MRI for traumatic brain injury Concussion is the most common type of traumatic brain injury (TBI). The organ does not undergo anatomical changes, and the neurological symptoms go away on their own. The diagnostic process includes questioning, examination and the use of instrumental methods. Performing magnetic resonance imaging if a concussion is suspected is unreasonable in the acute period. This is due to the fact that the considered variant of TBI is not accompanied by structural changes. An MRI after a suspected concussion will most reliably show the condition of the nervous tissue and promptly identify the presence of serious problems several weeks and even months after the injury. In the acute period, diagnosis does not make sense.
A concussion is considered a minor injury, accompanied only by disruption of brain function. A person may experience certain symptoms after an injury, including:
- short-term loss of consciousness;
- nausea;
- vomit;
- short-term amnesia (memory loss);
- sleep disturbance;
- headache, etc.
Loss of consciousness lasts from seconds to 5 minutes. The patient may not remember events that preceded the traumatic exposure (retro-) or occurred immediately after it (anterograde amnesia). However, all symptoms will go away in no more than 7 days. The main task of doctors in such a situation is not to miss dangerous injuries.
A brain contusion is a more severe injury. In this variant of TBI, morphological changes occur, cells are damaged and the connections of their processes (axons) may be disrupted, intracranial vessels rupture with the formation of hemorrhages and hematomas. When physical force is applied to the head, the nervous tissue receives two blows: the first - directly at the site of impact, the second - on the opposite side. The described phenomenon occurs due to the fact that the brain is injured from the inside by its own skull. The recovery period for a bruise may take more than one month, but a computed tomography scan will show the presence of this type of injury and will allow treatment to begin, and an MRI will reveal the consequences of a severe head injury after a while, helping to choose the right method of rehabilitation.
Subdural hematoma due to traumatic brain injury
Causes of cerebral contusion
A brain contusion is damage directly to brain tissue, which leads to the death of nerve cells. Can be unilateral or bilateral.
- Located both on the side of the damaged factor and on the opposite side
- The most common damage to the brain is caused by traumatic brain injury.
- Occurs as a result of a road traffic accident, beating, falling from a height, overturning heavy objects on the head, both at work and in everyday life, when falling from a height of one’s height during an epileptic attack or conditions accompanied by loss of consciousness (hypertensive, hypotonic crises, etc.).
- When an impact occurs, damage occurs to the structures of the brain, the vessels that feed them (as a result of the impact itself), as well as exposure to decay products of damaged cells.
The most common localization: fronto-occipital, occipital, parietal areas.
- When large vessels of the brain are damaged, intracerebral hemorrhage develops, which can lead to the formation of hematomas.
A distinction is made between mild, moderate and severe brain contusion, depending on the length of time the patient remains unconscious.
Brain contusion 1st degree (mild):
- occurs in 10-15% of cases of all traumatic brain injuries.
- loss of consciousness lasts from several minutes to tens of minutes from the moment of injury (in this case, headache, nausea, vomiting, increased blood pressure are observed)
Moderate brain contusion:
- occurs in 8-10% of victims
- from tens of minutes to hours (meningeal symptom complex, skull fracture is added)
Severe brain contusion:
- observed in 5-7% of patients
- from several hours to several weeks (the patient is in a coma)
Consequences of cerebral concussion
The consequences of brain contusion are extensive and depend on the severity. But even with a mild form with a fairly quick rehabilitation period, complications in the form of disturbances in the emotional sphere (irritability, psychosis) and the periodic occurrence of migraines cannot be excluded.
Post-traumatic syndrome after concussion may be delayed. Signs may take many months to appear, and sometimes begin during the early rehabilitation period.
Complications:
- Paralysis or paresis - the central gyri on the left side are damaged;
- Speech impairment – the source of damage is located in the frontal or temporal part;
- Hemorrhage;
- Hearing and vision impairment.
The consequences of a bruise inevitably occur after severe injuries. The person has difficulty restoring social adaptation, and psychosis or mental illness often develops.
Autonomic disorders persist for a long period (sweating, blood pressure, lethargy), migraine attacks cause irritability, and with excitement, a disturbance of the speech center may appear (in the form of stuttering). Phobias and epileptic seizures develop quite often.
Severe forms of bruises rarely lead to complete recovery and more often the victims become disabled. According to statistics, this form has high mortality rates.
Which method of diagnosing a brain contusion to choose: MRI or CT
Selection method:
- MSCT
What will CT images of the head show in case of brain contusion?
- Hypodense area in the acute stage, later - a hyperdense focus with a hypodense rim (perifocal edema)
- Size: from a few millimeters to several centimeters
- The presence of hemorrhage at the site of impact and hemorrhage due to the “counter-impact” mechanism, and the size of the latter may exceed the size of the hemorrhage at the site of application of the traumatic force
Volumetric effects may be observed depending on the size of the hemorrhage and the severity of edema:
- Swelling of the brain with loss of cortical definition.
- Displacement of midline structures.
- Compression of the ventricular system with impaired cerebrospinal fluid circulation.
- Compression of the surrounding tank.
Is MRI of the brain informative for concussion?
- Not indicated in acute cases
- High sensitivity in later stages of hemorrhages (subacute, chronic)
- Hypointense susceptibility artifacts on T2-weighted images
- The signal intensity on T1- and T2-weighted images corresponds to the intensity of the hemorrhage signal at the corresponding stage of the hemoglobin breakdown process
Hemorrhagic contusion in the superior frontal gyrus (24 hours after injury). CT, axial slice
Hemorrhagic contusion in both frontal lobes, 3 days old.
MRI T2*-WI (a) and T1-WI (b) in the axial plane. Lack of signal due to susceptibility artifact on T2*-weighted images (a). Hyperintense signal (methemoglobin) on T1-weighted image (b).
Clinical picture
In a complex wedge, a picture where symptoms and syndromes are closely intertwined, depending on concussion, contusion and compression of the brain, it seems possible to identify local symptoms of contusion or compression of the brain (see), which is of great practical importance. Symptoms of concussion (see) usually tend to quickly disappear, while symptoms of K. g. m. remain stationary or tend to progress from the 2-3rd day after the injury, and their regression is expected no earlier than with 2nd week after injury. The symptoms of K. g. m. and its dynamics are determined by the nature of the main lesion and perifocal phenomena, depending on the disturbance of blood and liquor circulation. When the central part of the contusion focus is located in functionally significant parts of the brain, persistent phenomena of prolapse usually remain. Perifocal changes are characterized by a later development and increase in symptoms, a short and complete regression in the recovery stage.
When the frontal lobes are damaged, psychopathol comes to the fore. symptoms with scarcity of purely neurol, symptoms. Sometimes lethargy and spontaneity against the background of other psychopathols, manifestations dominate the entire wedge, the picture of the first periods of the disease. There are unmotivated transitions from complacency and euphoria to attacks of rage, anger and discontent. In severe cases, persistent akinetic-amnestic syndrome manifests itself. When the premotor area is damaged, motor impairments are detected with loss of the ability to make fine differentiated movements. Roughly expressed pyramidal hemiparesis or hemiplegia appears only with massive damage to the frontoparietal region. Focal epileptic seizures, especially the Jacksonian type, in the acute period with brain contusion as a result of a closed skull injury are relatively rare and almost always indicate the presence of a local hematoma that must be removed. In the late period after injury, these seizures are common. With massive damage to the temporal lobe, diencephalic symptoms are almost always observed. These injuries often manifest themselves as violent motor excitation against the background of a general serious condition, upon exiting which more defined temporal symptoms are revealed. With severe lesions of the parietal-temporal region of the left hemisphere, aphasic, agnostic and apraxic disorders are identified (see Agnosia, Apraxia, Aphasia). With damage to the cortex of the temporal and inferior parietal lobes, disturbances in recognition, understanding of speech and writing, orientation in space and in one’s own body, psychosensory optical, vestibular, auditory, olfactory-gustatory and visceral disorders with derealization (see) and depersonalization (see) can be observed .). Contusions of the basal parts of the brain (hypothalamic-pituitary region and trunk) are clinically manifested by prolonged loss of consciousness and severe neurovegetative syndrome, the main components of which are respiratory disorders, cardiovascular activity, thermoregulation, as well as metabolic, humoral and endocrine disorders.
Symptoms
Brain contusion has three degrees of progression, with characteristic symptomatic manifestations:
- Easy. The victim may lose consciousness for a short time. After this, problems with hearing, orientation in space and time, weakness and drowsiness are noted. Such a patient has persistent headaches, nausea and dizziness, as well as vomiting. The patient may not remember events that occurred before the injury. After treatment, problems with remembering certain events are observed for a short time.
- Average. In this case, consciousness may not return to the victim for 5 hours. The patient exhibits cephalgia, vomiting, amnesia, spatial disorientation, mental disorders, tachycardia or bradycardia. In addition, speech is impaired, oculomotor deviations, partial paralysis, problems with muscle tone, and decreased or loss of sensitivity are observed. All symptoms go away in a month or a month and a half.
- Heavy. Unconsciousness can last up to two or more weeks. In terms of symptoms, a decrease in blood pressure, bradyarrhythmia, irregular breathing rhythm, slow movement of the eyeballs, ptosis of both eyelids, difficulty swallowing, and pathological reflexes in both feet are manifested. The patient experiences partial paralysis and loss of sensation, body temperature may rise, and convulsions appear.
In the case of severe changes in the brain area, the patient experiences persistent mental and neurological disorders.
The main difference between a concussion and a concussion is the presence of changes after injury in the cerebral tissues. An assessment of the degree of damage is given taking into account the disorder of consciousness in the victim, as well as the degree of neurological abnormalities and diagnostic data.
Symptoms of concussion
Signs of concussion are similar to those characteristic of a concussion. A person may begin to bleed from the nose and ears, and hearing and speech function sharply deteriorates. With correct, timely treatment, the disorders are reversible. The recovery period may vary.
Symptoms of contusion:
- Pain in the head, dizziness, which intensifies when performing rotational movements of the head.
- Nausea, attacks of vomiting.
- Amnesia of retrograde and anterograde types.
- Visual and speech dysfunction.
- Hearing impairment that develops as a result of barotrauma - damage to organs that occurs due to the difference in pressure inside the body and in the external environment.
- Increased sensitivity to noise and loud sounds.
When there is an amplitude difference between external and internal pressure due to an explosion, damage to the hearing organs in military personnel is often manifested by rupture of the membrane, decreased hearing acuity, and malfunction of the vestibular apparatus. The internal organs of the upper body are damaged due to compression between the spinal column, chest bones and diaphragm.
The consequences of concussion can last for a long period of time and are expressed in increased fatigue, irritability, epileptic seizures, insomnia, and poor health. In people who have suffered a bruise of brain tissue, alcohol tolerance worsens. The dose required for intoxication is significantly reduced.
Epilepsy
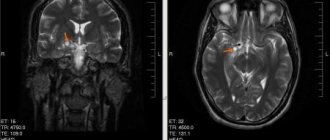
If epilepsy is suspected, MRI helps determine changes in the structure of the brain, as well as the source of the pathology. For example, in young children, the cause of epilepsy may be malformations of the brain, hemorrhages, or the consequences of intrauterine infections. In adults, epileptic seizures can be caused by:
- brain tumors;
- strokes;
- traumatic brain injuries;
- infectious and inflammatory diseases and complications after them;
- cortical dysgenesis;
- hippocampal sclerosis.
All of the above changes are diagnosed using MRI and allow you to confirm or refute epilepsy in the patient.
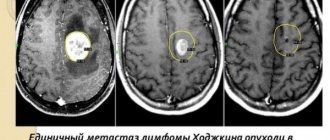
MRI will show oncology
If cancer is suspected, MRI provides the most complete and informative picture, since it allows you to see tumors even in the early stages. With MRI, brain tumors can be viewed in three planes. In addition, MRI is good at visualizing tumors located close to bone tissue, small tumors, and brain stem tumors.
Magnetic resonance imaging provides the widest possibilities for detecting metastases. The high sensitivity and information content of the method allows you to see the complete picture of the spread of metastases, and not just the focus. Brain metastases on MRI appear as limited, round-shaped formations.
First aid
Concussion of any severity requires emergency medical care.
The victim is given complete rest and prompt hospitalization. Before the ambulance arrives, the person must be placed on his side so that he does not choke on the vomit. The main helper for a shell-shocked person is cold. Place a wet towel or ice packs on your head to reduce pain.
If there is difficulty breathing or irregular pulse, the following actions are recommended::
- caffeine subcutaneously (1 ml solution);
- Cordiamine injection (1 ml intramuscularly or intravenously);
- injection of camphor extract (2-3 ml).
Performing direct cardiac massage through the chest is prohibited, as there is a high risk of subsequent organ injury. If there is no breathing, it is necessary to perform the “Mouth to Mouth” technique of stimulating the lungs. Before doing this, be sure to clear the victim’s mouth and nasal passages of soil or sand. You need to remove dirt from your mouth and throat using a clean finger, scarf or bandage.
Watch a video about first aid for cerebral contusion:
What can't be seen on an MRI?
MRI of the brain is effective in diagnosing many diseases of the central nervous system, but this research method is useless for determining some diseases. An MRI will not show cranial injuries or mental illnesses that do not cause physical changes in the brain.
MRI provides complete information about the state of the human brain. Due to its accuracy, safety and painlessness, the method is popular with both doctors and patients. When diagnosing some diseases, MRI is the only way to make a correct diagnosis. Tomographs are constantly being improved, which makes it possible to expand the list of diseases diagnosed with their help.
MRI for traumatic brain injuries
An MRI of the brain in case of a skull injury will allow you to determine the presence of damage and determine its type:
- brain contusion;
- diffuse axonal injury (DAI);
- intracranial hemorrhage;
- traumatic subarachnoid hemorrhage.
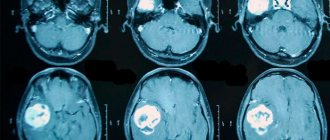
Brain contusion
A brain contusion is characterized by damage to the nervous tissue and the presence of a focus of necrosis, which is visible on MRI. Foci are of the following types:
- cytotoxic edema (type I contusion);
- infiltrative-gliotic changes and pinpoint petechial blood loss (type II contusion);
- a combination of edema and a hemorrhagic component in the form of intracerebral hematomas (type III contusion);
- intracerebral hematomas (type IV contusion).
All types of bruises are equally well diagnosed on MRI due to clear visualization of the lesions.
Diffuse axonal injury
DAP on MRI is visualized by an increase in brain volume, which occurs due to diffuse edema. Finely focal hemorrhages in the corpus callosum, brainstem and periventricular structures may also indicate DAP.
Intracranial hemorrhage
Intracranial hemorrhage contributes to the formation of a subdural, epidural or intracerebral hematoma. MRI helps determine the type of hematoma, its size and location. The subdural hematoma in the image has a crescent shape, the epidural hematoma is shaped like a biconcave lens, and the intracerebral hematoma is round in shape with an uneven contour.
Traumatic subarachnoid hemorrhage
Traumatic subarachnoid hemorrhage (TSH) is diagnosed using MRI several days after its occurrence. MRI allows you to determine the extent and location of hemorrhage.
Examples of common cases of acquisition of this injury
The list of common causes includes the consequences of road accidents, explosions, injuries at home, and falls. Concussion can also be caused by falling on water or during an epileptic attack.
During the war and due to explosions
The blast wave affects the entire body: from the back of the head to the feet.
The greatest harm is caused to the brain and nervous system. During an explosion, there is a sudden release of energy, which is explained by the property of gas to expand. The speed of shock wave propagation is greater than the speed of sound. The affected area from a shell or mine is several meters (the exact distance depends on the caliber). The wave from an atomic strike causes concussion in a person who is located a couple of kilometers from the source.
Because of the fall
In this situation, brain function is disrupted with obvious tissue changes. Disruptions occur in the process of inhibition and excitation. The subcortex and trunk suffer, vascular permeability increases. A person often loses consciousness (the duration of being unconscious depends on the height and severity of the fall).
Somatic causes
Brain contusion can develop even in the absence of damage to the brain . Dropsy, infectious and inflammatory processes in tissues, and disturbances in the composition of the cerebrospinal fluid lead to contusion.