initiation of therapy for patients with a relapsing-remitting type of the disease [14]. The advisability of using drugs for immunomodulatory treatment of multiple sclerosis has been proven even before a reliable diagnosis is made in patients after the first demyelinating episode or the so-called clinically isolated syndrome, with a high risk of progression according to MRI [15]. Immunomodulatory drugs include beta interferons. Their use makes it possible to reduce the frequency and severity of exacerbations of multiple sclerosis by a third; during treatment, a decrease in the number of inflammatory foci in the central nervous system was noted by 50-80%; in addition, the use of beta interferons has a positive effect on cognitive functions and the quality of life of patients in general. Currently, interferons are considered as the drugs of choice in the treatment of relapsing-remitting multiple sclerosis, and their successful use in clinically isolated syndrome has also begun. Interferons beta are also used in secondary progressive multiple sclerosis, since in this case they slow down disability and reduce the formation of new lesions on MRI. The main side effects of interferons: flu-like symptoms (fever, chills, malaise, muscle pain and fatigue) develop in approximately half of all patients at the beginning of treatment, but subsequently disappear. Local reactions, moderate thrombocytopenia and anemia, depressive episodes, and increased transaminase concentrations are less common. In some cases, the use of interferons may be accompanied by the formation of neutralizing antibodies. Treatment with interferons is carried out for a long time, its termination is justified only in case of obvious ineffectiveness (exacerbations more than 4 times a year or progression of disability by 1 point on the EDSS scale in 6 months) and if side effects develop. Interferons beta have antiviral and immunomodulatory activity. It is known that the biological effect of these drugs is mediated by their interaction with specific receptors that are found on the surface of human cells. The binding of interferon beta to these receptors induces the expression of a number of substances that are considered to mediate the biological effects of interferon beta. Beta interferons reduce the binding capacity and expression of interferon gamma receptors and enhance their degradation. In addition, they have the ability to increase the suppressor activity of peripheral blood mononuclear cells and, by blocking matrix metalloproteinase, stabilize the state of the blood-brain barrier. Interferon beta 1b (Betaferon®), the first of the beta interferons synthesized for the immunomodulatory treatment of multiple sclerosis, is now considered an established drug throughout the world. Among all DMTs, Betaferon has the longest clinical experience of use. To date, ideas about the effectiveness and safety of Betaferon are based on the results of controlled clinical studies involving patients with relapsing-remitting and secondary progressive multiple sclerosis, as well as in patients with clinically isolated syndrome. The experience of using interferon beta 1b in adult neurological practice spans more than 16 years of clinical observation. In 2005, the results of a 16-year prospective multicenter study of 135 adult patients with MS were presented for the first time, in whom the effectiveness and safety of long-term use of this drug was established against the background of continuous immunomodulatory therapy with interferon beta 1b [16]. Clinical studies have shown that the use of Betaferon in adult patients with relapsing-remitting and secondary progressive multiple sclerosis reduces the frequency of clinical exacerbations (after 2 years by 34 and 30%, respectively, compared with the group of patients taking placebo), the severity of relapses, the number of hospitalizations, the need for in treatment with corticosteroids, and also prolongs the duration of remissions. According to magnetic resonance imaging of the brain, in patients with relapsing-remitting and secondary progressive disease during treatment with Betaferon, there is a significant decrease in the formation of new active lesions, and the severity of the pathological process is also reduced. It has been proven that the use of interferon beta 1b in clinically isolated syndrome helps to increase the time until a diagnosis of definite multiple sclerosis is made. In patients with secondary progressive multiple sclerosis, the use of Betaferon can delay the progression of the disease for up to 12 months, even with a significant degree of disability. Currently, there are a number of studies conducted both abroad and in our country devoted to the study of the use of interferon beta 1b (Betaferon) in children and adolescents [5, 17]. The first experience with the use of drugs for immunomodulatory therapy of MS up to 18 years of age published in the literature was a clinical observation conducted by AB Adams et al in 1999, which demonstrated “dramatic” clinical effectiveness (significant reduction in disability and absence of exacerbations throughout treatment), confirmed by dynamic MRI data show a positive experience of long-term (30 months) treatment with interferon beta 1b for a 7-year-old child with relapsing-remitting MS. Considering the lack of experience with the use of interferon beta in children, the dose of the drug was adapted to age: initial - 4 million IU, after a year it was increased to 6 million IU. No systemic or local adverse reactions were observed during treatment. During therapy, a short-term increase in the titer of neutralizing antibodies to interferon beta 1b was recorded in the child, which did not affect the effectiveness of therapy, either clinically or according to MRI data [5]. The next description of the use of interferon beta 1b in children with multiple sclerosis is a study conducted in 2001 by SN Tenembaum et al., who also describe the positive experience of using interferon beta and glatiramer acetate in 19 children with relapsing-remitting and secondary progressive MS with exacerbations (5 children received interferon beta 1b). This publication draws attention to the rationale for the use of “adult” standard doses of interferon beta in children and adolescents, since an attempt to reduce the dose of the drug in the study (“adaptation” to age) reduced the clinical effectiveness of therapy. In domestic literature in 2004 by authors N.A. Totolyan and A.A. Skoromets used the example of 5 clinical cases to illustrate his own experience in prescribing interferon beta 1b for up to 18 years of age. The obtained clinical observation data were analyzed by the researchers and a number of reasoned conclusions were proposed:
1) on the advisability of prescribing drugs for immunomodulatory therapy as early as possible for children and adolescents with MS, especially with high disease activity, characterized by a high frequency of exacerbations (2 or more exacerbations during the first year from the onset of MS); 2) given the limited data on the safety of the use of beta interferons in childhood and adolescence, it is recommended to begin this type of therapy in a hospital setting, monitoring changes in biochemical and hematological parameters (for example, the number of blood leukocytes, the activity of liver enzymes, the level of creatinine in the blood serum); 3) expected systemic and local side effects when prescribing beta interferons require prevention (for example, moving the injection of the drug to the evening) and, if necessary, correction (for example, prescribing non-steroidal anti-inflammatory drugs);
4) in most cases, children are shown standard doses of beta interferons, however, to reduce the severity and duration of influenza-like syndrome, it is advisable to titrate the dose of the drug at the beginning of treatment; 5) therapy with interferon beta drugs should be continuous and long-term, since unreasonable cessation of treatment entails significant decompensation of the immunopathological process [17].
In 2006, the results of the first international multicenter retrospective study of the safety and tolerability of interferon beta 1b in children and adolescents with MS were published, based on the results of observation of patients who received at least one injection of interferon beta 1b before 18 years of age, collected up to 2004 inclusive. The study made it possible to systematize scattered data on the experience of using interferon beta 1b in pediatrics. The study included 43 pediatric patients with relapsing-remitting MS from 8 medical centers in the USA, Canada, Argentina, Turkey, Russia and Germany. After the final processing of the data obtained, only 39 patients met the diagnostic criteria for reliable MS [18, 19], in whom the final analysis of the effectiveness of treatment was carried out, and the results of observation of 4 children not included in this group were used to assess the tolerability of therapy. The average duration of immunomodulatory treatment was 29.2 months, and the average age of patients at the time of initiation of therapy was 13 ± 3.0 years. The clinical effectiveness of immunomodulatory therapy was confirmed by a decrease in the average EDSS score from 2.5 (from 0 to 8.5) to 2.0 (from 0 to 6.5) and a 50% reduction in the average annual frequency of exacerbations (the dynamics of the indicator was assessed in 32 children who received treatment for 12 months or more). To objectify the statistical processing of data on the safety and tolerability of therapy in a heterogeneous group of patients by age, all patients were conditionally divided into a subgroup of children under 10 years of age inclusive (8 patients) and a subgroup of adolescents from 11 to 17 years 10 months (35 patients). It should be noted that in the subgroup of children under 10 years of age, more laboratory abnormalities associated with the activity of liver enzymes were recorded, which apparently influenced the increase in the number of adverse reactions in the younger group as a whole (87.5% compared to 62. 9% in older patients). Based on the spectrum, frequency and severity of clinical adverse reactions (influenza-like syndrome in 35% of patients, local reactions in 21% of patients) and changes in laboratory parameters (increased activity of liver transaminases in 26% of patients), and none of the identified side effects was considered as severe or unexpected, the authors concluded that the treatment was well tolerated [20]. At the Scientific Center for Children's Health of the Russian Academy of Medical Sciences (directed by Academician of the Russian Academy of Medical Sciences A.A. Baranov), a clinical observation was carried out of 22 adolescents with relapsing-remitting (18 patients) and secondary progressive (4 patients) multiple sclerosis aged 13 to 17 years, during treatment interferon beta 1b (duration from 2 to 15 months) at a dose of 8 million IU subcutaneously every other day [21]. The effectiveness of therapy in patients was confirmed by a decrease in the average disability score (from 2.56 ± 0.23 to 2.09 ± 0.22 points on the EDSS scale); the number of patients without exacerbations during treatment (13 children - 59%); a decrease in the average annual frequency of exacerbations in 7 patients who received the drug for 12 months or more (from 2 ± 0.37 to 1.14 ± 0.34 exacerbations per year), and the progression rate from 0.69 ± 0.15 before treatment up to 0.45 ± 0.07 after a course of immunomodulatory therapy. During therapy, 12 patients (54%) experienced adverse reactions, represented by influenza-like syndrome in 50% (11 patients), local reactions were observed in 9% (2 patients), and in one teenager (4.5%) changes in biochemical blood parameters - a significant increase in the activity of liver transaminases (more than 10 times), and in one clinical case (4.5%) a depressive episode was observed. In the last two cases, a decision was made to discontinue the drug. The totality of all the data presented above demonstrates the need and advisability of timely administration of drugs for immunomodulatory therapy for both adolescents and children with multiple sclerosis. The results of a study of the natural course of multiple sclerosis in children (67 patients with the onset of the disease before 16 years of age, observed without the use of drugs for immunomodulatory treatment for 4.91 ± 0.58 years), also conducted in 2002 at the Research Institute of Pediatrics of the Scientific Center for Disease Control of the Russian Academy of Medical Sciences, indicate that without therapy, during the first five years from the moment of manifestation of the disease, that is, by the end of the “pediatric” age, almost 100% of patients with early onset of multiple sclerosis develop a persistent neurological deficit with EDSS = 3 points, and about 40% of patients will move into the stage of secondary progression of multiple sclerosis [22]. At the same time, the assumption made by both domestic and foreign authors about high functional plasticity, more intense remyelination and less severe neuronal damage in children was confirmed by data from dynamic MRI observations of children and adolescents with relapsing-remitting multiple sclerosis. Thus, based on theoretical data and practical positive experience in the use of DMTRS in pediatric neurological practice, it can be argued that early initiation of immunomodulatory therapy for multiple sclerosis in patients of childhood and adolescence is not only possible, but also necessary, since children and adolescents who have not received timely and adequate treatment, by the time they reach adulthood they will become permanently neurologically disabled.
Recommended reading 1. Duquette P., Murray TJ, Pleines J. et al. Multiple sclerosis in childhood: clinical profile in 125 patients // J Pediatr. 1987; 111: 359-363. 2. Ghezzi A., Deplano V., Faroni J. et al. Multiple sclerosis in childhood: clinical features of 149 cases // Mult Scler. 1997; 3: 43-46. 3. Boiko A., Vorobeychik G., Paty D., Devonshire V., Sadovnick D. Early onset multiple sclerosis: a longitudinal study // Neurology. 2002; 59: 1006-1010. 4. Banwell BL Pediatric multiple sclerosis // Curr Neurol Neurosci Rep. 2004; 4: 245-252. 5. Adams AB, Tyor WR, Holden KR Interferon beta-1b and childhood multiple sclerosis // Pediatr Neurol. 1999; 21: 481-483. 6. Mikaeloff Y., Moreau T., Debouverie M. et al. Interferon-beta treatment in patients with childhood-onset multiple sclerosis // J Pediatr. 2001; 139: 443-446. 7. Waubant E., Hietpas J., Stewart T. et al. Interferon beta-1a in children with multiple sclerosis is well tolerated // Neuropediatrics. 2001; 32: 211-213. 8. Eraksoy M., Demir G., Ozcan H., Bavndir C., Say A., Saruhan G. Multiple Sclerosis in childhood: a prospective study // J Neurol. 1996; 243: 444. 9. Eraksoy M. In: Siva A, Kesselring J, Thompson AJ, eds. Multiple sclerosis in children: a review. London: Martin Dunitz, 1999. 10. Tenembaum S., Segura M., Fejerman N. Tolerability and efficacy of disease-modifying therapies in childhood and juvenile multiple sclerosis // Neurology. 2001; 56:A361. 11. Tenembaum S., Segura M., Fejerman N. Disease-modifying therapies in childhood and juvenile multiple sclerosis // Mult Scler. 2001; 7:S57. 12. Tenembaum S., Segura M. Clinical effects of disease-modifying therapies in early-onset multiple sclerosis // Neurology. 2004; 62:A488. 13. Pohl D., Rostasy K., Gartner J., Hanefeld F. Treatment of early onset multiple sclerosis with subcutaneous interferon beta-1a // Neurology. 2005; 64:888-890. 14. Rieckmann P., Toyka K.V., Bassetti C. et al. Escalating immunotherapy of multiple sclerosis-new aspects and practical application // J Neurol. 2004; 251: 1329-1339. 15. Kappos L., Polman CH, Freedman MS, Edan G., Hartung HP, Miller DH, Montalban X., Barkhof F., Bauer L., Jakobs P., Pohl C., Sandbrink R. Treatment with interferon beta- 1b delays conversion to clinically definite and McDonald MS in patients with clinically isolated syndromes // Neurology. 2006; 67: 1-8. 16. Ebers G., Rice G., Wolf Ch., Traboulsee A., Langdon D., Kaskel P., Salazar-Grueso E. 16-year long-term follow-up of interferon beta-1b treatment of patients with multiple sclerosis. Presented at Congress: 2005: 21st ECTRIMS, Thesaloniki, Greece. 17. Totolian NA, Skoromets AA Interferon-beta treatment in patients with childhood-onset and juvenile multiple sclerosis // Zh Nevrol Psikhiatr Im SS Korsakova. 2004;104(9):23-31. 18. McDonald WI, Compston A, Edan G et al. Recommended diagnostic criteria for multiple sclerosis: guidelines from the International Panel on the diagnosis of multiple sclerosis // Ann Neurol. 2001; 50: 121-127. 19. Poser CM, Paty DW, Scheinberg L. et al. New diagnostic criteria for multiple sclerosis: guidelines for research protocols // Ann Neurol. 1983; 13: 227-231. 20. Banwell B., Reder AT, Krupp L. et al. Safety and tolerability of interferon beta-1b in pediatric multiple sclerosis // Neurology. 2006; 66; 472-476. 21. Bykova O.V., Kuzenkova L.M., Maslova O.I. The use of interferon beta 1b in adolescents with multiple sclerosis // Journal of Neurology and Psychiatry named after. S.S. Korsakova 2006;9: 29-33. 22. Gusev E., Boiko A., Bikova O. et al. The natural history of early onset multiple sclerosis: comparison of data from Moscow and Vacouver // Clin Neurol Neurosurg. 2002, 104: 203-207. 23. Higurashi N., Hamano S., Eto Y. Secondary progressive multiple sclerosis in childhood – interferon beta 1b treatment //To Hattatsu. 2006; 38:3:209-13.
Medicine form beta-1a
Alpha interferon is used to treat cancer, but this form of the drug has no effect on multiple sclerosis. The alpha form is not able to slow down the course of the disease, like the gamma type of interferon. The only type of molecule that can be used for pathology is interferon beta-1a. The substance slows down degenerative processes and helps relieve the patient of severe symptoms for 5-15 years.
The group of effective drugs with the beta-1a form includes: Rebif, Avonex, Betaferon. But about 30% of patients are insensitive to the use of the drug. In other cases, it reduces the number of relapses by about a third.
Beta interferon cannot be prescribed for multiple sclerosis if the patient is depressed, pregnant, or under 16 years of age.
The drug is characterized by frequent side effects: skin rashes, necrosis, problems with heart rhythm. Sometimes disorders of the liver occur, fatigue increases, headache, nausea, neutropenia, fever, sweating and chills appear, and in women the menstrual cycle is disrupted.
Release form, packaging and composition of the drug Interferon Beta-1B
Solution for subcutaneous administration
transparent, colorless or yellowish.
| 0.5 ml | |
| human recombinant interferon beta-1b | 8 million IU |
Excipients
: sodium acetate trihydrate - 0.408 mg, glacial acetic acid - up to pH 4.0, dextran 50-70 thousand - 15 mg, polysorbate 80 - 0.04 mg, mannitol - 50 mg, disodium edetate dihydrate - 0.0555 mg, water for injection - up to 1 ml.
0.5 ml - syringes (1) - contour cell packaging (1) (complete with alcohol wipes No. 1) - cardboard packs. 0.5 ml - syringes (1) - contour cell packaging (5) (complete with alcohol wipes No. 5) - cardboard packs. 0.5 ml - syringes (1) - contour cell packaging (15) (complete with alcohol wipes No. 15) - cardboard packs.
Solution for subcutaneous administration
transparent, colorless or yellowish.
| 1 ml | |
| human recombinant interferon beta-1b | 8 million IU |
Excipients
: sodium acetate trihydrate - 0.408 mg, glacial acetic acid - up to pH 4.0, dextran 50-70 thousand - 15 mg, polysorbate 80 - 0.04 mg, mannitol - 50 mg, disodium edetate dihydrate - 0.0555 mg, water for injection - up to 1 ml.
1 ml - bottles (5) - plastic contour packages (1) complete with disposable syringes (5), medical needles (5), alcohol wipes (10) - cardboard packs. 1 ml - bottles (5) - plastic contour packages (2) complete with disposable syringes (10), medical needles (10), alcohol wipes (20) - cardboard packs. 1 ml - bottles (5) - plastic contour packages (3) complete with disposable syringes (15), medical needles (15), alcohol wipes (30) - cardboard packs. 1 ml - bottles (5) - plastic contour packages (6) complete with disposable syringes (30), medical needles (30), alcohol wipes (60) - cardboard packs. 1 ml - bottles (5) - plastic contour packages (1) complete with disposable syringes (5), two types of medical injection needles (5), alcohol wipes (10) - cardboard packs. 1 ml - bottles (5) - plastic contour packages (2) complete with disposable syringes (10), two types of medical injection needles (10), alcohol wipes (20) - cardboard packs. 1 ml - bottles (5) - plastic contour packages (3) complete with disposable syringes (15), two types of medical injection needles (15), alcohol wipes (30) - cardboard packs. 1 ml - bottles (5) - plastic contour packages (6) complete with disposable syringes (30), two types of medical injection needles (30), alcohol wipes (60) - cardboard packs.
Interferon 1b
The drug "Infibeta" is interferon 1b, recommended for multiple sclerosis to eliminate symptoms and progress of the disease. It is highly effective and is available in powder form with water for injection. Has several features:
- combination of antiviral and immunomodulatory functions;
- interacts with immune cell receptors and suppresses their response , however, the exact mechanism of operation of the substance is unclear;
- helps reduce the amount of glucocorticoids taken;
- reduces the number of relapses and hospitalizations of the patient;
- improves the quality of life of patients with various forms of multiple sclerosis.
The prescription and use of beta-1b drugs is recommended for certain forms of sclerosis.
Method of use
The high effectiveness of interferon 1b in multiple sclerosis has been proven in the following cases:
- Clinically isolated syndrome. In this condition, there is one period of change in nerve fibers in the absence of associated causes. Patients do not take glucocorticosteroids, since interferons give the desired result - they completely stop the progression of the disease for a long time.
- Multiple relapsing sclerosis. Beta interferons are used to prevent exacerbations, reduce hospital visits, and reduce the severity of symptoms.
- Sclerosis with secondary progress. The disease occurs with repeated remissions and exacerbations. In this form, interferon significantly prolongs the patient’s life and slows the progression of the disease.
However, the use of interferons 1b in multiple sclerosis is not always indicated.
Special indications
Beta interferons can be used together with other drugs, since not a single medication affects the absorption and process of assimilation of the substance. Interferons can be used to treat any group of patients. But it should be borne in mind that beta molecules impair liver function, reducing its ability to remove harmful substances and drug toxins. If antidepressants and anticonvulsants are prescribed, this property may become critical.
Beta medicine belongs to the group of the most effective drugs for multiple sclerosis, but cannot give a 100% guarantee for the restoration of the body. The unknown mechanism of action sometimes leads to a lack of effect in some patients.
Side effects
After prescribing interferon beta 1 b for multiple sclerosis, the effects in the first month can greatly disturb the patient:
- severe muscle pain and joint aches develop;
- fever and chills, sweating appear;
- to prevent severe symptoms, the patient is prescribed Advil, Tylenol, or Motrin before interferon is administered;
- local itching, swelling and redness occurs;
- the patient is worried about irritability, anxiety;
- sometimes disturbances of consciousness and depression develop;
- concentration and memory decrease.
The patient's condition must be monitored by a doctor. In some cases, drug withdrawal is necessary. But more than 2/3 of patients get used to interferon after 1-2 months.
Side effects
During treatment with the drug, the following reactions were most often observed:
- rapid fatigue;
- headache;
- muscle pain;
- nausea, vomiting.
Long-term therapy may cause:
Don's tablets
- anemia;
- decreased levels of leukocytes and platelets;
- decreased blood clotting ability;
- transient increase in the activity of liver transaminases;
- increased heart rate;
- decreased appetite;
- arthralgia and bone pain;
- drowsiness;
- indigestion;
- drop in blood pressure;
- shortness of breath;
- hair loss.
All of these adverse reactions are reversible and disappear after stopping the drug. The reason to cancel or reduce the dose of Interferon beta may be an increase in body temperature above 40°, accompanied by fever, vomiting and surges in blood pressure.
Drug interactions
In combination with glucocorticosteroids (GCS) and non-steroidal anti-inflammatory drugs (NSAIDs), the effectiveness of Interferon beta may be reduced. Concomitant use with Paracetamol is allowed. The drug may increase the half-life of Theophylline from the body.
Research of drugs in the treatment of sclerosis
In 2004, research by Canadian scientists questioned the unconditional effectiveness of interferon drugs in the treatment of relapsing-remitting multiple sclerosis with relapses. Interferon beta was previously thought to be the gold standard in slowing the progression of the disease.
The study analyzed more than 2,600 cases of patients with multiple sclerosis:
- 868 people were included in the group that received beta interferon treatment from 1995 to 2004;
- 829 patients were included in the same year group who, for various reasons, did not receive the medicine, although it was prescribed to them.
Indications for use
- clinically isolated syndrome (CIS) (a single clinical episode of demyelination suggestive of multiple sclerosis, subject to the exclusion of alternative diagnoses) with sufficient severity of the inflammatory process to prescribe intravenous corticosteroids to slow the transition to CDRS in patients at high risk of developing CDRS.
There is no generally accepted definition of high risk. According to the study, patients with monofocal CIS (clinical manifestations of 1 lesion in the central nervous system) and ≥T2 lesions on MRI and/or lesions accumulating contrast agent are considered to be at high risk for developing CDRS. Patients with multifocal CIS (clinical manifestations of >1 lesion in the central nervous system) are at high risk of developing CDRS, regardless of the number of lesions on MRI;
- relapsing-remitting multiple sclerosis - to reduce the frequency and severity of exacerbations of multiple sclerosis in patients who are able to walk without assistance, with a history of at least 2 exacerbations of the disease over the past 2 years, followed by complete or incomplete recovery of the neurological deficit;
- secondary progressive multiple sclerosis with an active course of the disease, characterized by exacerbations or marked deterioration of neurological functions over the past 2 years - to reduce the frequency and severity of clinical exacerbations of the disease, as well as to slow down the rate of progression of the disease.
Use strictly as prescribed by your doctor.