Neuralgia refers to severe shooting pain that occurs due to a damaged or irritated nerve. Neuralgia can affect any part of the body, causing mild to severe pain. Certain medications and surgical procedures can effectively treat neuralgia.
Severe neuralgia can affect a person's ability to perform everyday tasks and can affect their quality of life.
Neuralgia has many possible causes, including:
- infections such as shingles, Lyme disease, or HIV
- pressure on bone nerves, blood vessels or tumors
- other medical conditions such as kidney disease or diabetes
- aging
This article examines the different types of neuralgia, their symptoms, and available treatment options.
Types of neuralgia
Medical professionals divide neuralgia into categories based on the areas of the body that it affects. The following are some common types of neuralgia :
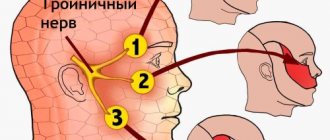
Trigeminal neuralgia
TN can cause shooting pain in the face.
Trigeminal neuralgia (TN) involves the trigeminal nerve in the head. It has three branches that send signals from the brain to the face, mouth, teeth and nose.
TN is divided into two divisions: type 1 and type 2.
Type 1 TN causes a painful burning or electric shock sensation in some parts of the face. People with type 1 TN experience irregular episodes that come on suddenly.
The duration of these episodes varies among individuals, but can last up to 2 minutes, according to the National Institute of Neurological Disorders and Stroke.
Type 2 TN produces a constant, dull, aching sensation on the face.
The exact cause of TN remains unclear. However, pressure from the enlarged blood vessel can irritate or even damage the trigeminal nerve.
Multiple sclerosis (MS) can lead to TN. MS is a neurological disorder that causes inflammation that damages the myelin sheath surrounding nerve fibers in the central nervous system.
Postherpetic neuralgia
Postherpetic neuralgia (PHN) is a painful condition that affects the nerves of the skin.
According to the Centers for Disease Control and Prevention (CDC), PHN is the most common complication of shingles, affecting about 10–13% of people who develop it.
Shingles is a viral infection that causes blisters and a painful skin rash. The varicella zoster virus, which causes chickenpox, remains dormant in the nervous system and becomes active later in life, causing shingles.
When the virus is reactivated, it can cause inflammation of nerve fibers. This inflammation can lead to permanent nerve damage, which causes pain even after the infection subsides.
Occipital neuralgia
This form of neuralgia affects the occipital nerves, which originate in the neck and send signals to the back of the head.
Occipital neuralgia causes throbbing or shooting pain that begins at the base of the skull and spreads along the scalp. Pain in occipital neuralgia may flow to the back of the eyes.
Occipital neuralgia has many potential causes, including:
- sudden head movements
- tense neck muscles
- lesions or tumors in the neck
- inflamed blood vessels
- infections
- gout
- diabetes
- neck injuries
Peripheral neuralgia
Peripheral neuralgia, or peripheral neuropathy, refers to pain that occurs due to nerve damage in the peripheral nervous system. This includes all nerve fibers outside the brain and spinal cord.
Peripheral neuralgia can affect one nerve or entire nerve groups.
Sustained damage to the peripheral nervous system can affect the nerves that control muscle movement, transmit sensory information, and regulate internal organs.
Peripheral neuralgia can cause pain or numbness in the arms, legs, arms and legs. Other symptoms may include:
- involuntary muscle twitching or spasms
- loss of coordination
- difficulty performing complex motor tasks such as buttoning a shirt or tying shoelaces
- hypersensitivity to touch or temperature
- excessive sweating
- gastrointestinal problems
- difficulty eating or swallowing
- it's hard to talk
Intercostal neuralgia
Intercostal neuralgia affects the nerves that sit just below the ribs. Doctors call the muscles in this area the intercostal muscles.
Several potential factors may contribute to intercostal neuralgia, such as:
- injuries or surgical procedures involving the chest
- pressure on the nerves
- shingles or other viral infections
Intercostal neuralgia causes sharp, burning pain that affects the chest wall, upper abdomen, and upper back. Certain physical movements, such as breathing, coughing, or laughing, can make the pain worse.
Additional symptoms may include:
- tightness or pressure that envelops the chest
- tingling or numbness in the upper chest or upper back
- muscle twitching
- loss of appetite
Diabetic neuropathy
Diabetic neuropathy is the most common complication of diabetes. Because diabetes affects so many people, rates of peripheral neuropathy are now starting to rise.
Symptoms include loss of balance and numbness, tingling and pain. The best way to prevent diabetic neuropathy is to keep your blood sugar levels within an acceptable range.
Diagnosis of intercostal neuralgia
Diagnosis of intercostal neuralgia is quite difficult, since it must be differentiated from a number of diseases that have similar symptoms. A cardiologist or pulmonologist may be involved in the diagnostic process. Specialists at the CELT Pain Clinic conduct an examination and collect anamnesis, and also determine the presence or absence of the disease in the following ways:
- chest x-ray;
- CT scan;
- myelography;
- Magnetic resonance imaging;
- spondylography;
- electro- and echocardiography;
- examination of the gastrointestinal tract.
If diagnostic studies do not reveal diseases of the lungs, gastrointestinal tract and cardiovascular system, the patient is referred to a neurologist who develops a treatment plan.
Treatment of neuralgia
Treatment options for neuralgia vary depending on the type and severity of the condition.
Ointments, local nerve blocks, and steroid injections may provide temporary pain relief for mild neuralgia.
Treatment for severe neuralgia pain may require prescription drugs, surgical procedures, or both.
Medications
Painkillers are generally not very effective in controlling neuralgia pain. Medications that can treat the underlying causes of neuralgia include :
- anticonvulsants such as carbamazepine, topiramate, and lamotrigine
- antidepressants such as amitriptyline
- muscle relaxants such as baclofen
- membrane stabilizing drugs such as gabapentin
Causes of intercostal neuralgia
The main causes of intercostal neuralgia are as follows:
- a number of diseases of the nervous system: multiple sclerosis, polyradiculoneuritis;
- diseases of the thoracic spine: deforming spondylosis, osteochondrosis, herniated disc, scoliosis;
- hypothermia of the body;
- intoxication of the body with alcohol, medications, salts of heavy metals;
- back and sternum injuries;
- weakening of the immune system;
- lungs' cancer.
Surgery
Certain surgical procedures can help relieve neuralgia pain when the condition does not respond to treatment.
Examples of surgical procedures that may help treat neuralgia include:
Microvascular decompression : Helps remove an enlarged blood vessel affecting a nerve. The procedure involves placing a soft pad between the blood vessel and the affected nerve.
Stereotactic surgery : This is a non-invasive procedure that directs highly concentrated beams into the root of the damaged nerve. The radiation disrupts the transmission of pain signals to the brain.
Percutaneous balloon compression : This involves inserting a small balloon into the affected nerve. The balloon is inflated, causing controlled, deliberate nerve damage. This procedure prevents the affected nerve from sending pain signals to the brain. However, the effects of the procedure usually wear off after 1-2 years.
Causes
The immediate cause of pain is pressure on the nerve fiber due to swelling or deformed muscle tissue.
This can occur with the following pathologies:
- various diseases of the spinal column - developmental anomalies, traumatic deformities, intervertebral hernias, osteochondrosis;
- benign and malignant tumors, cysts in the area of nerve fibers;
- infectious damage to the nerve fiber - tuberculosis, herpetic;
- intoxication - salts of heavy metals, alkaloids;
- inflammatory process in the nerve fiber itself;
- vitamin deficiency, especially B vitamins;
- metabolic diseases - diabetes;
- alcoholism and drug addiction;
- chronic diseases accompanied by severe hypoxia - atherosclerosis, respiratory failure;
- endocrine pathologies.
Clinical manifestations of neuralgia
The following symptoms are characteristic of trigeminal neuralgia:
- attacks of severe pain;
- increased pain during any actions with the mouth (chewing, opening, etc.);
- facial distortion;
- concentration of pain in the eyes, ears, teeth, mouth;
- teak.
Trigeminal facial neuralgia is characterized by attacks of stabbing, cutting, pulling pain lasting up to 1 minute. In the vast majority of cases, one side of the face is affected, but there are cases when pathological processes spread to the entire face. Painful sensations can be projected into the teeth and can cause the removal of a completely healthy tooth.
Symptoms
The clinical picture that accompanies muscular neuralgia will allow the neurologist to determine the focus of pathological processes and the stage of their development. The symptoms of the disease depend on the location of the muscle damage.
| Name | Symptoms |
| Intercostal neuralgia |
|
| Neuralgia of the sciatic muscle | Pathological processes often occur against the background of damage to the spinal column in the lumbar region. Provoking factors include tumor, injury, hypothermia or heavy physical exertion. Symptoms of sciatic neuralgia are as follows:
|
| Trigeminal neuralgia | The pathological condition is more often diagnosed in women over 40 years of age. Symptoms of trigeminal neuralgia are as follows:
|
| Neuralgia of the occipital region | Pathological processes often provoke osteochondrosis, gout, and tumor. Due to the high mobility of the spinal column in the occipital area, muscular neuralgia occurs even in a healthy person. Inflammation or pinching of the occipital nerve can also be triggered by a draft, hypothermia, or sudden head movements. Symptoms of the pathological condition are as follows:
|
| Postherpetic neuralgia | A special form of muscular neuralgia of infectious origin. Pathological processes are provoked by chicken pox. Postherpetic muscular neuralgia is often diagnosed in people who have weak immunity, severe illness, or immunodeficiency disorders. Symptoms of the pathological condition are as follows:
|
| Damage to facial muscles | Muscular neuralgia of the face manifests itself in most cases only on one side.
|
In any situation, a consultation with a neurologist is necessary, since pathological processes arise for certain reasons, they must be identified correctly and in a timely manner.
Principles of treatment
Muscular neuralgia can be treated with medications and non-drug methods. The drugs are usually used to relieve an acute attack. All other methods are aimed at preventing their occurrence.
Non-drug therapy
Includes a large number of methods:
- physical therapy complexes that involve problem areas of the body;
- acupuncture courses;
- kinesitherapy;
- massage of problem areas;
- use of a magnet, electrophoresis, Darsonval currents;
- physical exercises - swimming, race walking, yoga.
Non-drug therapy can be used continuously. It allows you to reduce the number and intensity of attacks.
Medications
Prescribed to reduce pain. Various groups of drugs are used. Tablet forms are used, since external ones have little effect - they are not able to affect the damaged nerve.
- Non-steroidal anti-inflammatory drugs - reduce swelling in the area of the damaged nerve, reduce pain. Such drugs include Ketonal, Nimesil. They should be taken with caution, as they can provoke the development of stomach ulcers.
- Muscle relaxants - these drugs help relax muscle tissue and reduce pain intensity. These include Sirdalud, Relpax.
- Antispasmodics - have an effect similar to muscle relaxants, but have a weaker effect. To a greater extent they affect the smooth muscles of internal organs.
- For trigeminal neuralgia and herpetic lesions, antiepileptic drugs are prescribed, which can also relieve neurogenic pain. These include Finlepsin, Catena.
- To restore nerve conduction, B vitamins are indicated. Their best absorption is observed when administered by injection. Combination drugs are usually prescribed - Milgamma, Combilipen.
All drugs are prescribed not individually, but in the form of various combinations. In case of severe pain, blockade of the exit points of nerve fibers is indicated. Analgesics such as Lidocaine and Ultracaine are used for them.
Muscular neuralgia is rarely completely cured; it is usually a chronic disease. Treatment can reduce the number of attacks and extend the time without pain.
Treatment of lesions of the facial or trigeminal nerve
The first thing to do (if the cause of the lesion is not known) is to undergo a full diagnosis and find out why this problem occurred. This will allow the doctor to choose the right treatment tactics.
It is very important to consult a doctor as soon as possible if you experience the first symptoms of complications after tooth extraction or implant installation. If treatment is started promptly, complete restoration of muscle functionality can be achieved. It is also important that if numbness persists for 3 months and no measures have been taken, it will most likely not be possible to restore the affected nerve, since persistent degenerative changes develop in it.
Diagnostics
- a blood test to check for a viral or bacterial infection that could cause nerve damage,
- CT or MRI of the skull and brain to determine the affected area,
- electromyography, which involves direct impact on nerve endings to determine the level of disturbance in the passage of impulses along the nerve.
Treatment
- drug therapy: this group includes anti-inflammatory, painkillers and anticonvulsants, as well as antidepressants and sedatives.
- physiotherapy: facial gymnastics, massage performed by specialists, electrical stimulation and acupuncture,
- microsurgery: surgery is performed to restore the integrity of the damaged nerve. This is a fairly serious surgical procedure that should be performed by a professional surgeon. Surgery is an extreme method of solving the problem; it is needed only in case of serious damage and if the first two options did not bring any result.