Vascular dementia is an organic lesion of the brain. As a result of the pathological condition, a gradual defeat of higher mental functions occurs. As vascular dementia progresses, a person’s professional and social maladaptation develops. According to statistics, vascular dementia ranks second among all brain lesions accompanied by cognitive impairment. In the international classification of diseases, vascular dementia is coded F01. Depending on the location and etiological factor, the following are distinguished:
- F01.0 - dementia with acute onset;
- F01.1 - multi-infarction;
- F01.2 - subcortical;
- F01.3 - mixed;
- F01.8 - other;
- F01.9 - unspecified.
At the Yusupov Hospital you can undergo examination and receive quality treatment for vascular dementia. Consultations are conducted by experienced neurologists, psychotherapists, cardiologists and therapists. Thanks to modern medical equipment, it is possible to detect changes even in the early stages. This allows for timely treatment and a complete recovery.
Vascular genesis
Vascular genesis is not an independent disease, but only a consequence of the development of vascular diseases. The brain is supplied with nutrients and oxygen through blood, which flows through several arteries. In addition to the arteries, the venous system also plays an important role in transporting the required amount of blood to the brain. Vascular pathology, which entails negative changes in the blood supply system to the brain, is called “vascular genesis.”
Depending on the nature of the patient’s brain damage, they can diagnose:
- Organic or general pathological changes. They are quite often accompanied by severe headaches, including dizziness and nausea.
- Focal pathologies. If only certain areas of the brain are affected, patients will experience completely different signs of the disease. For example, with small focal leukoencephalopathy of vascular origin, the patient experiences damage to the white matter, which, in turn, leads to senile dementia.
Depending on the type of cerebral circulatory disorders, it is customary to distinguish:
- Transitory. In this case, it is customary to talk about general cerebral disorders or small-focal vascular disorders. The former cause severe headaches with nausea and even vomiting. The latter cause disruptions in the motor functions of organs, and sensitivity may be lost in certain parts of the body. This type of disorder is reversible and can be easily treated with complete recovery.
- Narrowing of the artery lumen. This pathology greatly affects the functioning of the area of the brain associated with this artery. Ischemic pathologies are often observed here. Treatment can be lengthy and complex, including surgical interventions.
- Aneurysm rupture. This process leads to hemorrhage into the brain cavity, the consequence of which will be a stroke, which can be hemorrhagic or ischemic in origin.
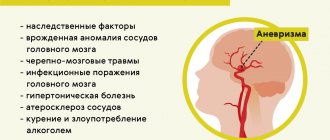
Reasons why vascular genesis of the brain develops
Considering that this pathology consists of insufficient blood supply to the brain, the doctor, in order to conduct effective treatment, is faced with the question of what led to the development of this disease. Most often, this situation is caused by hypertensive phenomena and the development of atherosclerosis of the vessels through which blood is delivered to the brain.
In the presence of hypertensive pathology, the patient develops thickening of the walls of blood vessels, which means that their lumen narrows significantly. In especially severe cases, sometimes complete stenosis of one or another vessel occurs, and the circulatory process can completely stop.
When the body is damaged by atherosclerosis, which, in turn, develops due to disruptions in the patient’s fat metabolism and the appearance of cholesterol deposits on the walls of blood vessels, normal blood flow becomes impossible. This leads to insufficient blood supply to the brain. In the most severe situations, due to the breakdown of cholesterol plaques, a blood clot can form in any of the blood vessels. It also usually causes blockage of the blood flow - complete or partial, thus creating foci of vascular origin.
In addition, other diseases lead to the development of vascular origin:
- aneurysm of the arteries supplying the brain;
- systemic diseases;
- pathological disruptions in the functioning of the heart;
- diabetes;
- anemia of any type;
- vegetative-vascular dystonia;
- osteochondrosis, leading to pinching of the paravertebral arteries.
The most common causes of these disturbances in the functioning of the body are:
- Constantly or frequently rising blood pressure;
- high blood glucose levels;
- head injury;
- psycho-emotional overload of the patient;
- bad habits - smoking, drinking alcoholic beverages in excess, overeating;
- disorders of the musculoskeletal system.
Sometimes disturbances in the blood supply to the brain occur as a result of improper functioning of the nervous and endocrine systems. Such disorders can occur with the development of chronic fatigue syndrome.
Causes
LNG can be caused by infectious diseases, the development of an inflammatory or malignant process, or systemic connective tissue diseases.
The most common reasons:
- infectious diseases - malaria, tuberculosis, aspergillosis, herpes, borreliosis, tick-borne encephalitis, abdominal-pelvic abscesses, prostate abscess, cholecystitis, dental infections, endocarditis, osteomyelitis, sinusitis, cytomegalovirus, Epstein-Barr virus, HIV, genitourinary infections, opportunistic infections ;
- autoimmune diseases - inflammatory bowel disease, rheumatoid arthritis, adult Still's disease, polymyalgia rheumatica, Reiter's syndrome, vasculitis, systemic lupus erythematosus, rheumatic fever;
- malignant tumors - renal cell carcinoma, hepatoma, colon cancer, pancreatic cancer, sarcomas, lymphomas, chronic leukemia, metastatic cancer.
Other reasons include:
- drug-induced fever (hypersensitivity reaction to certain medications);
- hepatitis (granulomatous, lupus, alcoholic);
- complications of liver cirrhosis;
- deep vein thrombosis;
- gout;
- Behçet's disease;
- Felty's syndrome;
- sarcoidosis;
- thyroiditis, Crohn's disease, familial periodic fever, cyclic neutropenia (rare).
Classification of the disease
In modern medicine, it is customary to distinguish the following types of insufficient blood supply to the brain:
- Binswanger's disease. This type of vascular circulation disorder leads to insufficient blood supply to the white matter of the brain. With this disease, the destruction of neurons occurs, which will soon lead to senile dementia - dementia. The first alarming symptom is severe pressure drops within one day. Then memory begins to deteriorate greatly.
- Pathological processes in the great vessels. Such disorders include narrowing of the lumens, strong bends, and thrombosis of blood vessels, which lead to a lack of circulating blood.
- Consequences of micro-strokes. When small vessels are blocked, there is a clear deterioration in the nutrition of the gray or white matter of the brain. This process cannot happen for a person without consequences. The patient may experience both general signs of the disease and disruptions only in certain body functions.
Signs of vascular origin
Manifestations of this disease at the first stage very rarely cause serious concern and seem to be a mild malaise against the background of fatigue or other illnesses.
First signs. Problems with the blood vessels of the brain most clearly begin to appear after increased emotional or physical activity. Also, prolonged exposure to a poorly ventilated room can trigger symptoms. The patient begins to feel:
- pain, noise and heaviness in the head;
- dizziness;
- sleep disturbance;
- high fatigue.
At this stage, an examination is usually started to exclude dystonia, neurosis or atherosclerosis. Only then will there be a suspicion of vascular genesis of the brain.
Mental disorders. Disorders of this type begin to appear only after a fairly long development of the disease. This can be expressed in the following manifestations:
- Increased irritability. This symptom is expressed in intolerance to loud sounds and bright lights.
- Deterioration of sleep. When the outflow of venous blood decreases, the patient develops prolonged and severe headaches. Dizziness is often observed, which intensifies with a sudden change in body position. Falling asleep takes a long time, and sleep time is very short - no more than four hours. This state of affairs leads to a deterioration in overall health and the development of chronic fatigue.
- Deterioration of mental functions. With prolonged circulatory failure in the white matter of the brain, the patient's memory and ability to purposefully plan begin to decline.
- Personal changes. As the disease progresses, the patient experiences a clear change in character. The main character traits begin to appear very strongly, and everything else gradually disappears. At this stage, a person develops very strong anxiety, suspiciousness and loses confidence in his actions.
With vascular genesis, all manifestations related to mental personality disorders are very treatable, which is clearly different from true mental illnesses.
Symptoms of diseases
Often, the primary symptoms of vascular origin appear after emotional, physical fatigue, as well as during prolonged stay in a poorly ventilated room. The patient complains of:
- Dizziness.
- Arrhythmia.
- Noise in ears.
- Heaviness in the head.
- Insomnia.
- Deterioration in concentration.
- Weakness in the limbs.
- Headache.
The nature of the headache depends on where exactly the focal brain lesion is located. With increasing ringing in the ears and a feeling of pulsation, we can talk about changes occurring in the craniocerebral arteries. Changes associated with greater filling of the cerebral veins are characterized by heaviness in the back of the head, morning headaches, and sleep disturbances. After waking up, the patient always feels heaviness and weakness throughout the body.
Other manifestations of vascular origin include:
- Mild mental disorders.
- Increased irritability.
- Memory impairment.
- Tearfulness.
Later, as the disease progresses, the following are added:
- Anxiety.
- Diffidence.
- Absent-mindedness.
- Unreasonable aggression.
After identifying the first alarming manifestations, it is necessary to seek medical help to exclude the development of atherosclerosis, neurosis, and vegetative-vascular dystonia.
Differences between headaches
As noted earlier, this disease is almost always accompanied by headache, which can vary significantly.
If the supply of arterial blood to the brain is disrupted, the pain occurs in a separate focus and is pulsating in nature with severe tinnitus. Gradually, the intensity of the pain attack decreases and turns into a dull, bursting pain.
In case of disturbances in venous blood flow, the patient experiences a dull heaviness throughout the head. The pain is clearly worse in the morning when standing upright or when coughing.
HEADACHE: PATHOGENETIC TYPES AND APPROACHES TO PATHOGENETIC PHARMACOTHERAPY
Since modern medicine does not have methods for objective verification of headaches, semiotics is of decisive importance in its diagnosis - a set of signs and features of the manifestation of subjective symptoms that the patient presents to the doctor in the form of complaints. Headache is a symptom, and therefore all attempts to classify it from a nosological position are baseless. At the same time, attempts at pathogenetic systematization and classification are certainly justified, since the identification of pathogenetic types of headache reveals approaches to the main directions of pathogenetic therapy. Experience shows that from a scientific and practical point of view, the following pathogenetic types of headaches can be distinguished: vascular, muscle tension, liquorodynamic, neuralgic and psychalgic. It should be emphasized that the names of these types are deliberately simplified so that the semantic content of these definitions is clear to doctors of different specialties. 1. Vascular type of headache
The vascular type of headache is associated with different types of craniocerebral arteriovenous dystonia. These variants of regional dystonia very often do not correlate with the main indicators of systemic hemodynamics. Arteriodilatatory (arteriohypotonic) variant of the vascular type of headache
associated with a decrease in the tone of the craniocerebral arteries.
This leads them to excessive stretching of the pulse volume of blood. Thus, the so-called pulsating headache is not a sign of vascular pain in general, but only of its arteriodilatatory variant. Excessive pulse stretching of the hypotonic arterial wall can occur even at normal levels of systemic arterial pressure, but more often when it increases. If the artery of the soft integument of the head is subjected to excessive pulse stretching (for example, the superficial, temporal artery), then compression of its adductor trunk in the temporomygomatic region with a finger can reduce throbbing pain. In some cases, the loss of autoregulation extends to arteriovenous shunts, which inappropriately expand, and then arterial blood, bypassing the capillary bed, enters the veins. Intravascular pressure, unusual for veins, adds to arterial pulsating pain a venous component that is uncharacteristic of venous pain itself. The extreme degree of arterial hypotension - paretic arterial dilatation (loss of arterial autoregulation) - is accompanied by impaired permeability and plasmatic saturation of the arterial wall, perivascular edema. Under these conditions, the amplitude of the pulsation decreases and the headache may lose its pulsating character. The throbbing pain gives way to a dull pain and becomes aching or bursting in nature. In the genesis of such pain, allogeneic vasoneuroactive substances take part, which, when permeability is impaired, penetrate into the vascular wall and perivascular tissue along with plasma. The arteriopathic variant of the vascular type of headache
occurs with “spasm” of the craniocerebral arteries.
From a practical point of view, by arterial “spasm” we can mean such a degree of increase in arterial tone that entails ischemic discirculation and ischemic hypoxia. In this case, the headache can be aching and dull in nature, perceived as a feeling of pressure, accompanied by lightheadedness, nausea, unsystematic dizziness, darkening in the eyes, “black spots” before the eyes. The venous variant of the vascular type of headache
(otherwise known as venous insufficiency headache) is caused by excessive blood filling of the venous vessels (veins and venous sinuses) and difficulty in venous outflow. Patients experience heaviness in the head and a feeling of dull fullness. In some cases, these sensations are limited to the occipital region, where the confluence of intracranial venous vessels is projected. However, due to multiple intracranial vein anastomoses, these sensations are usually generalized throughout the head. Venous outflow is more effective in a vertical position, when the direction of gravity (blood mass in the vessels) coincides with the direction of the venous outflow tract (jugular veins). Therefore, venous insufficiency headaches occur or worsen when lying down, working with the head bowed low, when straining or coughing. One of the characteristic symptoms of venous insufficiency headache is morning headache (“heavy head as soon as I opened my eyes in the morning”). Insufficiency of venous tone and venous outflow is confirmed by dilation of the veins of the fundus, cyanosis of the mucous membranes of the nose and oropharynx, pastiness of the face, in particular the eyelids (especially the lower ones). The nature of craniocerebral angiodystonia can be objectified using rheoencephalography (REG), the indicators of which reflect the state of the tone of the arteries and veins, as well as venous outflow. In order not to be mistaken in assessing these indicators and the role of certain changes in tone in the genesis of headaches, it is necessary to make at least two REG recordings - during a headache and during a period of well-being. It should be remembered that the increase in the tone of the craniocerebral arteries can be compensatory in nature and does not require correction with antispasmodics. To clarify the state of tone and determine the reactivity of the craniocerebral arteries, an REG is recorded with a pharmacological test (1/4-1/2 tablets of nitroglycerin under the tongue). To clarify the degree of venous insufficiency, REG is recorded in different body positions: sitting, lying (with and without a pillow), with the head lowered below the horizontal. Indirect information about the condition of intracranial vessels can be obtained by examining the arteries and veins of the fundus. The vascular type of headache is observed with migraine, regional craniocerebral form of vegetative-vascular dystonia, with arterial hypertension of various origins, including against the background of cerebral atherosclerosis, with systemic vasculitis. For the arteriohypotonic variant of the vascular type of headache, migraine attacks, ergotamine, dihydroergotamine, sumatriptan are prescribed, and for vegetovascular dystonia, xanthine drugs are prescribed: aminophylline, pentoxifylline, xanthinol nicotinate. For the arteriospastic variant, drugs that have an antispasmodic effect: phosphodiesterase inhibitors (papaverine, no-shpa), adenylate cyclase activators (vinpocetine and other Vinca minor drugs), a-adrenergic blockers (pirroxan, dihydroergotoxin, nicergoline), calcium antagonists (nifedipine, nimodipine) . For headaches of venous insufficiency, xanthine drugs are most effective. The effectiveness of pathogenetic treatment of vascular headache increases with adequate pharmacotherapy of the underlying disease. In cases where vascular headache is caused by a combined variant of arteriovenous craniocerebral dystonia, they try to isolate the key link in the pathogenesis and prescribe adequate therapy with appropriate vasoactive agents.
2. Muscle tension headache
Occurs when the muscles of the soft integument of the head are tense or compressed. Patients experience a sensation of the head being pulled together by a bandage or hoop. The pain can be local (forehead, crown, cervical-occipital region), but usually quickly generalizes, because the tension of one muscle is transmitted to other muscles through the tendon anoneurosis of the helmet. Tension headaches can occur in two ways. Firstly, under the action of central or systemic factors that facilitate and enhance transmission at the neuromuscular synapse, for example, stress during neurosis (“neurasthenic helmet”), or acting in a similar way, and humoral-hormonal changes (for example, in thyrotoxicosis), as well as during all cases of psychophysiological (psycho-emotional or psychophysical) failure in somatic diseases, especially with a progressive course (hypertension) or incomplete readaptation after somatic or infectious-toxic diseases, as well as after head injury. Another mechanism can be defined as segmental reflex, when tension in the muscles of the soft integument of the head occurs in response to pathological painful impulses during local processes (disease of the eyes, ears, paranasal cavities, cervical osteochondrosis). According to the traditional view, muscle tension headache is objectified by an increase in the potentials of electrical activity of the muscles of the soft integument of the head on the electromyogram. The debatable issue of the existence of tension headaches without tension of the head muscles will be considered when discussing the psychological type of headache. A muscle tension headache may be accompanied by a feeling of lightheadedness and unsystematic dizziness; patients find it unpleasant to comb their hair or wear a hat. The persistence of headaches makes patients irritable, they do not tolerate loud sounds, bright lights, memory and performance decrease. Pathogenetic treatment of pain of central origin includes tranquilizers and antidepressants. With segmental reflex genesis of pain, local methods of influence can play a significant role: lidocaine blockades, physiotherapy, acupuncture; and in the case of diseases of the eyes, paranasal cavities, ears - treatment of pathological processes that caused excessive painful impulses by the appropriate specialists: an ophthalmologist, an otolaryngologist.
3. Liquorodynamic type of headache
Cerebrospinal fluid (CSF) is produced by the choroid plexuses of the ventricles of the brain, circulates in the system of ventricles, cisterns and subarachnoid spaces, is absorbed by the villi of the pachyonic granulations and is sent further along the outflow tract into the venous system. The constancy of intraventricular, cisternal and subarachnoid cerebrospinal fluid pressure is ensured by the consistency of CSF production and outflow. CSF performs both the function of a fluid medium for brain metabolic processes and the mechanical function of a “cerebrospinal fluid cushion” that stabilizes the position of the brain within the strict confines of the intracranial space, limited by the bones of the skull and separated by the falciform process of the dura mater. Any pathological processes that disrupt the described dynamic balance of secretion and outflow, as well as the circulation of CSF, lead to either intracranial hypertension or intracranial hypotension. With increased intracranial pressure, the headache is bursting in nature, patients experience a feeling of pressure “from the inside to the outside,” “from the depths of the brain.” This pain intensifies with straining, coughing, sneezing and depends on the position of the body and head. All positions that impede the circulation of CSF worsen the headache. The rate of increase in liquorodynamic disturbances is also important. With a slow increase in intracranial pressure, adaptive and compensatory changes in the cerebrospinal fluid circulation are possible. Acute hydrocephalus always causes severe headache. CSF circulation disorders with increased intracranial pressure cause “space-occupying processes” that limit the intracranial space, such as tumors, parasitic and arachnoid cysts, brain abscess, cerebral edema due to trauma, inflammation or cerebrovascular accident. Volumetric intracranial processes (tumor, abscess, cyst) are often accompanied by the appearance of focal neurological symptoms, meningeal syndrome, vomiting, and impaired consciousness. Since these processes can cause a state of compression and/or dislocation of the brain that is incompatible with life, it is necessary to use neuroimaging methods - computed tomography (CT) and magnetic resonance imaging (MRI). Indirect signs of disturbances in intracranial pressure and CSF circulation can be obtained using radioisotope scintigraphy. A sign of increased intracranial pressure is venous congestion in the fundus and swelling of the optic nerve head. The dislocation of the middle structures is indicated by the displacement of the middle M-echo. The combination of these symptoms makes it possible to make a correct diagnosis and not be late in consulting the patient with a neurosurgeon to determine the indications and urgency of neurosurgical intervention. It should be remembered that if there is suspicion, and especially if there is objective evidence of displacement of the midline structures, it is unsafe to perform a lumbar puncture. Pharmacotherapy of intracranial hypertension includes dehydrating agents: osmotic diuretics - urea, manitool, sorbitol, glycerin (in the case of normal osmolarity); diuretics of another mechanism of action - furosemide, ethacrynic acid, hydrochlorothiazide, chlorthalidol, clopamide, potassium-sparing diuretics - triamterene, amiloride, spironoloctone. A decrease in intracranial pressure occurs as a result of a decrease in the production of CSF by the choroid plexuses of the ventricles and is accompanied by a dull generalized low-intensity but prolonged headache. Dysfunction of the choroid plexus occurs after a traumatic brain injury or an inflammatory process. The function of the CSF as a “liquor cushion” is lost. As a result, when the head moves or shakes it (for example, when walking), pain-sensitive intracranial structures - vessels, membranes, nerves - are stretched, and pain occurs, which intensifies in an upright position. Because this type of headache occurs after CSF is removed during a lumbar puncture, it is sometimes called a “drainage” headache. Sometimes the puncture site of the membranes after a lumbar puncture “does not close” and for some time CSF leaks through this hole, leading to a decrease in pressure. Drainage headaches are especially intense after a pneumoencephalographic contrast study with the extraction of a large amount of CSF and its replacement with air. Currently, due to poor tolerability, but mainly due to the introduction of CT and MRI into diagnostic practice, this method is not used. A decrease in CSF production can also occur in individuals with a long-term decrease in systemic blood pressure, for example, in patients with a hypotonic type of vegetative-vascular dystonia. If a decrease in systemic blood pressure is combined with hypotension of the cerebral arteries, then with reduced intracranial pressure the amplitude of the pulsation of the intracranial arteries may increase. Then the headache becomes throbbing. A decrease in CSF pressure is confirmed by lumbar puncture; other intracranial and cerebral disorders are clarified using CT and MRI. There are no drugs that could increase the production of CSF by the choroid plexuses of the ventricles. Therefore, indirect approaches can be proposed for treatment. Since the intracranial contents normally consist of the volumes of CSF, brain and intracranial blood supply (especially in the veins), with intracranial hypotension, bed rest is recommended, which increases blood supply, as well as drinking plenty of fluids with a higher than usual content of sodium chloride in food, which leads to a relative increase fluid-containing colloidal mass of the brain. To normalize liquor production, general restoratives and vitamin therapy are prescribed.
4. Neuralgic headache
As stated earlier, this type of pain is classified as facial pain (prosopalgia). They are distinguished by paroxysmal nature, with short paroxysms usually following each other, often causing the patient to suffer from neuralgia for hours or days. Pain, usually piercing, shooting, which, “like lightning” or “electric current”, strikes the patient. The second distinguishing feature is the presence of trigger or trigger zones, the irritation of which provokes an attack. The third characteristic sign is the irradiation of pain to neighboring or distant areas. It is believed that in most cases the cause of facial pain is a focus of pathological activity in the central structures of nociception related to the system of the trigeminal nerve and its central projections [just as the occurrence of an epileptic attack is explained by the presence of a focus (generator) of pathological activity in the systems that regulate the level of wakefulness and consciousness, or systems of motor activity]. For neuralgia of central origin, treatment with antiepileptic drugs, such as carbamazepine, is most effective. In some cases, neuralgia occurs when the sensory nerve is compressed through the mechanism of tunnel syndrome. It is precisely this mechanism that most often occurs with neuralgia of the occipital nerve, which is not included in the group of prosopalgia, but is cranial neuralgia. In these cases, in addition to antiepileptic drugs, they also resort to local effects: lidocaine blockades, physiotherapy, acupuncture.
5. Hallucinatory headache, or psychalgia
The traditional approach to the interpretation of visual or auditory hallucinations requires considering them as an objective sign of mental illness, although no morphological substrate in the form of damage to the structures of the visual or auditory analyzer is found. It is believed that the origin of hallucinations is associated with a neurotransmitter imbalance, leading to the emergence of a focus of pathological excitation in the system of a particular analyzer. A similar mechanism explains hallucinatory headaches that occur during the formation of a focus of pathological excitation (generator) in the central nociception system. Since this focus is formed in the system of structures of the central psycho-emotional perception of pain, the definition of “psychalgia” is applied to this type. It is very important to emphasize the difference between the definition of “psychogenic” (i.e., resulting from psychological stress) headache and the name “psychalgia”. Psychogenic, i.e. caused by stress, can be vascular, muscle tension headache, or neuralgic. And psychalgia itself can be psychogenic when it appears or intensifies after emotional stress. Many authors associate psychalgia with hidden (masked, larved) depression. Many patients with hidden depression complain of pain in the heart, stomach, intestines, etc., while in others hidden depression manifests itself as a headache. This projection of psychalgia onto the head area gave rise to another name - “conversion headache.” An important feature of psychalgia is the absence of specific physical characteristics in the patient’s description of the headache. Instead of specific definitions (for example, squeezing, bursting, pulsating), the patient resorts to vague metaphorical characteristics when describing pain. As a rule, when examined using instrumental methods, no pathology is found in such patients. To treat psychalgia, antidepressants, tranquilizers or antipsychotics are used. If a doctor, during dynamic observation of a patient and after conducting instrumental research methods, diagnoses hallucinatory psychalgia, then it is advisable to refer such a patient for observation to a psychiatrist, since most often the underlying disease is hidden depression.
6. Headache of mixed origin
Previously, different pathogenetic types of headaches in their “pure form” were given. However, we often deal with headaches of mixed origin. Even with migraine, a combination of different pathogenetic types can be observed: arteriohypotonic, venodystonic and muscle tension headache. Even more often, a combination of different headache mechanisms is observed in severe cerebral diseases: stroke, severe traumatic brain injury, meningoencephalitis. Of course, in these cases, the headache, although it requires pharmacological correction, recedes into the background before disorders that threaten the patient’s life. In such situations, the correct combination of symptomatic and nosological pathogenetic treatment is especially important. Summarizing the pathogenetic classification of headache, we consider it necessary to recall that headache is a symptom and as a symptom may not be indicated when formulating a detailed nosological diagnosis or appear in the background or third plan. At the same time, regardless of whether data on headache is included in the diagnosis, all data that allows one to establish the pathological type of headache must be included in medical documents - a medical history or an outpatient card.
Some controversial aspects
of the classification of headaches
As indicated, sharing the concept that a good classification should be based on one defining and dividing sign, in relation to the classification of headache as a symptom, we consider it adequate only to distinguish pathonetic types of headache. Classification according to nosological principle is impossible. All other attempts to group diseases that cause headaches are untenable. However, they have been and are being undertaken (1962 and 1988). Information about the classification of the International Classification Commission of Headaches of the International Headache Society was brought to the attention of neurologists in our country in the article by O.A. Kolosova and V.V. Osipova [1] and in the work of the chairman of this commission and the president of the European Federation of Neurological Societies J. Olesen [2]. The objectives of the article do not include a detailed analysis of the proposed classification. Nevertheless, neurologists in our country should be familiar with the proposals of the International Commission of Experts. The proposed classification divides headaches into 13 groups. Here is a list of these names: 1) migraine; 2) tension headache; 3) cluster headache; 4) various forms of headache not associated with structural lesions; 5) headache associated with head injury; 6) headache associated with vascular disorders; 7) headache associated with non-vascular intracranial disorders; headache associated with the use of certain substances or refusal to take them; 9) headache associated with extracerebral infection (i.e., a general infectious disease - author's note); 10) headache associated with metabolic disorders; 11) headache or facial pain associated with pathology of the skull, neck, eyes ,
2) tension headache; 3) cluster headache; 4) various forms of headache not associated with structural lesions; 5) headache associated with head injury; 6) headache associated with vascular disorders; 7) headache associated with non-vascular intracranial disorders; headache associated with the use of certain substances or refusal to take them; 9) headache associated with extracerebral infection (i.e., a general infectious disease - author's note); 10) headache associated with metabolic disorders; 11) headache or facial pain associated with pathology of the skull, neck, eyes ,
nose, sinuses, teeth, mouth or other facial structures;
12) cranial neuralgia, neuropathy and disafferentation pain; 13) unclassifiable headache. We cannot agree that this list of diseases and conditions can be accepted as a classification of headaches. J. Olesen writes that the first four groups can be classified as primary headaches. In our opinion, only points 1 and 3 can be definitely attributed to primary headache. Point 2 cannot be included regardless of approaches and predilections to interpretations of genesis and names. If we use the previous term “muscle tension headache,” then the headache is secondary either to neurosis or to local pathological processes in the head area. If we use the new term “tension headache,” then it is secondary to depression (or, again, to neurosis). The names of other groups are extremely vague and cannot be considered classification. We believe that the doctor’s thought should follow from the patient’s complaints to establishing the pathogenetic type of headache, from the type of headache to important accompanying symptoms, from the symptom complex that characterizes not only the headache, but the disease as a whole, to the nosological diagnosis of the underlying disease. We wrote about this back in 1987 [3]. The authors who took the trouble to introduce our neurologists to the international classification did not provide the full title of the work of the International Commission either in the title or in the text of their articles, but it reads like this: “Classification and diagnostic criteria for headaches, cranial neuralgia and facial pain.” Therefore, if the division into 13 groups cannot be accepted as a classification, this division and especially the explanation for it can only be considered as a diagnostic algorithm that can be used in the transition from establishing the pathogenetic type of headache to establishing a nosological diagnosis. It is important to understand that the same pathogenetic type of headache can be observed in different diseases and, conversely, with the same disease, the same patient may experience headaches of different pathogenetic types. An example is hypertension. Classics of Russian medicine G.F. Lang and A.L. Myasnikov perfectly described the types of headaches associated with hypertension: neurasthenic, vascular, “typical,” and toxic. From the point of view of our presentation, neurasthenic is a headache of muscle tension, vascular is arteriohypotonic, “typical” is a headache of venous insufficiency, toxic is liquorodynamic. In other words, the essence is the same, the names are simply clarified from the point of view of pathogenesis. Thus, the same patient at different stages of the disease may have a headache of one or another pathogenetic type. Or another example: cervical osteochondrosis. The same patient may have muscle tension headache, occipital neuralgia, headache of vascular origin as part of the posterior cervical sympathetic syndrome (Barre-Lieu vertebral artery syndrome).
Literature:
1. Kolosova O.A., Osipova V.V. Classification of headaches // Journal. neurology and psychiatry named after. S.S. Korsakova, 1996, No. 3, p. 8-11. 2. Olesen J. Diagnosis of headache // Neurological Journal, 1996, No. 3, p. 4-11. 3. Shtok V.N. Headache. M.: Medicine, 1987, 303 p. 4. Classification Committee of International Headache Society. Classification and Diagnostic Criteria for headache disorders, cranial neuralgia and facial pain. Cephalgia 1988;8(Suppl.1.7):1-96.
Diagnosis of the disease
This disease is extremely difficult to diagnose in the early stages, especially with single changes in the brain. Quite often, during examination, doctors do not find any significant deviations from the norm. But if there are obvious disturbances in your well-being, you should not calm down. It is necessary to continue further, more detailed examination.
Survey forms:
- computed tomography makes it possible to examine vessels for the presence of congenital or acquired vascular pathologies;
- Magnetic resonance imaging makes it possible to get a complete picture of the condition of blood vessels;
- magnetic resonance angiography is performed to determine the state of the gray matter and the presence of small focal changes in the brain of vascular origin;
- Dopplerography is carried out to clarify the speed of blood flow;
- electroencephalography diagnoses the structure of the brain of a sick person;
- spectroscopy allows you to analyze processes (biochemical) in brain tissue.
If the patient has obvious functional disorders of other organs, he is referred to other specialists for consultation. For example, if vision deteriorates, the patient is referred to an ophthalmologist.
When conducting any type of examination, if there is a suspicion of this disease, the patient is also prescribed a detailed examination of cardiac activity.
Diagnostics
It can be difficult to detect that the brain is receiving little nutrition and to determine changes in vascular origin at the initial stage, since in a given state of the body the electrocardiogram can be completely normal, without any abnormalities. But an ECG during physical activity can reflect changes that are present in the human body. It is also recommended to install a 24-hour monitor so that the doctor can see the work of the heart. But it is worth saying that these types of diagnostics may not show that some kind of malfunction is occurring in the body, for example, a single focus of vascular origin.
Treatment options
If the patient has very pronounced disorders in the functioning of the brain listed earlier, then he should be hospitalized as soon as possible. All treatment procedures in this case will be aimed at quickly eliminating high intracranial pressure, as well as eliminating the consequences of stroke or atherosclerosis. In the latter case, when blood flow stops due to the appearance of plaques in the lumens of blood vessels, surgical intervention is often used, aimed at removing completely blocked or severely affected areas of the vessels. During the rehabilitation period, patients are prescribed therapeutic exercises and a strict low-lipid diet.
In situations where there are obvious symptoms of insufficient brain nutrition, but surgical intervention is not necessary, patients are prescribed drug therapy:
- drugs aimed at thinning the blood (anticoagulants);
- medicines to eliminate vasospasm and restore normal blood circulation;
- blood pressure lowering agents;
- drugs that improve intercellular metabolism, as well as help the formation of a new vascular network.
All manifestations of vascular origin go away quite quickly after the underlying disease is eliminated. But people with such problems require constant monitoring. Vascular genesis, unfortunately, can progress quite quickly and cause significant damage to the patient’s psyche, and the consequences can be very serious.
Impaired blood supply to the brain
The main causes of malnutrition are hypertension and atherosclerosis. The first named disease is quite common. This disease affects both men and women. Often the origins of hypertension are unknown. But it can cause a person to be diagnosed with vascular genesis. The essence of hypertension is that the walls of blood vessels become denser, and the channel through which blood flows narrows. Sometimes complete narrowing occurs. In this case, the passage of blood becomes impossible. Next, vascular genesis of the brain occurs. What this is, we described above.
Atherosclerosis is associated with lipid metabolism disorders. Due to increased levels of cholesterol in the blood and other fat-containing substances, deposits form in the blood vessels. They interfere with normal blood circulation. Its movement is hampered by the fact that plaques form in the vessels over time due to lipids. First, they clog blood vessels. Then they begin to fall apart. Their particles are carried with the blood to other small vessels. As a result, they can cause blockages.
Also, a disease such as osteochondrosis can affect the blood supply to the brain. Since the movement of intervertebral discs can lead to pinched arteries. Thus, brain nutrition will deteriorate.
Preventive actions
Preventive actions aimed at reducing the risk of developing cerebrovascular diseases should be aimed at preventing any vascular disease that, as it progresses, leads to impaired cerebral circulation.
Basic measures that a potential patient can take:
- rational alternation of work and rest;
- good physical activity corresponding to general physical condition;
- following a diet if there is a risk of developing atherosclerosis, diabetes and heart disease;
- strict blood pressure control;
- regular preventive examinations.
All recommended activities are very easy to implement, but you should remember that taking your daily well-being seriously is the key to a long and fulfilling life.